Co-occurring psychiatric disorders are widely prevalent in populations with Tourette syndrome (TS). Eighty-five percent of individuals with TS have at least one comorbid psychiatric disorder during their lifetime, and 58% have two or more (
1). For many individuals with TS, these co-occurring psychiatric conditions are more distressing and impairing than tics (
2). The most common co-occurring psychiatric diagnoses among those with TS are attention-deficit hyperactivity disorder (ADHD), obsessive-compulsive disorder (OCD), anxiety disorders, and mood disorders, with lifetime prevalence rates of 54%, 50%, 36%, and 30%, respectively (
1). Many individuals with TS who do not fulfill formal diagnostic criteria for these comorbid psychiatric conditions still exhibit subthreshold symptoms of the disorders (
3,
4). Given the high prevalence of ADHD, OCD, anxiety disorders and mood disorders and their strong association with poor quality of life in TS populations (
2,
5–
7), clinical practice guidelines for TS recommend routine assessment for these disorders (
8,
9).
Co-occurring psychiatric symptoms in TS exhibit distinct clinical trajectories. ADHD symptoms often arise in early childhood (median age at onset: 5 years old), typically preceding onset of tics (median age at onset: 6 years old) (
1). OCD and anxiety symptoms generally emerge slightly later in childhood (median age at onset: 7 years old) (
1), and depressive symptoms often first manifest in adolescence (median age at onset: 13 years old) (
1). For the majority of individuals with TS, tics, ADHD symptoms, and OCD symptoms improve during late adolescence (
10). In contrast, depression and anxiety become increasingly evident throughout adolescence and adulthood (
1). In one of the largest studies of comorbid psychiatric conditions in TS to date (N=1,374 patients), lifetime prevalence of mood disorders was 16% in children, 33% in adolescents, and 60% in adults (
1). Similarly, lifetime prevalence of anxiety disorders in this sample increased with age, from 25% in childhood to 29% in adolescence to 39% in adulthood (
1). In clinical samples of adults with TS, 20%–45% have elevated scores on depression rating scales relative to general population norms (
3,
5,
11), and nearly 70% have elevated scores on anxiety rating scales (
11). Moreover, while depression and anxiety are associated with poor quality of life in TS populations of all ages, these associations are strongest in adulthood (
2). In fact, among adults with TS, quality of life more closely correlates with severity of depressive (
5–
7) and anxiety (
6,
7) symptoms than with severity of tics, ADHD symptoms, or OCD symptoms.
Thus, previous studies suggest the psychiatric profile of TS evolves over the course of development: during the transition from childhood to adulthood, the severity of tics, OCD symptoms, and ADHD symptoms decrease, and the severity of depressive and anxiety symptoms increase. Within the extant literature on depression and anxiety in adults with TS, however, important limitations and knowledge gaps are evident. First, many studies of adults with TS investigated mood and anxiety disorders as categorical rather than dimensional constructs (
1,
4,
11). Categorical approaches assume that psychiatric disorders are either present or absent, neglecting the clinical continuum that exists above and below diagnostic thresholds (
12,
13). As emphasized in the Research Domain Criteria framework proposed by the National Institute of Mental Health, dimensional approaches may facilitate deeper insights into the clinical features and neurobiological bases of mental disorders (
12–
14). Second, of the studies that did adopt a dimensional approach in their evaluation of adults with TS, the majority focused on depression and its association with a specific clinical domain of interest (e.g., quality of life [
7,
11,
15], tic severity [
7,
16], OCD severity [
7], and ADHD diagnosis [
17]) without accounting for anxiety or other common co-occurring psychiatric symptoms. Third, most studies evaluating depression and anxiety in adults with TS did not perform between-sex comparisons of these dimensions (
4,
11,
16–
18), despite mounting evidence of phenotypic differences between men and women with TS (
19–
22).
To begin addressing the above knowledge gaps, we conducted a single-center, retrospective chart review of a clinical population of adults with TS and other chronic tic disorders, systematically analyzing clinical information and psychiatric symptom rating scale data collected during routine care. The aims of the study were to determine the prevalence and severity of depressive and anxiety symptoms in a treatment-seeking cohort of adults with chronic tic disorder using a dimensional approach and to determine the relationship of depressive and anxiety symptom severity with other clinical characteristics, including sex, age, tic severity, ADHD symptom severity, and OCD symptom severity. We hypothesized that depressive and anxiety symptom severity would be significantly elevated in adults with chronic tic disorder compared with normative populations and that depressive and anxiety symptom severity would be more strongly associated with ADHD and OCD symptom severity than with tic severity.
