The concept that challenging life events have the potential to facilitate positive change has been explored for centuries in the areas of philosophy, theology, and the arts. However, scientific examination of stress-related growth (SRG) started in the 1990s (posttraumatic growth [PTG], thriving, finding benefits, adversarial growth) (
20–
24). Research over the past half-century has also established that high levels of stress increase risk for development of both psychiatric and medical conditions (
25). The growing recognition that individual outcomes following exposures to challenging events are quite diverse (i.e., ranging from highly detrimental to highly beneficial) led to the development of resilience as a broader framework (
5,
7,
26–
28). In this context, resilience is conceptualized as a dynamic multifactorial process presenting multiple possibilities for improving outcomes (e.g., SRG)
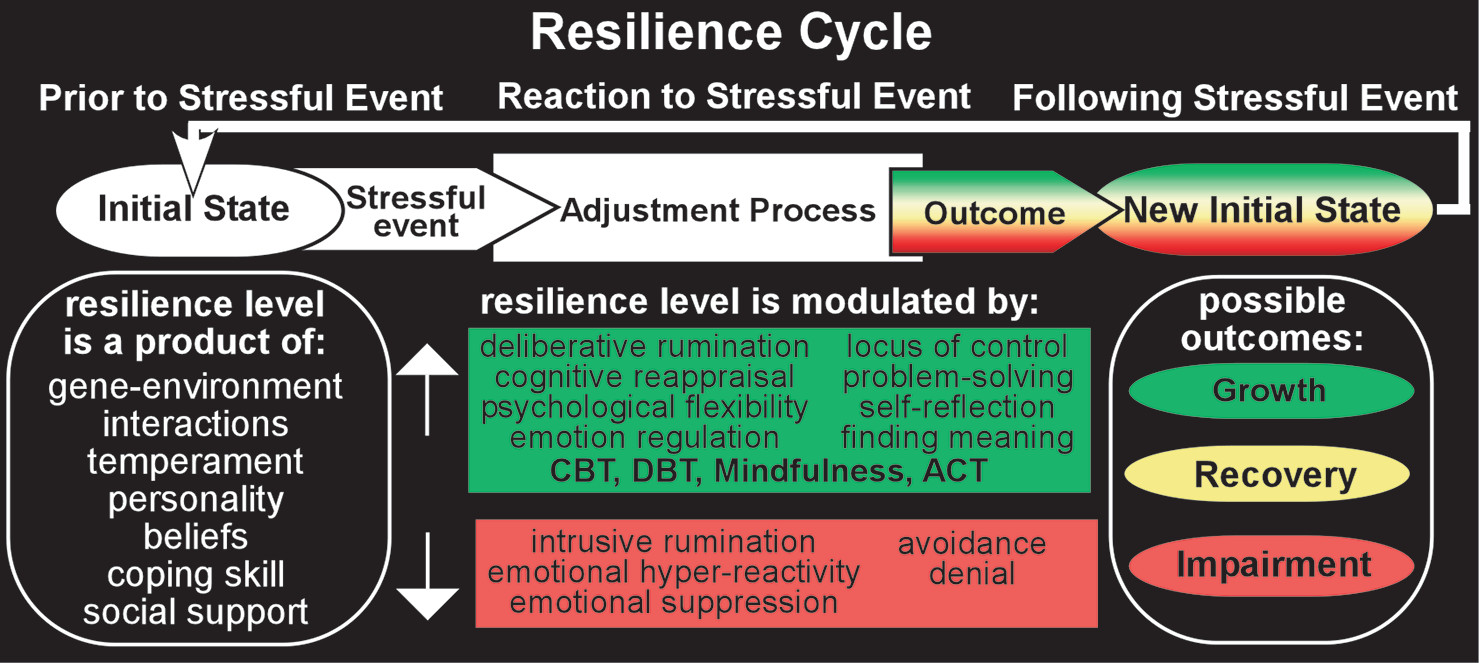
The resilience cycle (
Figure 1) encompasses ongoing interactions among a complex array of biological (e.g., genetic, epigenetic), neuropsychological (e.g., cognitive, emotional), and environmental (e.g., social, economic, and cultural) factors that affect how an individual responds to a particular stressful experience (
3–
9,
26–
30). A resilient (hardy) individual maintains an adaptive level of physiological and psychological functioning when challenged by events. Multiple types of evidence support the importance of moderately stressful events (tolerable stress) for increasing an individual’s level of resilience (stress inoculation, tempering, steeling, adversity-driven resilience) (
1–
5,
7). Events that induce little or no stress do not provide a resilience-building experience. Events that induce very high levels of stress may overwhelm an individual’s coping capacity, at least temporarily (toxic stress). It should be noted that SRG has been identified not only in relation to stressful or traumatic external events but also in relation to recovery from serious mental illness (
31,
32). A personal account of recovery from psychosis noting psychological growth following several psychotic episodes suggested that opportunities for growth (e.g., intentional introspection, meaning making, benefit finding, and positive self-disclosure) should be intentionally incorporated into treatment and recovery plans (
32).
