Consensus Clinical Guidance for Diagnosis and Management of Adult COVID-19 Encephalopathy Patients
Abstract
Description
The Epidemiological Picture of COVID-19 Encephalopathy
Search Strategy and Methods
What is the Pathophysiology of COVID-19 Encephalopathy?
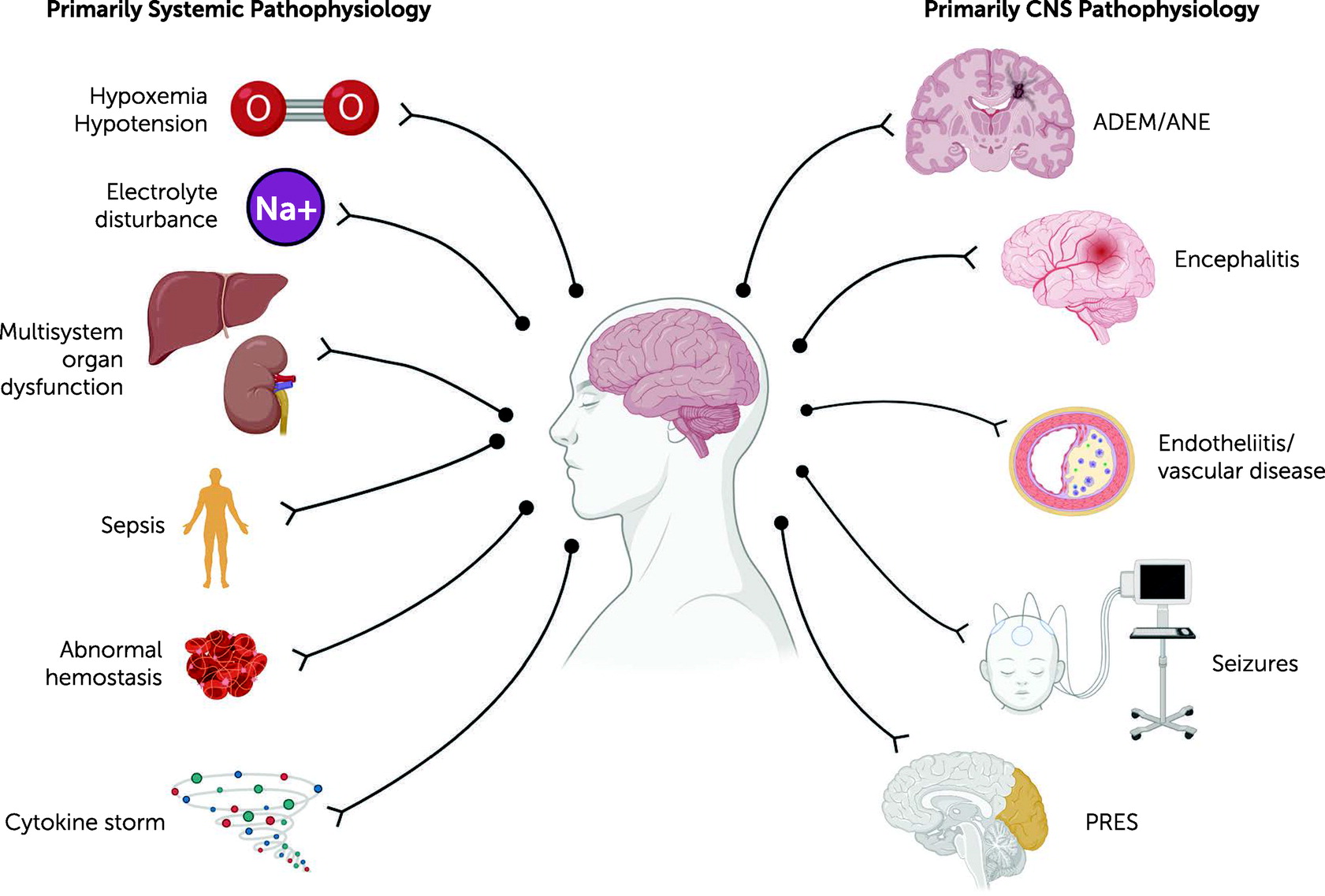
Primary Systemic Pathophysiology
Hypoxemia and hypotension.
Electrolyte disturbance.
Multisystem organ dysfunction.
Sepsis.
Abnormal hemostasis.
