Allocation of resources to prevent and treat mental illness is low compared with the burden that mental illnesses place on individuals and society (
1). According to the World Health Organization, for example, in industrialized countries such as the United States, depression is second only to ischemic heart disease in terms of total health burden (
2). In aggregate, mental illnesses account for 15.4% of the total burden caused by all disease in developed countries. Yet, according to the U.S. Department of Health and Human Services, mental health conditions account for only 6.2% of U.S. health care expenditures (
3). This pattern is paralleled in the allocation of resources for federally sponsored health research. In the National Institutes of Health budget in 2006, approximately 5% went to the institute primarily responsible for mental health research, compared with 17% for cancer and 16% for allergy and infectious diseases (
4).
Why is there a disconnection between the burden imposed by mental illness and the allocation of resources to understand, prevent, and treat such illnesses? Some experts attribute part of this disparity to public attitudes toward mental illness (
1,
5–
8). According to results from the 1996 General Social Survey, public support for mental health funding is low compared with support for funding of other government services, including general health services (
8). Specifically, 68% of people in that survey favored increased government spending for health care generally, but only 50% felt this way about mental health care (
8). Some researchers have suggested that societal stigmatization of mental illness may explain this reluctance to allocate resources for treatment (
5,
7,
9,
10). For example, people who hold individuals with mental illness personally responsible for their illness have been found to express less support for funding programs to help them (
1). In addition, evidence from the General Social Survey suggests that people who have personal experience with mental illness—who therefore are presumably less likely to hold stigmatizing beliefs—are more willing to support treating mental health conditions (
11).
Although previous studies have measured general attitudes toward funding for mental health, none have established whether apparent apathy toward mental illness simply reflects a belief that mental illnesses are not as burdensome as many general medical illnesses. If people underestimate the burden imposed by mental health conditions, then their answers to questions about preferences for treating general medical conditions might reflect a perception that general medical conditions are more serious or disabling. In addition, certain beliefs about mental illnesses could lead to relative devaluation of treatments for them, even among people who acknowledge that such illnesses cause significant suffering. For example, some people may believe that given enough willpower, they would be able to recover from a mental illness on their own, without medical intervention. These persons might imagine that mental illnesses severely detract from quality of life, but they may also feel reluctant to pay as much for treatment of these illnesses.
To examine these issues, it is important to systematically compare perceptions of mental illnesses and of general medical illnesses in a way that separates perceptions of burdensomeness from a willingness to prioritize treatments for these conditions. In this article, we report findings from a national survey of U.S. adults in which we elicited their perception of the burdensomeness of a series of mental and general medical illnesses and their willingness to pay to cure themselves of the illnesses (
12–
15). This approach allowed us to assess whether the public would undervalue treatments for mental health conditions compared with general medical conditions and to determine whether willingness to pay less for mental health care results from a perception that these conditions impose a lower burden or because of some other reason.
Methods
Data collection
Participants were recruited from an Internet panel managed by Knowledge Networks, a survey research firm. Knowledge Networks maintains a panel of more than 60,000 households, a representative sample of the U.S. population of adults (over age 21) who were originally recruited by random-digit dialing. As an inducement to join the panel, and to facilitate study implementation, the firm provides Internet access to all households that agree to participate. Providing Internet access for panel members who do not already have it reduces a source of bias typically present in Internet survey studies. Results from surveys of this panel have been widely reported in a variety of disciplines (
16–
25). In June and July 2006, our survey was sent to a random sample of 1,000 panel members, of whom 710 completed the survey, for a response rate of 71%.
Respondents were presented with descriptions of five health conditions (diabetes, below-the-knee amputation, partial blindness, depression, and schizophrenia). The order of presentation of these conditions was fully counterbalanced and randomized (that is, every participant saw all five scenarios and was randomly assigned to one of 120 possible orders of presentation). After reading each description, respondents were asked to indicate how much they would be willing to pay out of pocket on a monthly basis for a treatment that would allow them to avoid each condition (
15). Respondents then provided a rating of the burdensomeness of each condition (described below), using the same order of presentation. The survey included several other measures (for example, demographic characteristics), which are described below.