Although most research to date has focused on the construct of posttraumatic growth, this is only one aspect of a rather complex and multifaceted phenomenon of positive adaptation and development following events that are perceived as distressing regardless of valence (
4,
28). An emerging body of literature indicates that growth is not limited to situations and events that have negative valence and that psychological growth may occur following any event that challenges an individual’s coping resources. A recent meta-analysis of longitudinal studies examining the effects of life events on psychological well-being reported a positive trend for self-esteem, positive relationships, and mastery following both positive and negative events, with no general evidence that negative life events had a stronger effect (
33). Additionally, they found that in studies utilizing control groups, results did not significantly differ between the event and control groups, indicating that changes in outcome variables cannot necessarily be attributed to the reported life events.
Multiple conceptual models for adaptive coping with adversity and fostering resilience and growth have been proposed (e.g., PTG, coping circumplex model, systematic self-reflection, cognitive appraisal of resilience, cognitive growth, and stress) (
4,
9–
11,
34). All include an aspect of cognitive flexibility (e.g., cognitive processing, cognitive appraisal, rumination, problem-solving, meaning making, benefit finding, and self-reflection) as a primary mechanism for strengthening resilience after exposure to life stressors that require adaptation (i.e., psychological adjustment through the process of redefinition of the self and reappraisal of one’s beliefs). Several models include emotion regulation as the second key aspect of resilience (
4,
9,
11). Recent reviews on the neurobiology of resilience converge on the central importance of the prefrontal cortex (PFC)-limbic circuitry (
5–
7,
35–
37). Higher resilience is associated with greater emotion regulation capacity (i.e., top-down regulation of emotional responses). Greater engagement of PFC areas important for cognitive and emotional control enhances inhibition of limbic areas such as the amygdala, reducing reactivity to stressful stimuli. Resilience-related differences in resting-state EEG have also been reported. A study of children that compared groups with and without maltreatment reported greater relative left central activity (lower left compared with right alpha power) in high-resilience (composite index of adaptive functioning) individuals from both groups, whereas low resilience was associated with greater right hemisphere activity (
38). A study of middle-aged adults reported that higher right frontal activity was associated with increased levels of blood biomarkers (interleukin-6, C-reactive protein, and fibrinogen) indicating low-grade inflammation only in the group who reported having experienced moderate to severe abuse as children (Childhood Trauma Questionnaire) (
39). As discussed by the authors, these results are consistent with higher right frontal activity indicating greater vulnerability to emotionally challenging stressors (diathesis-stress model) and that this may also increase risk for inflammation-related medical conditions.
Both cognitive and emotional approaches to coping with adversity span a wide range of strategies, some of which are detrimental to functioning. For example, rumination (repetitive thinking about an event) can be either deliberate or intrusive (
40,
41). Deliberate (reflective) ruminations are adaptive, voluntary purposeful thoughts focused on better understanding of the event (i.e., its meaning, consequences, and implications). Additionally, deliberate rumination may serve as a coping strategy for managing emotional responses. Intrusive (perseverative) ruminations (e.g., worry, brooding) are maladaptive, automatic unwanted thoughts or memories that increase an individual’s distress. Intrusive rumination may also involve attempts to suppress thoughts about a stressful event. As would be expected, research indicates that intrusive and deliberate ruminations play very different roles in outcomes (
41). Recent longitudinal and cross-sectional studies in a wide range of trauma-exposed groups (e.g., middle school and college students, military veterans, emergency services personnel, cancer survivors, and patients with nervous system injuries) indicate that intrusive rumination is positively associated with psychiatric symptoms, whereas deliberative rumination is positively associated with SRG (
10,
42–
49). As noted in several studies, these results support the potential of interventions facilitating deliberative rumination during recovery to promote better outcomes. Similarly, emotional coping may be positive and lead to emotional equilibrium (i.e., adequate emotional control), or it may be negative and result in emotional disequilibrium (e.g., emotional hyperreactivity, excessive anxiety, and suppressing emotions). These concepts are consistent with the broader body of literature that has demonstrated associations between emotion dysregulation and various forms of psychopathology (
50). Studies identifying specific capacities or skills associated with higher resilience and/or better recovery from challenging events provide potential targets for interventions.
