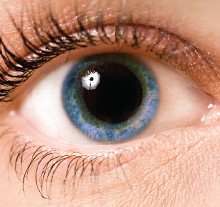
Pupil Dilation May Help Determine Depression Risk
Pupil dilation in response to emotional stimuli may help identify individuals who are at greatest risk for depression following a natural disaster, according to a report in Clinical Psychological Science.
“After major stressful events like natural disasters, research suggests only about 20 to 25 percent will go on to develop a depressive disorder,” said lead study author Mary Woody, a Ph.D. student at Binghamton University in New York, in a press release. These findings suggest “that pupil dilation could be used to identify those who are at greatest risk for depression.”
Woody and her colleagues at Binghamton University evaluated 51 women who were living in Binghamton in 2011, when catastrophic floods swept through the region. As part of a separate study, these women had their pupillary responses to emotional images assessed prior to the floods.
The researchers found that decreased pupil dilation to emotional expressions predicted a significant increase in depressive symptoms following the flood, but only in women who experienced higher levels of flood-related stress.
Some previous research has found that pupillometry can predict who responds best to psychotherapies such as cognitive-behavioral therapy. The current study builds on that research and suggests that pupillometry could identify good candidates for psychotherapy in the immediate aftermath of a natural disaster.
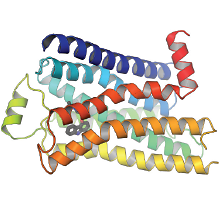
Researchers Discover Potential Pathway Toward Sustained Pain Relief
G-protein coupled receptors (GPCRs) are known to regulate pain transmission, but most GPCR-targeted painkillers have failed in clinical studies. A study published in Science Translational Medicine has demonstrated that one GPCR known as neurokinin 1 receptor (NK1R) can migrate inside the cell in response to pain—and out of reach of most traditional analgesics.
Using rodent models, researchers from Monash University in Australia and colleagues observed that when stimulated by pain, NK1R moved from the surface of nerve cells to intracellular compartments known as endosomes. When the researchers used chemical and genetic techniques to block the ability of NK1R to internalize, they found that the animals showed less pain sensation in their paws after injections of capsaicin.
The researchers then joined an NK1R inhibitor (spantide I) with a cholesterol-like molecule, thus allowing the drug to directly pass through the fatty cell membrane and into the cells. This method provided sustained pain relief that lasted several times longer than spantide I without this conjugate.
“Our study suggests that therapeutic targeting of endosomal GPCRs is a paradigm of drug delivery that offers more effective and selective treatment for pathophysiological conditions, including chronic pain,” the investigators concluded.
Jensen D, Lieu T, Halls M, et al. Neurokinin 1 Receptor Signaling in Endosomes Mediates Sustained Nociception and Is a Viable Therapeutic Target for Prolonged Pain Relief.
Sci Transl Med. May 31, 2017; 9(392): eaal3447.
http://stm.sciencemag.org/content/9/392/eaal3447.shortBiomarker for Alzheimer’s May Be Modifiable by Stress Reduction
The repressor element 1-silencing transcription (REST) factor—a protein that regulates stress responses in the brain—may be a viable blood-based biomarker of Alzheimer’s disease (AD), reports a study appearing in Translational Psychiatry by researchers at University College London.
Previous studies suggest that reduced levels of REST in the brain are associated with increased cognitive impairment, but it was unknown if REST measured in plasma would differ between people with AD, mild cognitive impairment (MCI), and healthy controls.
When the researchers compared plasma REST levels in people with stable MCI, people with worsening MCI, Alzheimer’s patients, and healthy controls, they found that plasma REST levels declined with increasing severity of impairment.
Next, the investigators explored whether interventions that target stress might lead to changes in REST levels. The researchers measured REST in 81 older adults with symptoms of depression or anxiety but not dementia before and after the adults participated in a mindfulness-based stress reduction program or health-education program as a control.
Mindfulness-based training was associated with an increase in REST levels compared with the control intervention, and increased REST was associated with a reduction in depression and anxiety symptoms.
“These findings presented here are of great significance for the diagnosis and clinical management of AD, as determining REST in blood provides a prognostic marker that can help stratify patients for inclusion in trials, identify those at high risk of ‘stress-induced’ cognitive decline, and determine the efficacy of therapeutic interventions,” the study authors wrote. “Importantly, we demonstrated that REST levels can be modulated through a relatively brief behavioral stress-reduction intervention and that changes in REST are associated with clinical improvements.”
Ashton N, Hye A, Leckey C et al. Plasma REST: A Novel Candidate Biomarker of Alzheimer’s Disease Is Modified by Psychological Intervention in an At-Risk Population. Transl Psychiatry. June 6, 2017; 7(6): e1148.
Risk Factors Identified For Autism-Related Hospitalization
Researchers at Brown University have identified five factors that may increase the risk of psychiatric hospitalization in children and adolescents with autism spectrum disorder (ASD).
Notably, only two of the five risk factors identified in the study were related to ASD symptomology: lower adaptive functioning and higher severity of social-affective ASD symptomology. The other three risk factors related to psychiatric hospitalization were the presence of sleep problems, the presence of a mood disorder, and living with a single caregiver. Of these, the presence of a mood disorder was the strongest risk by far, with roughly a seven-fold increased risk of hospitalization.
The analysis came from two large datasets of ASD patients. The Autism Inpatient Collection (AIC), which incorporates data from six children’s psychiatric hospitals specializing in developmental disorders, and the Rhode Island Consortium for Autism Research and Treatment (RI-CART), which includes ASD patients and families from the general community.
By comparing 218 patients between the ages of 4 and 20 from AIC with 255 age- and gender-matched RI-CART youth who were not hospitalized, the researchers were able to identify traits that were independently associated with hospitalization risk.
“[T]he present findings reveal indicators that may be useful for identifying children and adolescents at greater risk of psychiatric hospitalization as well as offer potential targets for individual and family intervention aimed at reducing the likelihood of requiring acute psychiatric services,” the authors noted.
The analysis was published in Journal of Autism and Developmental Disorders.
CBT Found to Have Long-Term Benefits for Body Dysmorphic Disorder
Cognitive-behavioral therapy (CBT) has been shown to be effective at treating adolescent body dysmorphic disorder (BDD) in the short term, but few studies have examined long-term effects of this intervention.
A follow-up study of adolescents with BDD who received CBT now provides evidence that improvements can last for up to 12 months. The study, led by researchers at Kings College London, was published in Behavior Therapy.
As part of the original study, 26 adolescents aged 12 to 18 received 14 sessions of CBT for BDD over a four-month period. Two months after the last CBT session, the researchers assessed BDD symptoms, as measured by the Yale-Brown Obsessive-Compulsive Scale Modified for BDD, as well as other outcomes including depression, disease insight, and quality of life. They found that BDD symptom scores dropped by around 11.5 points, and several secondary measures also improved.
Study participants were evaluated for an additional 10 months, during which they received three CBT booster sessions.
During the follow-up period, the researchers found that the adolescents maintained their BDD symptom improvements and that the number of participants who could be classified as responders (>30 percent reduction in symptom scores) increased from 35 percent to 50 percent. Secondary outcomes remained stable as well.
Despite these improvements, the authors noted that by 12-month follow-up, only about half of the sample could be classified as “treatment responders.” Additionally, two participants attempted suicide during the follow-up period, and five sought consultations for cosmetic procedures.
“Our findings suggest that a significant proportion of adolescents who receive CBT for BDD continue to experience clinically significant symptoms in the longer term and remain vulnerable to a range of potential risks and negative outcomes. … For this reason, we recommend long-term monitoring of these patients.” ■