Methods
Population
Since December 2020, all new and returning patients presenting to Vanderbilt’s Adult Tourette Syndrome Clinic complete previsit self-report scales assessing depressive, anxiety, ADHD, and OCD symptoms. The same movement disorders neurologist (D.I.) evaluates each patient in this clinic and administers the Yale Global Tic Severity Scale (YGTSS) during the clinic visit (
23,
24). Data from patients who fulfilled the following eligibility criteria were included in the present analysis: attended our clinic between December 2020 and July 2022; diagnosis of TS, chronic motor tic disorder, or chronic vocal tic disorder based on DSM-5 criteria; age 18 years or older; ability to complete self-report scales unaided; and English fluency. Given evidence that TS, chronic motor tic disorder, and chronic vocal tic disorder exist along a single clinical continuum (
25), these three DSM-5 tic disorders were studied collectively as chronic tic disorder. The Vanderbilt Institutional Review Board approved this study in accordance with all applicable international guidelines and laws.
Rating Scales
The self-report scales administered to all patients prior to their clinic appointment included the Quality of Life in Neurological Disorders (Neuro-QoL) Depression Short Form, version 1.0 (Neuro-QoL Depression); the Neuro-QoL Anxiety Short Form, version 1.0 (Neuro-QoL Anxiety); the Adult ADHD Self-Report Screening Scale for DSM-5 (ASRS-5); and the Dimensional Obsessive-Compulsive Scale (DOCS). A brief summary of scale properties is provided below, with additional details provided in Table S1 in the online supplement.
The Neuro-QoL measures were developed as part of the National Institute of Neurological Disorders and Stroke initiative to create psychometrically rigorous quality-of-life scales for individuals with neurological disorders (
26). Both Neuro-QoL Depression and Neuro-QoL Anxiety are eight-item self-report questionnaires. Individual items are statements concerning depressive or anxiety symptoms, respectively, in reference to the previous 7 days, to which respondents rate their agreement on a 5-point Likert scale. For each measure, individual item scores are summed to generate the raw total score, which is then converted to a T-score. A T-score of 50 represents the mean from a large community-reference population (N=2,113 adults). T-scores above 50 indicate greater severity of the given construct in the sample population relative to the reference population. A 10-point T-score interval is equivalent to one standard deviation in the reference population score. Neuro-QoL Depression and Neuro-QoL Anxiety have demonstrated excellent internal reliability (Cronbach’s alpha coefficient >0.90) in the general population (
26) and in several neurological populations (
27,
28).
The ASRS-5 is a six-item self-report scale in which respondents rate their agreement with statements concerning ADHD symptoms over the previous 6 months using a 5-point Likert scale (
29). The DOCS is a 20-item self-report scale in which the severity of a respondent’s OCD symptoms over the previous month are quantified via answers to multiple-choice questions (
30). The YGTSS is the gold-standard, clinician-administered, semistructured interview for assessing tic severity (
23). From the YGTSS interview, two separate scores are generated: a total tic severity score and a tic impairment score. Besides the YGTSS, patients do not undergo formal structured or semistructured psychiatric interviews as part of routine care in our clinic.
Data Collection
A systematic chart review was conducted for all patients who presented to the clinic between December 2020 and July 2022. The electronic medical record of study-eligible patients was reviewed for the following information: age at time of visit; sex; self-reported age at tic onset; prescribed medications at time of visit; chronic tic disorder diagnosis; and history of select psychiatric diagnoses, including ADHD, OCD, any anxiety disorder, any mood disorder, any psychotic disorder, and autism spectrum disorder. Additionally, individual item scores and total scores for Neuro-QoL Depression, Neuro-QoL Anxiety, ASRS-5, DOCS, and YGTSS were collected. For subjects with multiple visits during this time period, we used data from the earliest visit in which all scales were completed.