Cytokine storm.
Primary CNS Pathophysiology
Endotheliitis/vascular disease.
Acute disseminated encephalomyelitis/acute necrotizing encephalopathy.
Encephalitis.
Seizures.
Posterior reversible encephalopathy syndrome (PRES).
Which Clinical Features Suggest COVID-19 Encephalopathy?
Recommendations
Clinical Approach
Which Clinical Features Suggest a Primary Central Nervous System (CNS) Pathology?
Recommendations
| Pathology | Systemic cause | Investigation |
|---|---|---|
| Organ dysfunction | Hypercapnia/hypoxia, hepatic failure, acute kidney injury, thyroid disorders, and cardiac failure | Pulse oximetry and blood gas; ALT, AST, GGT, and ALP; ammonia; creatinine and urea; TSH and T4; ECG, echocardiography, and clinical examination |
| Metabolic dysfunction | Hypernatremia/hyponatremia, hypercalcemia/hypocalcemia, hypomagnesemia, hyperglycemia/hypoglycemia, hypothermia, fever/hyperpyrexia, and cytokine storm | Plasma Na+, corrected plasma Ca2+, and plasma Mg2+; plasma/finger prick glucose; temperature/observations; IL-1, IL-6, and TNFα (guided by local expertise) |
| Toxicity | Sedatives, corticosteroids, hydroxychloroquine, lopinavir, ritonavir, tocilizumab, and drugs and alcohol | Patient history, treatment review, blood alcohol level, and urinary drug screen |
| Sepsis | Superinfection (typically bacterial or fungal) | Blood, urine, and sputum cultures; serology/PCR |
| Vascular disease | Hypertensive encephalopathy and severe hypotension | Noninvasive or invasive blood-pressure monitoring |
| Nutritional deficiency | Wernicke encephalopathy | B12/thiamine |
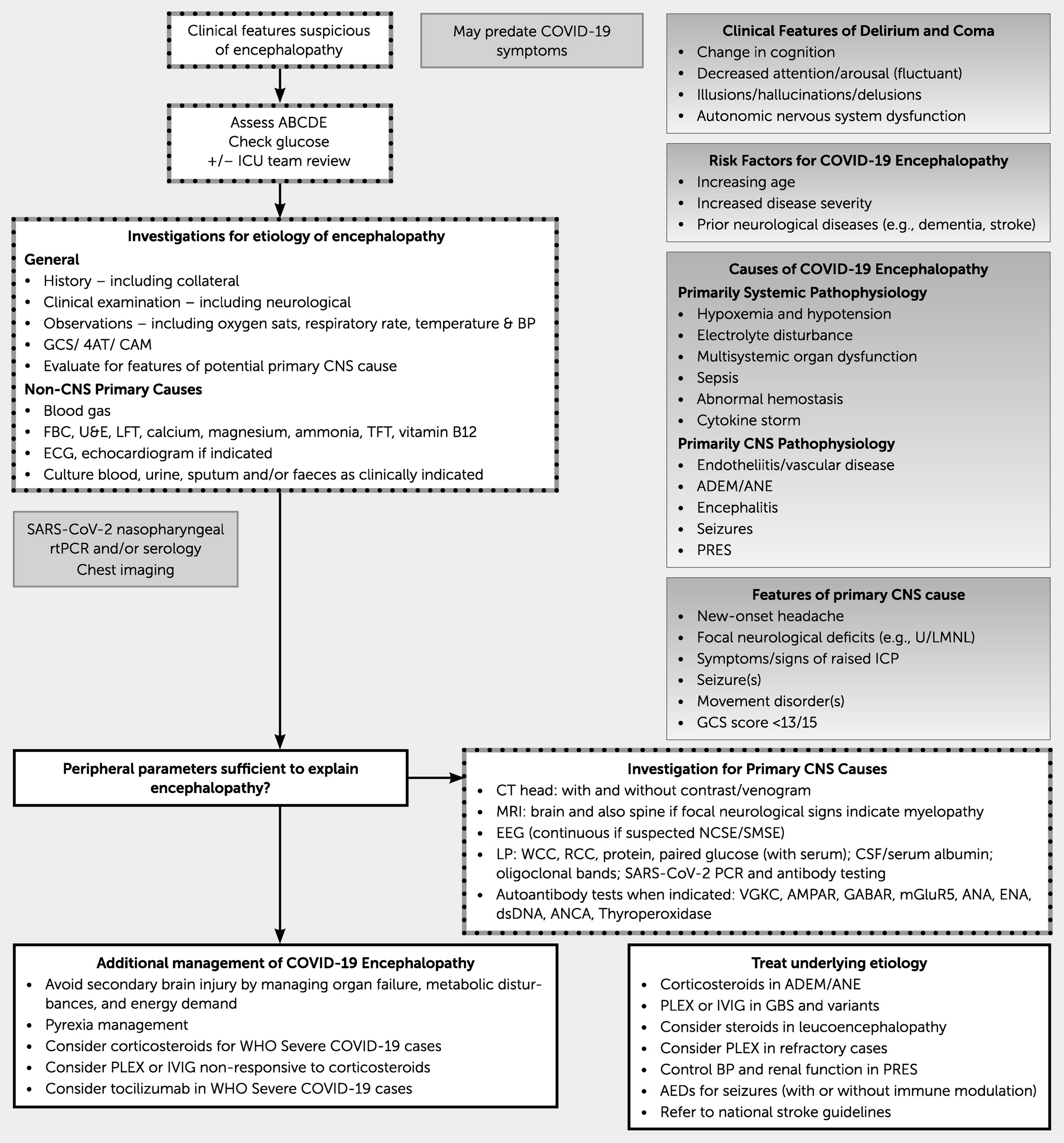
Clinical Approach
What Investigations Should be Performed to Establish These CNS Diagnoses?
Recommendations
