It is an accepted view that community mental health systems should provide a continuum of care, encompassing outpatient, residential, emergency, and acute inpatient services (
1). Budget shortfalls and resource constraints increasingly lead mental health systems to reduce services (
2). Acute inpatient services are often targeted for reductions because they are typically the most costly (
3). Local, national, and international studies have repeatedly shown that reducing inpatient capacity in state psychiatric hospitals and other long-stay hospitals does not result in negative patient or community outcomes, such as decreases in patient functioning or increases in rates of suicide, incarceration, or crime (
4–
10). When capacity is reduced in long-stay hospitals, services successfully shift to community-based outpatient and residential settings, augmented with acute inpatient care in community hospitals (
5,
11–
13).
Few studies have examined capacity reductions in the community hospitals that now provide the majority of inpatient psychiatric care (
14). In addition, studied reductions in long-stay inpatient services have typically been accompanied by targeted expansion of alternative community services. Inpatient capacity reduction has not been well studied in the absence of increases in alternative services or in the context of widespread reductions across the continuum of care.
Acute inpatient services in public-sector settings are of particular interest because they provide safety-net care to indigent patients and others who cannot access private-sector care. Recent data suggest that reductions in public inpatient beds may result in higher suicide rates (
15). With such potentially high stakes, it is critical to examine the impact of reductions in acute public-sector inpatient services.
This study examined the impact of reductions in acute public-sector inpatient capacity in the context of a natural experiment resulting from two separate reductions in the number of acute psychiatric inpatient beds at San Francisco General Hospital (SFGH), San Francisco's primary provider of inpatient and emergency psychiatric services. These inpatient capacity reductions occurred in the context of widespread reductions in public mental health services and were not accompanied by increases in alternative community services.
The hypothesis that inpatient capacity reductions would have a negative impact on patients and the community was tested by using administrative data. Negative impacts would be anticipated initially in the psychiatric emergency service, because most inpatients are admitted through that service. Fewer opportunities to admit acutely ill patients to inpatient care could lead to overcrowding in the emergency service, reflected in increased length of stay, a greater number of hours closed to new admissions, and fewer patients served. Efforts to curtail overcrowding could lead to more stringent criteria for emergency care that would restrict services to the most severely ill and poorly functioning patients. Likewise, capacity reductions would be expected to have an impact on the inpatient service, leading to decreases in the number of patients served and increases in discharges to restrictive settings such as state hospitals and jails, as well as increases in recidivism to inpatient care if patients were discharged prematurely to permit new admissions. In addition, capacity reductions could differentially affect subgroups of patients defined by diagnosis, age, gender, or race-ethnicity. Finally, reductions could lead to higher levels of inadequately treated mental illness in the community, which could be reflected in increases in the number of suicides and the number of persons with mental illness in the criminal justice system.
Methods
Clinical context
SFGH is the primary provider of care to San Francisco's uninsured and indigent residents and the primary provider of emergency and acute inpatient psychiatric services for adults over age 18. SFGH houses the only 24-hour psychiatric emergency service available to San Francisco residents that accepts patients on involuntary legal holds. Annually, there are approximately 5,700 admissions to the emergency service.
Before July 2008, SFGH operated four inpatient psychiatry units, comprising 79 beds, that were staffed to serve acutely ill patients. There were approximately 1,770 admissions annually. These units consistently operated at full capacity, making it difficult to admit acutely ill patients and making overcrowding in the psychiatric emergency service a common problem. To make beds available to the most acutely ill patients, efforts were ongoing to reduce inpatient length of stay. Between January 2007 and June 2008, mean length of stay decreased approximately 12%, from 11.1 days to 9.8 days; however, the four inpatient units continued to operate at full capacity.
In July 2008, major shortfalls in the community mental health system budget necessitated a range of service reductions, including closure of one of the inpatient units, reducing capacity from 79 to 61 beds. After additional budget reductions in January 2009, one of the remaining acute units was converted to a subacute level of care. The subacute unit is cost saving because it has a lower staffing level appropriate for patients who no longer meet criteria for acute care. At treating clinicians' discretion, patients are transferred to the subacute unit, where they can be served more cost-effectively until community placements become available. However, acutely ill patients cannot be admitted to the subacute unit. Thus, although inpatient capacity remained at 61 beds, acute inpatient capacity was further reduced in January 2009 to 40 beds.
Data sources and impact indicators
Data on SFGH psychiatric inpatient and emergency services were obtained from departmental databases from January 1, 2007 (18 months before the first acute inpatient capacity reduction), through September 30, 2009 (nine months after the second capacity reduction).