All participants in this study were treated in accordance with all applicable ethical guidelines for human research. The study procedures were approved by the University of Michigan Medical Institutional Review Board.
Health condition descriptions
Participants read brief descriptions of all five health conditions. [These descriptions are provided online as a data supplement to this article.] The descriptions focused on symptoms or level of disability, or both. For general medical illnesses, diabetes was described as requiring blood sugar monitoring and insulin shots, but without any complications or symptoms; below-the-knee amputation was described as uncomplicated by stump pain or phantom limb pain, with a well-functioning prosthesis; partial blindness was described as a level of impairment that would preclude driving or reading but would allow navigating a room by sight. To create a description of depression, we modified statements from the Montgomery-Asberg Depression Rating Scale for moderate depression (for example, “You feel sad or downhearted a lot of the time.”) (
26). For schizophrenia, we described symptoms such as hallucinations and disordered thoughts, as well as side effects of medications, such as abnormal movements. In all cases, the descriptions indicated that any disability of symptoms were being experienced even though currently available treatments were being administered.
Measures
For each health condition, participants indicated how much they would be willing to pay to avoid experiencing the condition (
12–
15). We used an open-ended response format, using the following wording: “Suppose a pill existed that would allow you to permanently and completely avoid ever having [health condition]. However, without the pill, you would have [health condition] as described in the scenario, within a month. This pill is not covered by insurance and you will have to pay for it out-of-pocket using your own financial assets and income. Please estimate the maximum dollar amount you think you would be willing and able to pay monthly for this treatment.”
Additional instructions emphasized that participants should consider their actual available financial resources in answering the question and that their answer should reflect how much they would value avoiding the health condition, rather than how much they think such a treatment should cost (
15,
27).
To measure the perceived quality-of-life burden of each condition, we asked participants to choose a number between 0 and 100 that best represents the overall quality of life with that condition, where 0 represents the worst imaginable quality of life and 100 represents the best imaginable quality of life. We then subtracted their quality of life estimate from 100 to generate ratings of perceived burden (that is, higher numbers indicate greater burden).
As a distractor task between willingness-to-pay evaluations and ratings of burden of the five conditions, we used an innocuous measure—a seven-item measure of subjective numeracy (
28)—that was not related to the central aims of the study. At the end of the survey, respondents were asked whether they had ever experienced each of the health conditions described.
Analyses
We first compared burden ratings (range 0–100) for the conditions using within-subjects t tests. Given the skewed distribution observed with open-ended willingness to pay, we compared willingness to pay for depression to willingness to pay for each of the other general medical illnesses, using Wilcoxon signed ranks tests. We also compared schizophrenia with depression and with the other general medical illnesses.
Finally, for descriptive purposes we created a variable that combined the burden and willingness-to-pay ratings. Specifically, for each participant and for each condition we computed a value that equaled the participant's willingness-to-pay value divided by his or her quality-of-life burden score. This variable, therefore, represents a willingness-to-pay value for a one-unit increase in quality of life as a result of curing the health condition. By comparing this value across health conditions, we were able to assess whether respondents systematically prioritized some conditions over others, aside from any differences in their perception of the burdens caused by those conditions. Finally, we repeated our primary analyses after excluding individuals who reported ever having had any of the health conditions described in the survey.