Statistical Analysis
One hundred twenty-nine patients met study eligibility criteria. Nine of these patients had no self-report scale data available in the electronic medical record. Therefore, 120 patients were included in the final data set for analysis. Neuro-QoL Depression and Neuro-QoL Anxiety scores were available for 119 patients. ASRS-5 and DOCS scores were available for 119 and 118 patients, respectively. For patients missing individual item responses from Neuro-QoL Depression (N=1 patient), Neuro-QoL Anxiety (N=1), or DOCS (N=1), missing responses were imputed from mean nonmissing responses, and total scores were generated by summing nonmissing responses with this imputed item value. One patient did not complete any ASRS-5 or DOCS items; for this patient, total scores on these two scales were imputed from mean nonmissing total scores. YGTSS items were complete for all patients.
To examine the internal reliability of the self-report scales, we computed Cronbach’s alpha and McDonald’s omega coefficients (
31). The latter coefficient is an estimate of internal reliability that is robust to violation of the tau-equivalence assumption and thus is generally more appropriate than Cronbach’s alpha for psychological self-report scales (
31). We also examined known-groups validity of self-report scales by comparing relevant scale scores between patient subgroups stratified by the presence or absence of documented mood, anxiety, ADHD, and OCD diagnoses. Wilcoxon rank-sum tests were used for these between-group contrasts.
Medians and interquartile ranges were calculated for all continuous variables. Between-sex contrasts were conducted with Wilcoxon rank-sum tests for continuous variables and Fisher’s exact tests for dichotomous variables. We used the one-sample Wilcoxon signed-rank test to evaluate whether the T-scores for Neuro-QoL Depression and Neuro-QoL Anxiety in the sample population differed from the reference population mean T-score of 50. We conducted this test for the entire cohort and then separately for men and women in the cohort.
To examine the relationships between continuous variables, we computed Spearman rank correlations, adjusting the significance threshold with a procedure to control the false discovery rate and account for multiple comparisons (
32). For the correlation analyses, we used Neuro-QoL Depression and Neuro-QoL Anxiety raw scores, rather than T-scores, because T-scores incorporate information about the reference population that is extraneous for within-group analyses.
To determine the clinical variables most strongly associated with Neuro-QoL Depression scores, we performed a multivariable linear regression analysis. As with the correlation analysis, Neuro-QoL raw scores, rather than T-scores, were used. We first constructed a base model with square-root Neuro-QoL Depression raw score as the dependent variable and the following as independent variables: sex, age, Neuro-QoL Anxiety raw score, ASRS-5 score, and DOCS score (model 1; see Table S5 in the online supplement). Square-root Neuro-QoL Depression raw score was used rather than Neuro-QoL Depression raw score because the latter exhibited significant heteroskedasticity. Next, we constructed two models expanded from model 1: one model incorporated interaction terms of sex with each independent variable (model 2), and the other model incorporated interaction terms of age with each independent variable (model 3). Lastly, we constructed a model (model 4) consisting of the model 1 independent variables as well as the interaction terms that were significantly associated with the dependent variable in models 2 or 3. For each model, we plotted histograms of residuals to visually examine for deviations from normality, plotted residuals against the dependent variable to visually examine for heteroskedasticity, computed the Breusch-Pagan test statistic to quantify heteroskedasticity, and computed the variance inflation factor for independent variables to quantify degree of multicollinearity. To compare goodness of fit between model 1 and the other models, we used likelihood-ratio tests, adjusted R2 values, and Akaike information criteria (AIC). To assess the association between each independent variable and the dependent variable within a given model, we conducted post hoc t tests with a prespecified significance threshold of p<0.05.
To determine the clinical variables most strongly associated with Neuro-QoL Anxiety scores, we performed a multivariable linear regression analysis using the same model construction and diagnostic approach outlined above. For the base model, Neuro-QoL Anxiety raw score was the dependent variable, and the following were independent variables: sex, age, Neuro-QoL Depression raw score, ASRS-5 score, and DOCS score (model 5; see Table S5 in the online supplement). Sex and age interaction terms were inserted for models 6 and 7, respectively, and the final model (model 8) consisted of the independent variables from model 5 as well as the interaction terms that were significantly associated with the dependent variable in model 6 or 7.
Statistical analyses were conducted with Stata 15.0 and Excel 16.5.
Results
Between December 2020 and July 2022, 195 patients attended our clinic, of whom 129 met study eligibility criteria. Nine of the eligible patients had no self-report scale scores in their electronic medical records. Thus, the final data set for analysis included data from 120 patients. Details on ineligible patients are provided in Table S2 in the online supplement.