Indicators of overcrowding in the psychiatric emergency service included number of patients seen, admissions to the SFGH acute inpatient service from the emergency service, length of stay in the emergency service, and hours when the service was closed to new admissions. Indicators of efforts to control overcrowding by implementing more restrictive criteria for admission to the emergency service included involuntary admission, patient level of functioning at admission and discharge, and redirection without admission to the emergency service. Level of functioning was measured by Global Assessment of Functioning (GAF) (
16) scores assigned by treating clinicians.
Redirection without admission to the emergency service could reflect more stringent admission criteria. Individuals who visit the emergency service receive a preadmission evaluation to determine whether they require emergency care; a few are redirected to other services because they are not experiencing a psychiatric crisis. If reductions in acute inpatient capacity led to overcrowding in the emergency service, the threshold for admission might be raised, increasing the number of individuals redirected without admission.
Indicators of impact on the inpatient service included the number of patients discharged, mean length of stay, discharge disposition, and inpatient recidivism, defined as readmission within 30 days of inpatient discharge. Inpatient length of stay includes days spent on both acute and subacute units.
For both emergency and inpatient services, case mix was characterized in terms of patient age, gender, and race-ethnicity. Primary diagnosis at discharge was also examined for the inpatient service.
Data on suicides among clients of the community mental health system were obtained from San Francisco Community Behavioral Health Services. Since suicide is a relatively rare event, these data were obtained for a longer period of time, starting in January 2003, and aggregated by month. Data from psychiatric evaluations conducted in the San Francisco County Jail were obtained from Jail Health Services. Only annual data were available from jail evaluations.
Analyses
Data were analyzed in two ways. Preliminary pre-post analyses were conducted with admission as the unit of analysis. Because most impact indicators were either dichotomous or counts, general estimating equation methods were used, with a binomial distribution for dichotomous indicators and a Poisson distribution for counts (with a negative binomial distribution used in instances of overdispersion). The first postintervention period (after the unit closure) and the second postintervention period (after the subacute unit conversion) were compared with the preintervention period.
The pre-post comparisons do not account for contemporaneous trends, cycles, and other autocorrelations that could obscure the impact of the capacity reductions. Therefore, time series analyses that controlled for these background factors were conducted to more rigorously evaluate the impact of the two capacity reductions. Data aggregated by day were analyzed by using autoregressive, integrated, moving-average methods, employing established strategies to identify and model autocorrelation (
17,
18). Impact of capacity reduction was examined in two ways. First, impact was examined directly by using two binary variables that were set to 0 before the implementation of each reduction and set to 1 after implementation. Second, outlier detection methods (
