Extensive research has examined the racial disparity in receiving appropriate conventional mental health treatment and potential explanations for such disparity. However, very little research has comprehensively examined the use of both conventional and unconventional mental health treatment by members of different racial and ethnic groups.
Current research consistently indicates that blacks and Hispanics are less likely than whites to seek mental health treatment when needed and are more likely to report unmet need for mental health services (
1–
6). This racial disparity remains even when controlling for socioeconomic status, health insurance, and severity of mental illness (
1,
3,
5,
7,
8). Racial disparities in use of psychotropic medication are especially great (
8,
9). Research has consistently found that blacks and Hispanics are less likely to receive a prescription for or to use psychotropic medication (
8–
11).
Unconventional medicine has been called “a far-flung landscape of diverse practices” (
12). Although the definition of unconventional medicine is open to some debate, for the purposes of this article, it is defined as “a group of diverse medical and health care systems, practices, and products that are not generally considered to be part of conventional medicine” (
13). In this article we make a crucial distinction between two types of unconventional treatment—complementary and alternative medicine (CAM) and parochial medicine. These two unconventional treatment types should not be understood as inflexible discrete categorizations but as a taxonomy or conceptual framework that helps to gain a clearer understanding of the use of unconventional treatment types by members of different racial and ethnic groups (
12).
Parochial treatment is defined in this article as a type of unconventional mental health treatment that appeals “to a specific religious group” and that “often lack[s] the markings of a health delivery system” (
12). CAM is distinguished from parochial medicine in that it is not associated with any religious beliefs. However, it is important to note that similar to parochial treatment, CAM practices often contain a spiritual component. Nevertheless, to focus on racial differences in religiosity and not in spirituality, this article treats religiosity and spirituality as separate constructs (
14,
15).
It is especially crucial to distinguish between these two types of unconventional mental health treatment because research consistently emphasizes the importance of religion in the black and Hispanic communities (
12,
16–
19). Another reason to study the use of CAM and parochial medicine separately is that blacks and Hispanics often face greater financial barriers to seeking needed mental health treatment (
1,
3,
7,
8). CAM is often quite expensive and rarely covered by even the most comprehensive insurance, but parochial treatment does not require payment (
5,
20–
23). Furthermore, research posits that members of racial and ethnic minority groups are less likely to seek mental health treatment when needed because of strong feelings of mistrust, fear, and skepticism toward Western “white medicine” (
2,
3,
8). Hence, the cultural barriers that prevent blacks and Hispanics from seeking conventional mental health treatment might also limit their use of CAM, which is mostly provided by and used by middle-class white females (
24). The use of parochial treatment is more consistent with the cultural and religious values of black and Hispanic racial and ethnic groups, which may increase trust in this means of treatment among members of those groups.
This study used pooled 2005–2007 data from the nationally representative National Survey on Drug Use and Health (NSDUH) to examine how race and ethnicity affect the type of conventional and unconventional mental health treatment sought by adults. We also consider other key factors in treatment-seeking behavior, including sex, socioeconomic status, health insurance, and severity of psychological distress. To determine whether the use of unconventional mental health treatment can partially account for the racial differences in the seeking of mental health treatment, this study addressed the following research questions: Does including parochial medicine as a type of mental health treatment reduce the racial disparity in treatment-seeking behavior? How does race affect the type of conventional and unconventional mental health treatment one seeks?
Methods
The NSDUH, sponsored by the Substance Abuse and Mental Health Service Administration, is an annual survey of a representative sample of the noninstitutionalized U.S. population over the age of 12. It is administered through a combination of computer-assisted personal interviewing and audio computer-assisted self-interviewing that focuses on alcohol and substance use behaviors as well as mental and general medical health. This study pooled data from 2005 to 2007 to ensure the largest possible subsample of blacks and Hispanics for examining use of unconventional mental health treatment. Pooling the data was appropriate because each year represents an independent, nationally representative, cross-sectional survey.
In addition the 2005 NSDUH was the first survey in a coordinated five-year sample design (2005–2009) that relied on a 50% overlap in second-stage units (area segments) between successive years. For this reason, the research used the 2005 survey and included survey data until 2007, the last survey for which data were available (
25).