Our cohort was comparable to other clinical samples of adults with chronic tic disorder in terms of age at tic onset (
1,
3,
4,
11,
21,
33), sex distribution (
3,
4,
7,
17,
21), and prevalence of mood and anxiety disorders (
1) (
Table 1). The prevalence of comorbid ADHD and OCD in our cohort was lower than that in samples of patients with chronic tic disorder who are prospectively assessed for these disorders with structured diagnostic interviews (
1). The number of lifetime psychiatric diagnoses in our cohort aligned with previous studies: 87% of patients had a prior diagnosis of at least one of the six comorbid psychiatric disorders listed in
Table 1, and more than 60% of patients had two or more comorbid conditions (
1).
Internal reliability and known-groups validity for the self-report measures are presented in Table S4 in the
online supplement. Neuro-QoL Depression T-scores for the entire cohort, for men in the cohort, and for women in the cohort did not significantly differ from 50. Based on proposed Neuro-QoL T-score cut points (
34), depressive symptom severity was mild (score of 55–60) in 18 patients, moderate (60–70) in 13 patients, and severe (>70) in no patient. Neuro-QoL Anxiety T-scores were significantly higher than 50 for the entire cohort (p<0.001), for men in the cohort (p<0.001), and for women in the cohort (p<0.001). Based on the above Neuro-QoL cut points, anxiety symptom severity was mild in 31 patients, moderate in 44 patients, and severe in four patients.
Women had significantly higher YGTSS impairment scores and Neuro-QoL Anxiety scores than men (
Table 2). There were no significant sex differences on any other rating scale scores. Women were more likely to have a history of anxiety disorder, based on chart review.
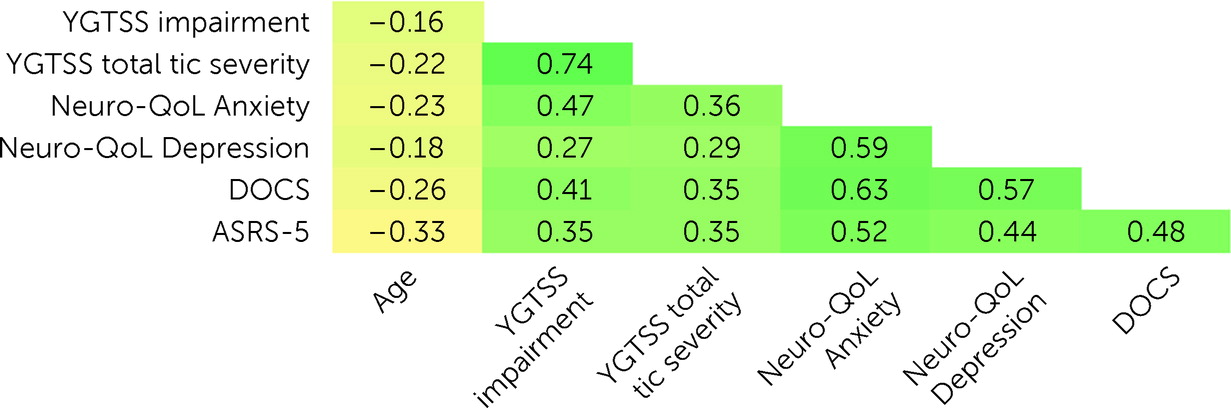
All tested correlations were significant except for the correlation between age and YGTSS impairment score (
Figure 1). Age was negatively correlated with all rating scale scores; all other correlations were positive in direction. Neuro-QoL Depression raw scores were most strongly correlated with Neuro-QoL Anxiety raw scores and DOCS scores, followed by ASRS-5 scores, YGTSS total tic severity scores, and YGTSS impairment scores. Neuro-QoL Anxiety raw scores were most strongly correlated with DOCS scores and Neuro-QoL Depression raw scores, followed by ASRS-5 scores, YGTSS impairment scores, and YGTSS total tic severity scores.