19) were used to identify sustained “level shifts” that could reflect delayed effects.
Research procedures were approved by the University of California, San Francisco, Committee on Human Research.
Results
Pre-post analyses
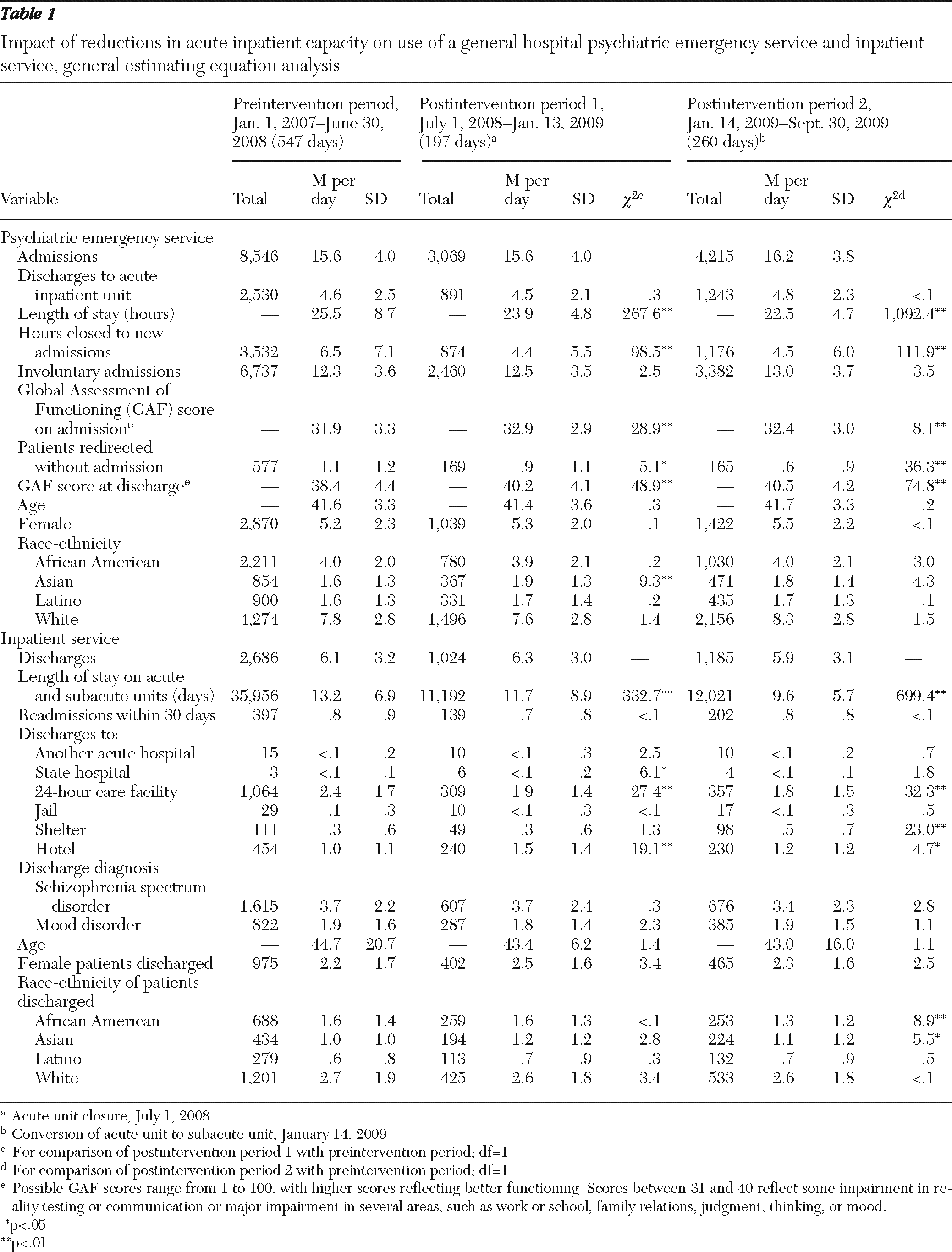
Hypothesized negative impacts of reductions in acute inpatient capacity were not observed in the psychiatric emergency service. As detailed in
Table 1, pre-post comparisons showed no evidence of overcrowding as a result of the lack of opportunity to admit patients to the inpatient service. The number of patients seen per day remained stable over time. Length of stay did not increase; in contrast, statistically significant decreases were observed in both postintervention periods. The number of patients admitted to the acute inpatient service did not decrease. Hours closed to new admissions decreased rather than increased.
There was little indication that criteria for admission to emergency care became more stringent to control overcrowding. The number of patients redirected without admission decreased rather than increased. Hypothesized decreases in patient functioning, as measured by the GAF scale, were not observed; instead, statistically significant increases in functioning were found.
Likewise, hypothesized negative impacts were not observed on the inpatient service. The number of patients served, reflected in the number of discharges, remained stable over time. No changes in readmissions within 30 days were observed. Statistically significant decreases in length of stay were observed in both postintervention periods. No changes were observed in discharges to restrictive placements such as other acute psychiatric hospitals or jails. A statistically significant increase was observed in discharges to the state hospital, reflecting an increase from three discharges in the preintervention period to six in the period after the unit closure; in both periods less than 1% of all discharges were to the state hospital. Other changes in discharge dispositions were observed. There were fewer discharges to 24-hour care facilities and more discharges to hotels and shelters in both postintervention periods than there were in the preintervention period.
In terms of case mix, small but statistically significant postintervention increases were observed in the number of Asian patients seen in both the psychiatric emergency service and the inpatient service. The number of African-American patients seen in the inpatient service also decreased slightly after the unit closure. There were no other indications that capacity reductions differentially affected subgroups defined by age, gender, race-ethnicity, or diagnosis.
At a community level, reductions in acute inpatient capacity were not associated with changes in the number of suicides among community mental health clients. Similarly, capacity reductions do not appear to have been associated with an increase in the number of psychiatric evaluations conducted in the county jail. Available annual data indicated that the jail conducted 8,202 psychiatric evaluations and issued 490 involuntary psychiatric holds in the year before the closure of the inpatient unit (July 2007 through June 2008). Smaller numbers of evaluations were conducted (N=7,782) and involuntary holds issued (N=372) in the year after the unit closure (July 2008 through June 2009).