Clinical Approach
| Imaging and test | Indication | Investigation |
|---|---|---|
| CT | Altered level of consciousness; headache with “red flags”b; altered behavior; focal neurological signs/symptoms; unexplained generalized seizures; focal/generalized seizures; suspected stroke; and suspected CVST | CT with and without contrast enhancement; CT angiography±CT perfusion in case of sudden-onset symptoms; and CT venography |
| MRI (97) | Same as CT in cases of unclear cause | T1; T2; DWI; FLAIR; arterial time of flight; gradient echo/SWI; T1+gadolinium; and T2+gadolinium |
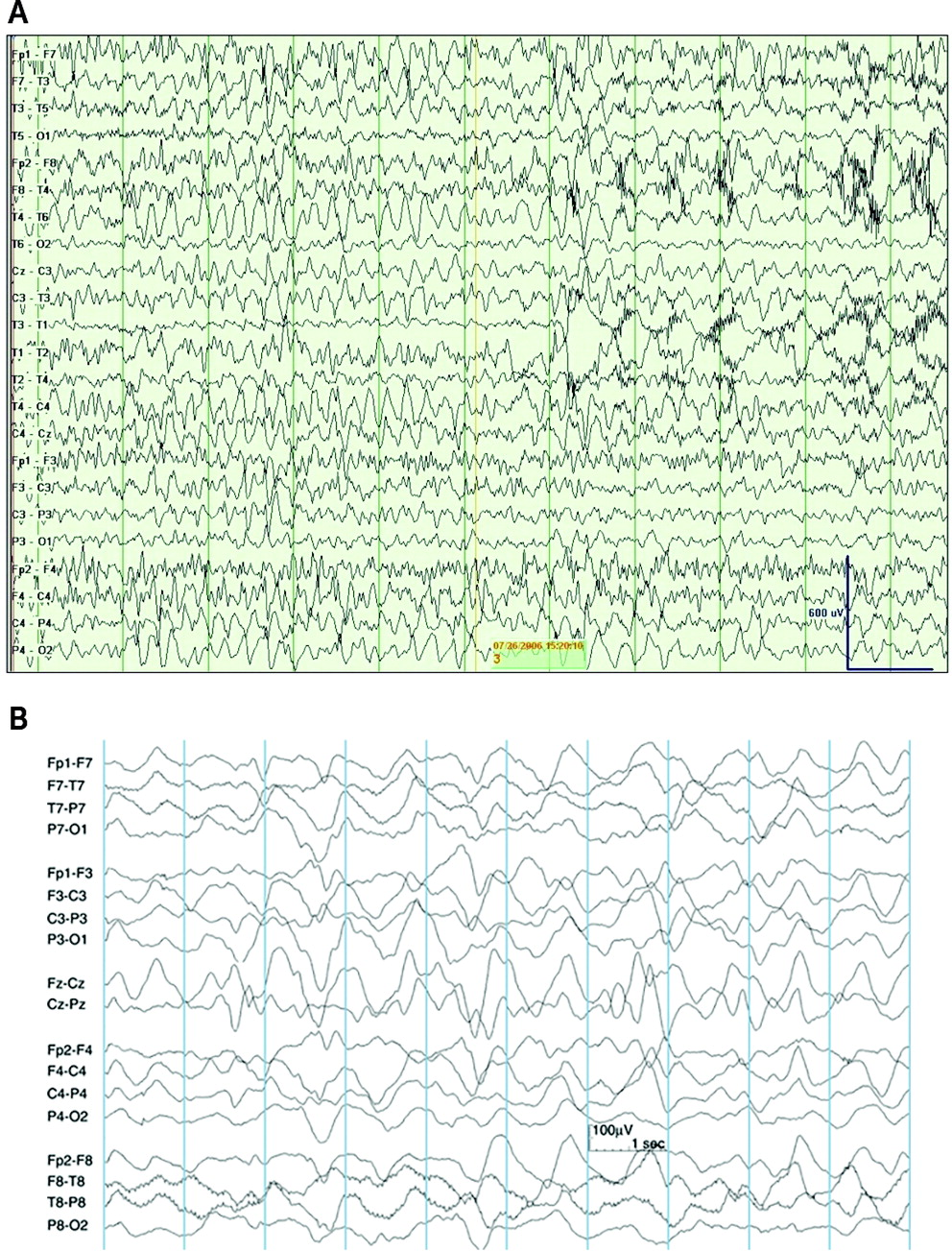
| EEG (96, 98, 99) | Suspected nonconvulsive status epilepticus; suspected subtle motor status epilepticus (when unclear of a psychiatric cause or encephalopathy) | EEG; possible improvement of localization of seizures with video EEG; prolonged monitoring considered |
| LP (76, 100–104) | In case of suspected encephalitis (including ADEM and ANE), as soon as possible; in the absence of another clear explanation for encephalopathy; unexplained seizures or status epilepticus (once stable); and suspected autoimmune encephalitis or Bickerstaff encephalopathy | WBC; RBC; protein concentration; paired serum/CSF glucose; paired CSF albumin/plasma albumin; paired oligoclonal bands; and paired SARS-CoV-2 PCR and antibody |
| Autoantibody tests (105) | Unexplained encephalopathy, particularly if associated with psychiatric features, encephalomyelitis, memory decline, seizures, cerebellar syndrome, movement disorder, or sensory neuronopathy, which may suggest autoimmune encephalitis | Autoantibodies against the following receptors: NMDA-R, LGI-1, CASPR2, AMPAR, GABA-A/B, mGluR5, and DPPX; CRP; ANA; ENA; dsDNA; ANCA; thyroperoxidase autoantibodies; and antiganglioside antibodies |