Interventions that promote cognitive flexibility and/or emotion regulation would be expected to strengthen resilience. Cognitive restructuring is one of the primary techniques utilized in cognitive-behavioral therapy (CBT), which involves identifying and challenging negative and rigid thought patterns (
51,
52). The goal is to facilitate resilience rather than to solve a particular problem or achieve a certain outcome, as illustrated in a recent study of patients with posttraumatic stress disorder (PTSD) comparing CBT with eye movement desensitization and reprocessing therapy (
53). There were no differences in clinical efficacy, but only CBT improved general life functioning (Work and Social Adjustment Scale). Acceptance and commitment therapy (ACT) is a transdiagnostic approach that has the primary focus of fostering psychological flexibility as a pathway toward adaptation and psychological well-being (
54,
55). Recent systematic reviews and meta-analyses of randomized controlled trials of interventions that included therapeutic mindfulness (e.g., ACT, mindfulness-based stress reduction, mindfulness-based cognitive therapy) reported beneficial effects on a wide range of behavioral health outcomes (e.g., anxiety, depression, fatigue, stress, quality of life, and PTG) in adults with cancer (
56,
57). Mindfulness-based interventions have also been shown to decrease use of maladaptive coping strategies (e.g., avoidance or disengagement coping, negative emotional coping) (
58,
59). Dialectical-behavior therapy (DBT) may also be a useful therapeutic approach to facilitate emotion regulation, because it incorporates mindfulness, emphasizes the role of difficulties in emotion regulation, and focuses on the development of emotion-regulation skills (
60–
62). DBT has been shown to be effective in decreasing transdiagnostic emotion dysregulation (
63–
65). Overall, meta-analyses and systematic reviews of various psychosocial interventions generally show that interventions based on principles of CBT and mindfulness have the strongest effect sizes in fostering resilience and psychological growth following adverse events (
66,
67). Imaging studies comparing pretreatment to posttreatment resting-state and/or task-activated functional MRI (fMRI) have reported changes in brain activation patterns following treatments that correlate with symptom improvements, suggesting beneficial neuroplastic processes (
53,
68–
72).
Whether self-reported growth following challenging events is primarily positive is a matter of considerable debate (
34,
73–
81). A key problem with research in this area is reliance on retrospective reports of self-perceived growth that may not represent genuine transformation (
76,
79,
82–
86). The few longitudinal studies indicate that self-perceived growth does not correlate with more objective measures of psychological growth (i.e., measures of actual psychological resources) (
82,
85,
87,
88). In addition, a longitudinal study assessing veterans decades after their participation in the Yom Kippur War found that self-reported growth was linked with several detrimental outcomes, including higher rates of loneliness and lower dyadic adjustment in marital relationships (
78,
80). The authors suggested that self-perceived growth may be better described as a set of defensive beliefs, a potentially maladaptive strategy for coping with distress. The Janus Face model encompasses this dichotomy by proposing that self-perceived growth following traumatic events has both a functional or constructive side and an illusory (e.g., self-deceptive or dysfunctional) side that may coexist (
89,
90). The constructive side is correlated with healthy adjustment, whereas the illusory side is correlated with denial. Similarly, other studies have concluded that self-reported growth can indicate an adaptive outcome of successful cognitive coping or a positive illusion that is a result of avoidance and denial (
76,
91). However, the question remains whether self-perception of growth may be beneficial to individuals even if it does not reflect measurable change. On one hand, illusory perceptions (i.e., beliefs that are not grounded in reality) are generally considered maladaptive. On the other hand, some studies have demonstrated that even perceptions of positive change may be linked with more adaptive coping (i.e., positive reinterpretation), better mental health (e.g., lower symptoms of anxiety and depression, higher stress tolerance), and increased quality of life (
74,
77,
92–
94). Thus, illusory or self-deceptive growth is not always associated with maladjustment. If illusory perceptions of growth coexist with and do not hinder active coping (e.g., deliberate ruminations), then they may serve as a short-term adaptive palliative coping strategy helping individuals deal effectively with the aftermath of distressing events (
83,
90,
95).