Time series analyses
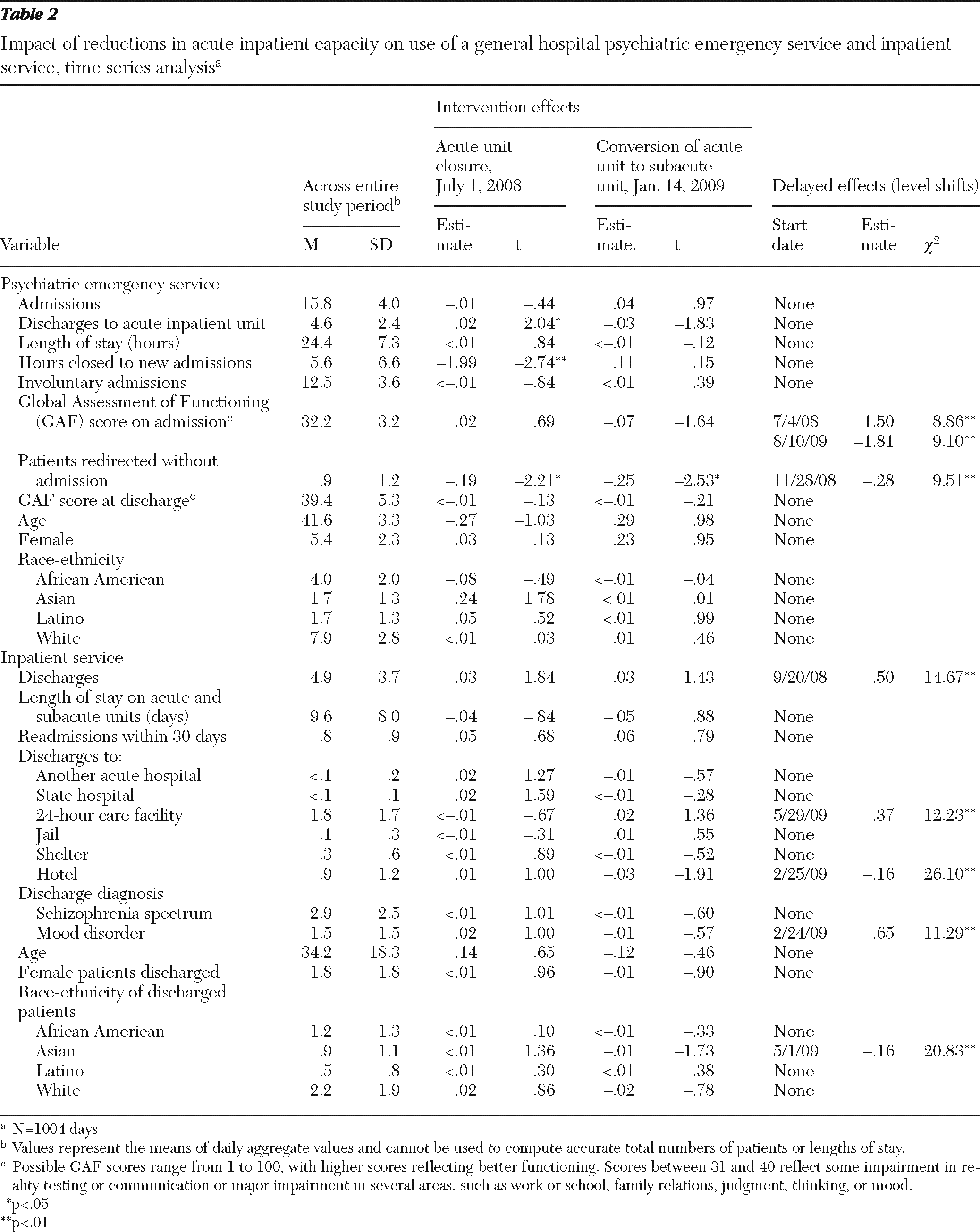
Time series analyses were conducted to statistically control for trends, cycles, and other background factors co-occurring with the two inpatient capacity reductions. These analyses, summarized in
Table 2, yielded results similar to the uncontrolled pre-post analyses and showed no evidence of hypothesized negative impacts in the emergency service, the inpatient service, or the community.
A few differences found in the uncontrolled pre-post comparisons were not found in the time series analyses, suggesting that these differences reflect stable trends toward change that were in progress before the inpatient capacity reductions and that continued after the reductions. Specifically, the time series analyses showed no association between capacity reductions and involuntary admissions to the psychiatric emergency service, inpatient length of stay, discharges to the state hospital or shelters, or the number of African-American patients seen on the inpatient service. Over the full study period, discharges to residential facilities were trending downward and discharges to hotels were trending upward. However, there were slight reversals in these trends after capacity reduction.
Time series analyses also revealed a few intervention impacts not detected in the pre-post analyses. Specifically, the number of patients seen on the inpatient service increased slightly after the unit closure, and there was a delayed increase in the number of patients with mood disorder diagnoses seen on the inpatient service one month after the subacute unit conversion.