A final survey weight was calculated by using the general exponential model to account for sampling and individual nonresponse bias to further ensure that the sample was as representative as possible of the targeted population (
25,
26). These survey weights were used in all analyses in this study. Because the research design required a focus on mental health treatment questions and measures of psychological distress that were asked of only adults, only a subsample of adults 18 or older was used. Additionally, because of insufficient sample sizes in all other racial or ethnic categories, the sample was further limited to non-Hispanic whites, non-Hispanic blacks, and Hispanics. Cases with missing data for any of the variables used in this analysis were eliminated.
To address whether including parochial medicine as a type of unconventional mental health treatment reduces the racial disparity in treatment-seeking behavior, design-based F tests and six logistic regressions were conducted for any mental health treatment, any conventional treatment, any psychotropic medication, any unconventional treatment, any CAM, and any parochial medicine on race. In order to examine how race affects the type of mental health treatment one seeks, we also conducted design-based F tests and an additional six logistic regressions for each possible single treatment type by race. All logistic regressions controlled for sex, age, education, income, insurance, and severity of psychological distress.
Severity of psychological distress was measured by the self-administered K6 screening scale for psychological distress. The K6 scale uses six questions regarding the extent of psychological symptoms experienced during a month in the past year when the respondent “was at his or her worst emotionally.” Possible scores range from 0 to 24, and a score of 13 or higher indicates serious psychological distress (
25). The K6 scale has been found to be a reliable and accurate measure of varying degrees of
DSM-IV mood or anxiety disorder among diverse populations (
27).
The dependent variables in this study were use of three types of nonexclusive mental health treatment—conventional treatment, excluding the use of psychotropic medication; psychotropic medication; and unconventional treatment. Respondents were classified as having sought conventional mental health treatment if they reported having received either conventional outpatient treatment other than psychotropic medication only or inpatient care at least once in the past year. Although the use of psychotropic medication is considered a type of conventional mental health treatment, for the aims of this study it was examined separately.