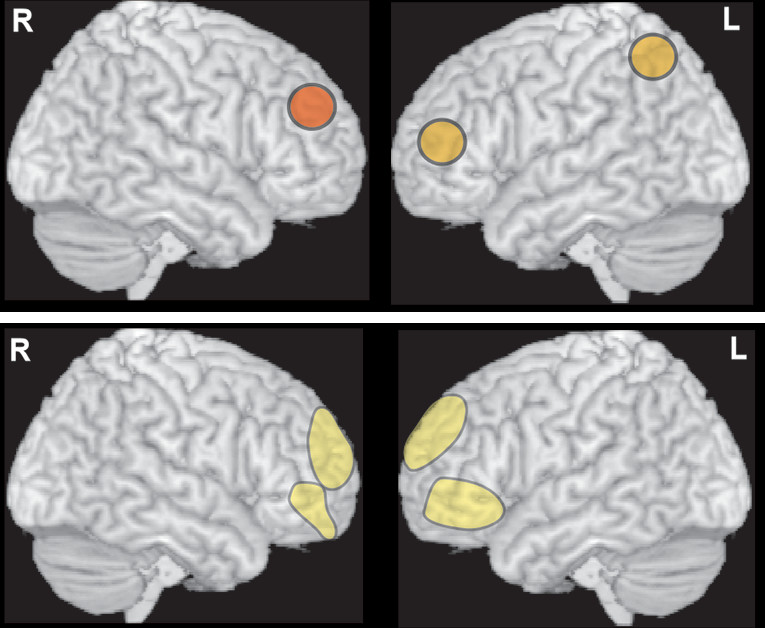
Most research on the neurobiological correlates of SRG has also utilized self-report questionnaires (e.g., the Post Traumatic Growth Index [PTGI]) that assess retrospective perception of change. Several studies have reported correlations between PTGI scores and imaging metrics within the dorsolateral PFC (
Figure 2) (
13–
15). A study of healthy adults utilizing group spatial independent component analysis of resting-state fMRI reported a positive correlation between PTGI scores and higher resting-activity level in two left hemisphere areas that are part of the central executive network (dorsolateral PFC, superior parietal lobule) (
13). A longitudinal MRI study of healthy young adults identified changes in regional gray matter volume (whole brain voxel-based morphometry) between images acquired prior to and 3 months after they experienced the East Japan Great Earthquake (
14). PTGI scores were positively and significantly associated only with change in the right dorsolateral PFC (
14). In the region of interest analysis, PTGI scores were positively correlated, whereas posttraumatic stress symptoms (Clinician-Administered PTSD Scale [CAPS]) were negatively correlated with changes in gray matter volume in the same area. As noted by the authors, individuals with low PTGI scores had reduced volume in this area, suggesting that the direction of volumetric changes may indicate adaptive versus maladaptive responses to stress (
14). Congruent with this hypothesis, an earlier longitudinal MRI study that compared patients with PTSD and healthy individuals reported that at the earliest imaging time point (average of 1.42 years since the trauma), the PTSD group had greater cortical thickness within portions of dorsolateral PFC bilaterally (
Figure 2) (
15). Greater cortical thickness was positively correlated with better performance on tests of executive functioning in the PTSD group. It also correlated with greater symptom reduction (CAPS score) during the previous year and by the final time point (average of 3.85 years since the trauma). Cortical thickness had normalized by the final time point, and cortical thinning correlated with symptom resolution, indicating a role for dorsolateral PFC in supporting recovery from PTSD (
15).
As detailed in recent reviews, an individual’s ability to dismiss unwanted memories when they intrude into conscious awareness is an important aspect of healthy emotion regulation that may be modifiable (
16,
17). This capacity is experimentally assessed by pairing items to be remembered with reminder cues and comparing results when participants are instructed to recall (Think) or instructed to not recall (NoThink) the paired items when cued. Participants also report whether a memory intrusion occurred during the NoThink condition. In healthy individuals, suppression of an intrusive memory decreases the frequency of subsequent intrusions and weakens (as indexed by decreased priming effects) the memory trace (suppression-induced forgetting, motivated forgetting, adaptive forgetting, beneficial forgetting, and selective forgetting). Recent studies of suppression-induced forgetting provide evidence that both explicit and implicit memory traces are affected (
96,
97). Ability to suppress intrusions varies considerably across healthy individuals, and lower ability has been associated with higher maladaptive traits (e.g., anxiety, brooding) (
17). A study of college students found that higher ability was associated with higher trauma exposure, suggesting the possibility that this capacity may be increased by successfully coping with moderate levels of adversity (
16,
17). Impaired ability to suppress intrusive memories on this task has been reported for multiple psychiatric disorders, including PTSD (
16,
17).