Results
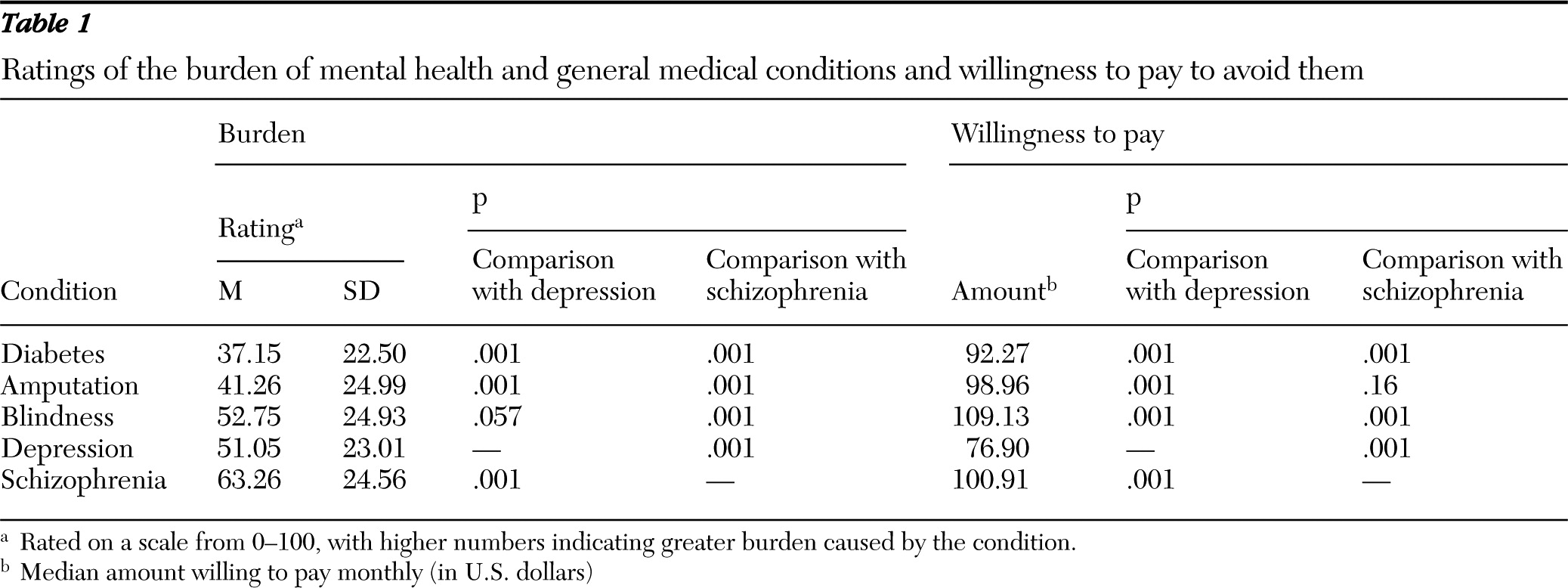
Results in
Table 1 show that depression received a higher burden score than amputation or diabetes; the depression score was comparable to that for partial blindness. Despite this relatively high burden rating, depression received the lowest median willingness-to-pay value; willingness to pay for depression was significantly lower than willingness to pay for diabetes, amputation, or partial blindness (p<.001 for all three).
Schizophrenia received the highest mean burden score, but it did not have the highest willingness-to-pay valuation. Instead, willingness to pay to avoid schizophrenia was similar to willingness to pay to avoid amputation and significantly less than willingness to pay to avoid partial blindness (p<.001), even though schizophrenia was rated as more burdensome than either of these conditions.
We also examined the ratio of willingness to pay to perceived burden, or willingness to pay for each unit of increase in quality of life. On the basis of this computation, willingness-to-pay valuations to avoid the two mental health conditions were about 40% on average less than those for the three general medical illnesses ($2.76 per unit compared with $1.70 per unit; p<.001) (data not shown).
In a separate series of analyses (data not shown), we excluded participants who indicated that they had experienced any of the health conditions described in the survey to determine whether this experience influenced the pattern of results. We excluded 260 respondents, most of whom (N=208) reported having experienced depression. None of the findings described above were substantively altered by the exclusion of these respondents. Even when those with experience of the conditions were excluded, participants were willing to pay less to avoid depression than to avoid any of the three general medical illnesses (p<.01 for all comparisons).