The use of unconventional mental health treatment was determined on the basis of responses to questions included in the 2005–2007 NSDUH. Respondents were asked whether they had received treatment from an acupuncturist, chiropractor, herbalist, massage therapist, or religious or spiritual advisor in the past 12 months for their emotions, nerves, or mental health. Respondents who reported seeking mental health treatment from a religious or spiritual advisor were classified as having sought parochial treatment; respondents who reported seeking all other types of unconventional treatment were classified as having sought CAM.
The research was reviewed and approved by the University of New Hampshire's Institutional Review Board for the Protection of Human Subjects in Research.
Results
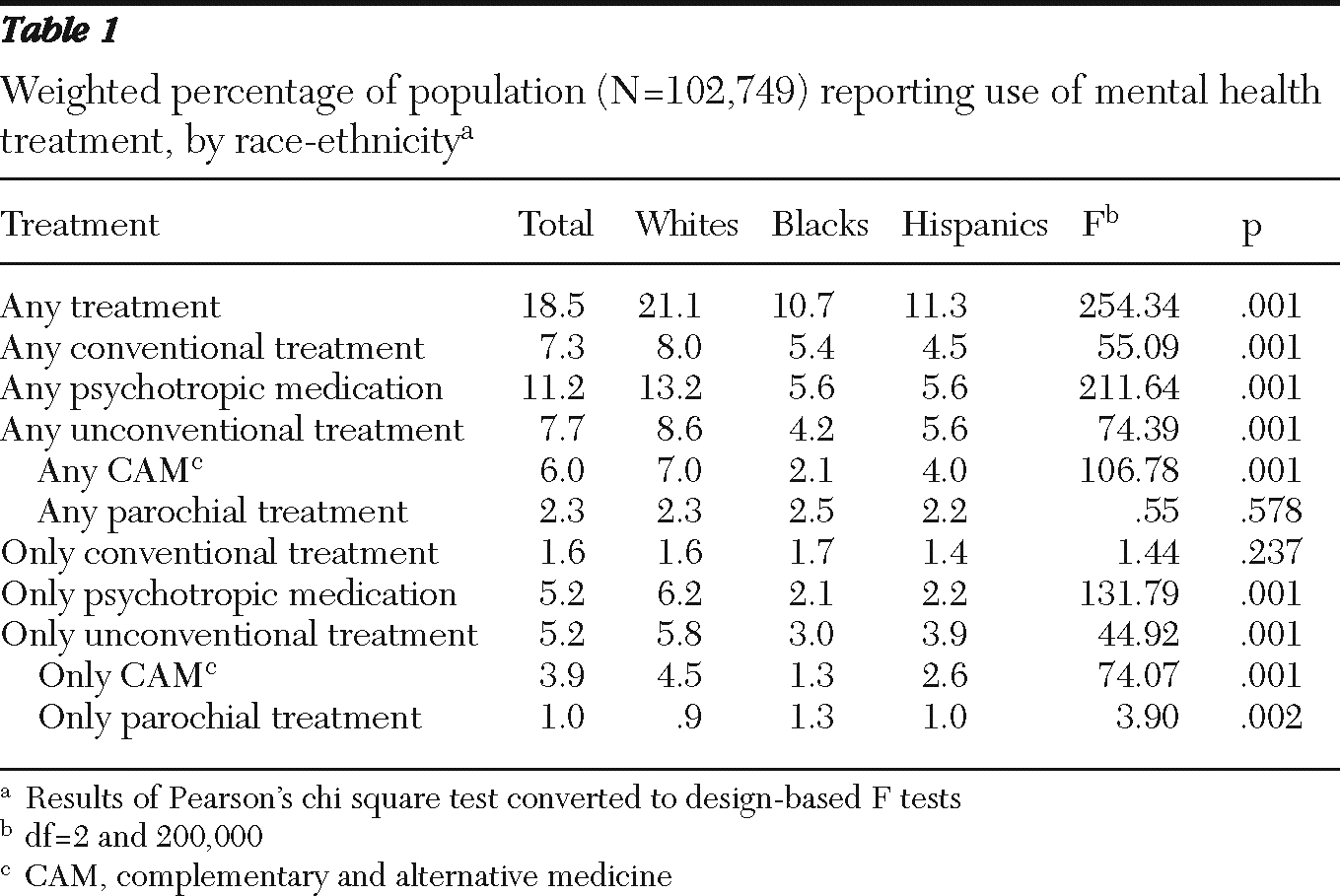
A final sample of 102,749 observations was used. A total of 74.1% of the sample were non-Hispanic white, 12.1% were non-Hispanic black, and 13.9% were Hispanic. The sample was 51.7% female, and 29.5% were between the ages of 26 and 34; 28.7% reported a total family income of $75,000 or more, 26% reported having a college degree, 11.1% met the criteria for serious psychological distress, and 83.4% reported having health insurance coverage in the past year. A total of 18.5% of the sample reported seeking any type of mental health treatment in the past year—7.3% reported the use of conventional mental health treatment, 11.2% reported the use of psychotropic medication, 7.7% reported the use of unconventional mental health treatment, 6.0% reported the use of CAM, and 2.3% reported the use of parochial treatment.
As shown in
Table 1, statistically significant relationships were evident between race and all treatment types except parochial medicine. Whites were significantly more likely than blacks and Hispanics to report seeking any treatment, any conventional treatment, any unconventional treatment, or any CAM. It is important to note that the relationship between race and the use of any parochial medicine was not statistically significant. Thus although blacks and Hispanics were generally less likely to seek treatment overall, they were equally as likely as whites to seek unconventional parochial medicine as a type of mental health treatment. A design-based F test of all three treatment types—conventional, psychotropic medication, and unconventional—by race and a design-based F-test of the two types of unconventional treatment—CAM and parochial medicine—by race confirmed these findings (analysis not shown).
Furthermore, as shown in
Table 1, whites were significantly more likely to use psychotropic medication, unconventional treatment, or CAM as their only form of treatment in the past year. On the other hand, blacks and Hispanics were significantly more likely than whites to report the use of parochial medicine as their only means of mental health treatment. Notably, there were no significant differences between blacks, whites, and Hispanics in using conventional mental health treatment as their only type of treatment.