Regression analysis results for the best-fitting models are provided in
Table 3. Comprehensive details on all constructed models are provided in Table S5 in the
online supplement. Of the models with square-root Neuro-QoL Depression raw score as the dependent variable, model 4 provided the best goodness of fit, as evidenced by its higher adjusted R
2 value, lower AIC value, and significantly large likelihood-ratio test statistic. Independent variables in model 4 collectively explained 42% of the variance in square-root Neuro-QoL Depression raw scores. After adjusting for covariates, square-root Neuro-QoL Depression raw scores were significantly associated with sex, Neuro-QoL Anxiety raw scores, DOCS scores, and the age×DOCS score interaction term; these findings indicated that greater depressive symptom severity was associated with male sex, greater anxiety symptom severity, and greater OCD symptom severity, although the strength of the association between OCD and depressive symptom severity diminished with age. Neither YGTSS total tic severity scores nor ASRS-5 scores were significantly associated with square-root Neuro-QoL Depression raw scores.
Of the models with Neuro-QoL Anxiety raw score as the dependent variable, model 8 provided the best goodness of fit, as evidenced by its higher adjusted R2 value, lower AIC value, and significantly large likelihood-ratio test statistic. Independent variables in model 8 collectively explained 55% of the variance in Neuro-QoL Anxiety raw scores. After adjustment for covariates, Neuro-QoL Anxiety raw scores were significantly associated with Neuro-QoL Depression raw scores, DOCS scores, and the sex×ASRS-5 score interaction term; these findings indicated that greater anxiety symptom severity was associated with greater depressive and OCD symptom severity and that the association between anxiety and ADHD symptom severity was stronger among women than men. YGTSS total tic severity scores were not significantly associated with Neuro-QoL Anxiety raw scores.
Discussion
In this study of depressive and anxiety symptoms in a clinical sample of adults with chronic tic disorder, we identified several novel findings. First, anxiety symptoms were more prevalent and severe than depressive symptoms in this population. Second, depressive and anxiety symptom severity were more closely associated with each other and with OCD symptom severity than with tic severity. Third, sex is an important consideration in investigations of depression and anxiety among adults with chronic tic disorder. These findings will be discussed sequentially.
Contrary to our a priori hypothesis and the findings from several previous studies (
16,
18,
35), depressive symptom severity in our cohort of adults with chronic tic disorder was not significantly greater than population norms. Of the 120 patients in our sample, one-quarter had Neuro-QoL Depression scores consistent with mild or moderate depressive symptoms; no patients scored in the severe depressive symptom range. Reported prevalence rates of mood disorders and depressive symptomatology in adults with chronic tic disorder vary considerably across studies, in part due to differences in methods of ascertainment (e.g., psychiatric interview [
3,
4] versus self-report measures [
3,
11,
16]) and sampling (e.g., treatment-seeking [
1,
3,
4,
11] versus nontreatment-seeking [
22] populations). On the basis of psychiatric interviews, 12%–23% of treatment-seeking adults with chronic tic disorder fulfill criteria for current major depressive disorder (
3,
4), but as many as 60% have experienced a mood disorder at some point during their lifetime (
1). In contrast, among nontreatment-seeking adults with chronic tic disorder, only 28% report a prior diagnosis of mood disorder (
22). In studies using self-report measures to assess current depressive symptoms in treatment-seeking adults with chronic tic disorder, 21%–45% of patients have elevated depression scores (
3,
11), the lower end of this range aligning with findings in the present study.
Anxiety symptom severity in our cohort was significantly higher than normative values. Two-thirds of our sample had at least mild anxiety symptoms, and 40% had moderate or severe anxiety symptoms. In accord with our results, one previous study found that 68% of treatment-seeking adults with chronic tic disorder had elevated scores on a self-report anxiety measure (
11). The prevalence of current anxiety symptoms exceeds those of current depressive symptoms in adult chronic tic disorder samples in which both are measured (
11), though, interestingly, the lifetime prevalence of anxiety disorders appears to be lower than that of mood disorders based on psychiatric interviews: 39% versus 60% (
1). One potential reason for this discrepancy is that many individuals with anxiety symptoms may not meet diagnostic criteria for an anxiety disorder. Critically, subthreshold anxiety symptoms are linked with significant burden and impairment (
36). A dimensional approach may allow researchers and clinicians to more accurately quantify the impact of anxiety in adults with chronic tic disorder.