Discussion
In our study, a nationally representative sample of U.S. adults expressed a willingness to pay significantly less to avoid mental illness than to avoid general medical illness. This lower valuation was not simply a result of respondents' minimizing the burden of depression and schizophrenia. In fact, study participants rated these two mental illnesses as generally being more burdensome than the general medical illnesses we described. Rather, even after we accounted for respondents' own perceptions of how these illnesses would influence quality of life, they were willing to pay substantially less to avoid mental illnesses such as depression or schizophrenia than to avoid physical illnesses such as diabetes, partial blindness, or below-the-knee amputation.
For example, respondents assigned comparable levels of burdensomeness to partial blindness and moderate depression but were willing to spend over 40% more to avoid blindness than to avoid depression. This pattern of preferences within individuals parallels the overall allocation of treatments at the societal level, where the relative prioritization of mental health care falls below what might be expected given the prevalence and burdensomeness of mental health conditions.
These findings are novel, in that they suggest that treatments for mental health conditions such as depression are devalued by the public and that this devaluation is not a result of a belief that mental illness is not as severe or burdensome as general medical illness. The results also build on previous work examining the public's general willingness to allocate funds to treat mental illness. The willingness-to-pay elicitation we used asked participants to imagine themselves with the condition and to indicate their willingness to pay out of pocket for their own treatment, not to make allocation decisions for others or to weigh in on public financing. Nevertheless we observed a clear preference for paying to avoid the general medical illnesses we described compared with the mental illnesses—a preference that persisted even after perceived burden of the conditions was taken into consideration.
Our findings have potential implications for understanding the relatively low priority assigned to allocating resources for mental health treatments. If the public would not pay as much to avoid suffering the effects of a mental illness themselves—even while recognizing its relatively greater negative effect on quality of life—then they may not be as willing to demand greater prioritization of mental health care. In addition, our results suggest that efforts to eliminate the gap in resource allocation priorities between mental health conditions and general medical conditions will likely require targeting specific beliefs that people have about mental illnesses and the value of treatments for mental illness.
Because our study focused on willingness to pay for one's own treatment, it does not have direct implications for the study of stigmatization of people with mental health conditions. However, beliefs about mental illness, such as the ones studied here, may result in both stigmatizing attitudes toward people who have mental illness and devaluation of treatments. For example, a belief that mental illnesses are under one's personal control could result in lower willingness-to-pay valuations (why pay as much for something you can “get over” on your own) and in casting blame on people who have a mental illness (“it's their own fault”). For now, this must remain speculative, but future research can examine this and other possibilities.
Our study has several limitations. Our methodology necessarily relied on a hypothetical valuation of an idealized treatment. We did not ask respondents to value a “cure” for an illness but rather to pay for a hypothetical treatment that would allow them to avoid having to experience the illness. We chose this frame for a simple reason—to standardize the mode of treatment. A “cure” for amputation, for example, would presumably be surgical, and thus naturally costlier, in participants' eyes, than a treatment for depression of diabetes, such as a medication. However, it could be argued that our results are an artifact of this unusual framing. Although we cannot fully discount this possibility, in a survey conducted before the one reported here we pilot-tested several elicitation methods for willingness to pay for these conditions. In the pilot test (also an Internet panel survey, although not with a nationally representative sample), we examined the standard “cure” frame for willingness to pay and observed the same pattern of results reported here. Thus we do not believe our results are restricted to the particular “avoid” frame chosen.
But other concerns with the willingness-to-pay elicitation remain. These measures have been criticized for failing to capture individual's true preferences, because they ask them to place dollar values on things that they are not used to paying for. Thus it could be argued that the disparity we observed between illness burden ratings and willingness to pay merely reflects measurement error. However, within each of the two broad categories of illness, there was a direct relationship between quality-of-life estimates and an individual's willingness to pay. For example, for the general medical illnesses, the more burdensome respondents thought the illnesses, the more they were willing to pay to avoid them. The same pattern was observed between the two mental illnesses. Instead, the disparity between quality-of-life estimates in people's willingness to pay occurred only when mental illness was compared with general medical illness.