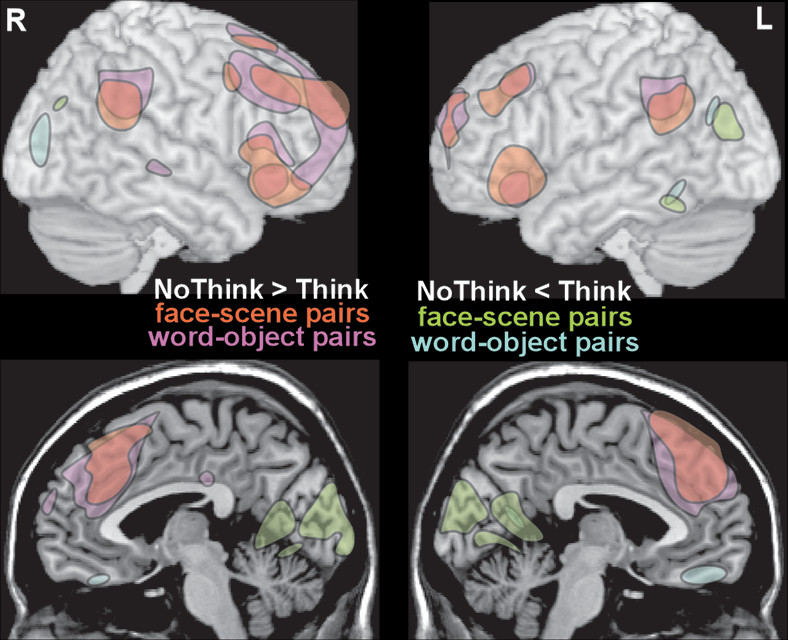
Cross-sectional fMRI studies of healthy individuals performing the Think/NoThink task have reported that memory suppression is associated with increased activation (NoThink >Think) in frontal and parietal cortices and decreased activation (NoThink <Think) in memory-related areas (e.g., hippocampus, memory-associated domain-specific cortical areas) (
Figure 3) (
16,
18,
19). An fMRI study that utilized unpleasant images demonstrated that an area in the right dorsolateral PFC exerted parallel top-down inhibition of the hippocampus and domain-specific areas (e.g., amygdala, sensory cortices) (
18). Effective connectivity analyses indicated that intrusion of memory into awareness in the NoThink condition, which triggers increased effort to dismiss the memory, was associated with increased top-down inhibition (i.e., increased negative coupling with the right dorsolateral PFC). Greater success at suppressing intrusive memories (i.e., higher memory control) was associated with reduced intrusion frequency and reduced memory-associated negative emotion, indicating weakening of both episodic and emotional memory traces (
18). An fMRI study that compared trauma-exposed individuals (in the Paris terrorist attacks) with and without PTSD to unexposed individuals on this task reported that all three groups improved on suppression with practice (fewer intrusions during NoThink trials) to a similar extent (
19). However, the PTSD group differed from the trauma-exposed without PTSD and unexposed groups on functional metrics. The PTSD group had neither the robust decrease in memory strength for NoThink items (i.e., decreased priming effect indicating weakening of memory traces) nor the increase in top-down inhibition (i.e., increased negative coupling between the right dorsolateral PFC and areas important for memory such as the hippocampus) during suppression of intrusive memories seen in the other groups. As discussed by the authors, these findings indicate an impairment in memory regulation in the PTSD group that may be the reason memory intrusions are so persistent (
19). Multiple authors have noted that results from this task suggest that it may be time to re-examine the common belief that all forms of memory suppression are maladaptive (
16–
19,
97).
In conclusion, recent studies are contributing a new understanding of adaptive and maladaptive stress-related changes in the brain, resilience, and to the neuroplastic changes underlying SRG. This understanding offers promising evidence for recovery following even serious adversities and psychological traumas.