Neuroimaging.

Examination of CSF for SARS-CoV-2 and antiviral antibodies.
Anti-CNS autoantibody detection.
How Should Patients with COVID-19 Encephalopathy be Managed?
Recommendations
Clinical Approach
Monitoring.
General supportive care.
Iatrogenic insults.
Systemic Immunomodulation
Specific CNS Therapy
What is the Prognosis for Patients with COVID-19 Encephalopathy?
What is the Role of Rehabilitation for These Patients?
Recommendations
Clinical Approach
Footnotes
References
Information & Authors
Information
Published In
History
Keywords
Authors
Competing Interests
Funding Information
Metrics & Citations
Metrics
Citations
Export Citations
If you have the appropriate software installed, you can download article citation data to the citation manager of your choice. Simply select your manager software from the list below and click Download.
For more information or tips please see 'Downloading to a citation manager' in the Help menu.
View Options
View options
PDF/EPUB
View PDF/EPUBLogin options
Already a subscriber? Access your subscription through your login credentials or your institution for full access to this article.
Personal login Institutional Login Open Athens loginNot a subscriber?
PsychiatryOnline subscription options offer access to the DSM-5-TR® library, books, journals, CME, and patient resources. This all-in-one virtual library provides psychiatrists and mental health professionals with key resources for diagnosis, treatment, research, and professional development.
Need more help? PsychiatryOnline Customer Service may be reached by emailing [email protected] or by calling 800-368-5777 (in the U.S.) or 703-907-7322 (outside the U.S.).