Open-ended versions of willingness to pay, such as the one we used, are prone to some problems, most notably positive skew because of high value responses. Some have recommended forced-choice formats as an alternative (
29). However, these formats have been criticized as well for introducing starting-point biases. A review published in 2004 found no evidence of clear superiority of one format over the other (
30). In our case, given the relative complexity of the task, we thought it wise to choose the simpler open-ended format and to accept the limitations of the approach (for example, the need to use nonparametric tests in our analyses). Again, it is reassuring to see that within the general medical conditions, willingness to pay tracked closely with perceived severity, which can be viewed as a test of validity of the approach.
More broadly, the willingness-to-pay valuation is, by its nature, a hypothetical exercise, which may not always accurately reflect actual behavior. Thus, although we believe that the measure was well suited to our purposes regarding relative willingness to incur costs across these conditions, the actual values obtained should be interpreted with caution.
There are some other methodological limitations worth discussing. We elicited willingness to pay before eliciting burden ratings for each of the conditions; thus it is possible that there were carryover effects between the elicitations. To minimize such effects, we inserted a distracting task to create distance between the two elicitations. Furthermore, any carryover effects would tend to increase the consistency between the willingness to pay and burden, but we observed disparities between willingness to pay and quality-of-life estimates for mental health versus general medical conditions. In addition, in large prior pilot studies that used the same elicitations, we randomized the order of the elicitations but consistently found the same pattern of results.
In addition, participants may simply have not accepted our descriptions of the hypothetical treatments as effective when those treatments were for depression or schizophrenia. This could explain their reluctance to pay, even when they believed that the conditions are serious. Of course, the treatments for all five conditions were similarly hypothetical and idealized—there is no cure for diabetes, for example—and we have no reason to believe that respondents simply refused to play along with the hypothetical scenario only for the two mental illnesses. But we cannot rule this out. We will note that if skepticism about efficacy of treatments for mental illnesses is so strong so as to bias responses even in the case of hypothetical scenarios, this would represent an interesting finding well worth following up.
Similarly, the respondents may have believed that depression, for example, would improve on its own, obviating the need to pay for treatment. Indeed, depressive symptoms wax and wane over time. However, this would not explain the relatively low valuations given for schizophrenia. Schizophrenia symptoms get milder later in life, but there is no evidence that this is widely known to the general public; rather most people believe schizophrenia and depression worsen with time (
31,
32).
Finally, our study elicited ratings for only a small number of health conditions and for only one level of severity for each of the illnesses. We don't know how people would rate severe depression or a milder form of blindness, for example. Nevertheless, the strength of our study is that we elicited both quality-of-life estimates and willingness-to-pay measures for the same health conditions, and we were able to find a striking discrepancy between people's willingness to pay to avoid general medical illness versus mental illness.
Conclusions
Our study demonstrated that respondents were willing to pay significantly less to avoid mental illnesses than they were to avoid other medical illnesses. It is clear that this lower willingness-to-pay valuation was not merely a result of respondents' minimizing the burden and impact of mental illness. Even when they acknowledged that mental illnesses such as depression and schizophrenia can have large effects on quality of life, these attitudes did not “translate” to their pocketbooks.
Public attitudes likely influence how much payers for health care are willing to spend to treat mental illness and how likely federal agencies are to invest in research on mental illness. Those who feel that the public is shortchanging mental illness will need to do more than convince the public that mental illnesses cause great burden or that people who bear that burden are worthy of help. It should be a priority to explore the deeper underlying attitudes that reduce people's willingness to spend money to avoid mental illness.
Acknowledgments and disclosures
This research was supported by grant R01HD040789 from the National Institute of Child Health and Development. The authors are grateful for the assistance of the team at Knowledge Networks, especially Mike Dennis, Ph.D., Bill McCready, Ph.D., Vicki Pineau, M.S., and Poom Nukulkij, M.A.
The authors report no competing interests.