Consistent with previous research, both depression and anxiety were associated with a more severe chronic tic disorder phenotype in our cohort. Similar to other studies adopting a dimensional approach to evaluate adults with chronic tic disorder, depressive and anxiety symptom severity correlated strongly with each other (
6,
7), with tic severity (
5,
6,
11,
16,
22), and with OCD symptom severity (
3,
6,
7). Depressive and anxiety symptom severity also correlated with ADHD symptom severity in our cohort. After adjustment for covariates in the regression analyses, the associations of depressive and anxiety symptom severity with each other and with OCD symptom severity were significant, whereas neither depressive nor anxiety symptom severity was significantly associated with tic or ADHD symptom severity. Interestingly, anxiety and ADHD symptom severity were more strongly associated with each other among women than among men, as evidenced by the significant interaction term in the anxiety regression model. In addition, the strength of the association between depressive and OCD symptom severity was weaker among older than younger patients, which may be partly attributable to the decreasing severity of OCD symptoms with age (
10). Collectively, findings suggest that common psychiatric manifestations of chronic tic disorders are more tightly linked with each other than with tics among adults with the disorder and that investigators must account for the dynamic, multifaceted, and dimensional nature of the chronic tic disorder phenotype when examining the relationships between clinical factors in this population.
The psychiatric symptom profile differed between men and women in our treatment-seeking cohort of adults with chronic tic disorder. Women had significantly greater anxiety symptom severity than men, but depressive symptom severity did not differ between sexes, a pattern of findings observed in another sample of adults with chronic tic disorder (
22). The largest study to date of psychiatric comorbidity among individuals with chronic tic disorder identified higher lifetime prevalence rates of mood and anxiety disorders among female patients than male patients, but the investigators did not report prevalence rates of these comorbid conditions in adulthood stratified by sex (
1). Two findings from the regression analyses in the present study suggest that the relationship of sex with depression and anxiety domains is influenced by other clinical factors. First, after adjustment for clinical covariates, anxiety severity was more strongly associated with ADHD symptom severity among women than men, consistent with findings observed in a large national registry study of adults with ADHD (
37). Second, after adjustment for clinical covariates, depressive symptom severity in our cohort was associated with male sex. This finding appears to be at odds with previous studies that observed greater depression severity in women (
38) or no difference between the sexes (
22). However, previous studies investigating sex differences in depression and anxiety among adults with chronic tic disorder did not adjust for covariates in their analyses (
22,
38).
Beyond the aforementioned sex differences in depression and anxiety, several other findings from the present study add to the accumulating evidence of phenotypic differences and similarities between adult men and women with chronic tic disorder. Men and women in our cohort self-reported similar ages at tic onset, consistent with some but not all studies examining sex differences in tic onset (
20). Men and women in our cohort also exhibited similar total tic severity, although tic-related impairment was greater in women, a pattern of findings in agreement with other studies of women with chronic tic disorder (
21,
22). In addition, severity of both OCD and ADHD symptoms in our cohort were similar between sexes. Female sex is associated with higher lifetime prevalence of OCD and lower lifetime prevalence of ADHD among TS populations (
1,
20), although the between-sex discrepancy in ADHD prevalence narrows when considering adult TS populations (
21,
22). Ultimately, deeper insight into sex-based differences in tics and psychiatric symptoms of chronic tic disorders will require longitudinal studies involving adults with these disorders, particularly since depression and anxiety manifest more prominently in adulthood than childhood within such populations (
1,
39,
40).
Our study had several limitations. First, our study cohort consisted of adults with chronic tic disorder seeking care at a specialty TS clinic, and the cohort was predominantly non-Hispanic and White. As a result, generalizability of our findings to nontreatment-seeking adults with chronic tic disorder and to the broader ethnically and racially diverse population of individuals with chronic tic disorder is unclear. Second, most patients in our study were receiving medications for tics or other neuropsychiatric symptoms, which may have influenced the severity of psychiatric symptoms and the relationships between clinical variables, a limitation shared by other studies of treatment-seeking patients (
1,
3,
4,
11). Third, data used in this study were collected during the COVID-19 pandemic, which may have impacted the severity of various psychiatric symptoms, although agreement of many of our results with prepandemic studies suggests the influence of this limitation was minimal. Fourth, standardized psychiatric interviews are not conducted as part of routine care at our TS clinic; therefore, clinician-confirmed DSM-5 diagnoses of mood disorders, anxiety disorders, OCD, and ADHD were not obtained in this cohort.