Discussion
These findings from one urban safety-net setting suggest that it may be possible to reduce psychiatric inpatient capacity without negative impact. A 50% reduction in acute beds—and a 23% reduction in total beds—on an inpatient service that had been operating at full capacity was not associated with anticipated negative effects, such as increased demand for psychiatric emergency services, decreased access to emergency or inpatient services, increased recidivism to inpatient care, or increased levels of inadequately treated mental illness in the community. No patient subgroups defined by age, gender, race-ethnicity, or diagnosis appear to have been negatively affected.
The data presented here, however, provide only a limited view of the impact of inpatient capacity reduction. No data are available on the long-term impact on individual clients, in terms of their well-being, psychosocial functioning, or use of services outside the inpatient setting. In addition, available data on jail psychiatric evaluations do not provide a complete measure of criminal justice involvement.
Despite these limitations, evidence gleaned from this single experience with inpatient capacity reduction has the potential to inform strategic reductions in costly inpatient services elsewhere. The context for the capacity reductions studied differs from the contexts of published studies of capacity reduction in long-stay psychiatric hospitals in ways that merit particular attention. First, capacity reductions were not initiated because available capacity was underutilized; the original 79-bed inpatient service was operating at full capacity before the reductions. Second, capacity reductions were not implemented in concert with increases in alternative community services; reductions in inpatient capacity were necessitated by budget shortfalls that led to service reductions throughout the public mental health system. Third, there was no supply of private-sector inpatient services to offset reductions in the public sector. San Francisco's private-sector psychiatric inpatient capacity was reduced during the study period, and indigent, uninsured patients are not able to access private-sector inpatient care.
In this setting, strategic efforts to reduce inpatient length of stay were a key factor in buffering potential negative impacts of service changes. Over the 33-month study period, inpatient length of stay decreased by almost one-third, making it possible to serve the same number of patients with fewer resources. Although no new community resources became available to directly replace inpatient care, San Francisco has long had a range of outpatient mental health programs, including short- and long-term case management services that provide ongoing support to clients with severe and persistent mental illness. Reducing length of stay was an administrative priority, and inpatient clinicians were encouraged to make increasingly assertive efforts to collaborate with outpatient providers to identify community placement options and shorten inpatient stays. A key strategy involved initiating collaborative discharge planning soon after patients were admitted rather than waiting until they were ready for discharge. Another focus of planning was to combine intensive case management with temporary community placements in hotels or shelters. New agreements were negotiated with residential care facilities, allowing patients who needed long-term residential placement to be admitted from temporary community placements rather than wait in the hospital for openings to become available.
Several issues related to efforts to reduce length of stay warrant additional consideration. First, it is important to note that efforts to reduce length of stay were under way at SFGH before capacity reduction, although even with these efforts, the original service was operating at full capacity before the number of beds was reduced. Experience with strategies for reducing length of stay made it possible to pursue them more aggressively when capacity was reduced and to serve the same number of individuals with fewer beds. Attempting to initiate efforts to reduce length of stay at the same time as reducing capacity could constitute an insurmountable challenge. Second, reducing length of stay is unlikely to be a strategy that can be pursued indefinitely. The mean length of stay observed in the last quarter of the study period was eight days, which is comparable to the mean length of stay (8.2 days) observed in national data on mental health-related hospitalizations across a broad range of settings (
20). Given that SFGH serves a disadvantaged and complex patient population, stays somewhat longer than the national average might be warranted. Thus it is highly unlikely that future budget shortfalls can continue to be accommodated by further, progressive reductions in length of stay.
Conclusions
Data from a single urban safety-net setting indicate that it is possible to reduce acute psychiatric inpatient capacity without causing negative impacts on patients or the community. In this instance, it appears that demand for acute inpatient care was “elastic,” in that capacity was fully used when it was available, but when it was no longer available other options were found to meet patients' basic needs. In the studied setting, proactive use of existing community resources facilitated major reductions in inpatient length of stay that made it possible to serve the same number of patients with fewer inpatient beds. In other mental health systems, other types of adjustments may be more appropriate and equally or more successful in accommodating capacity reductions.
As multiple mental health systems face growing budget shortfalls and other resource constraints, further in-depth study of the impact of reductions in inpatient capacity is warranted. Examination of alternative strategies for reducing capacity in diverse service settings can usefully inform strategic resource allocation decisions that are tailored to meet local needs.
Acknowledgments and disclosures
The authors thank Michael Resnick for invaluable assistance in data acquisition and Dawn Kaiser, M.S.W., and Sita Patel, Ph.D., for helpful comments on the manuscript.
The authors report no competing interests.