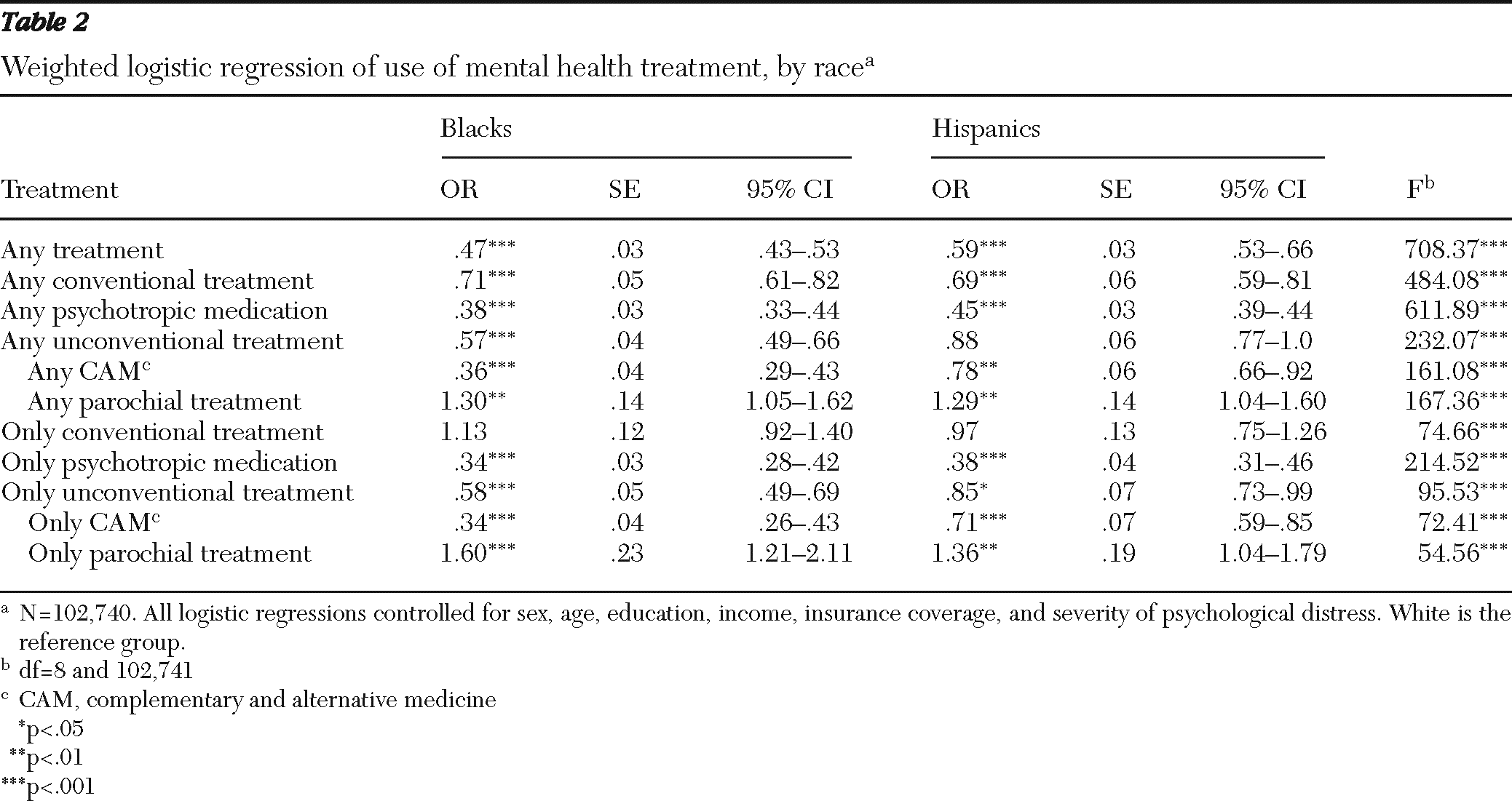
Table 2 presents odds ratios from a weighted logistic regression of treatment type on race that adjusted for key factors of sex, age, education, income, insurance coverage, and severity of psychological distress. Compared with whites, blacks had 53% lower odds and Hispanics had 41% lower odds of seeking any type of mental health treatment. Blacks had 29% lower odds and Hispanics had 31% lower odds than whites of seeking any conventional mental health treatment. Blacks had 62% lower odds and Hispanics had 55% lower odds than whites of using psychotropic medication as a type of mental health treatment.
Compared with whites, blacks had 43% lower odds of seeking any unconventional treatment and 64% lower odds of seeking any CAM in the past year. On the other hand, Hispanics were not significantly different from whites in their likelihood of using any unconventional treatment, but they had 22% lower odds than whites of seeking any CAM. Finally, compared with whites, blacks had 30% greater odds and Hispanics had 29% greater odds of seeking any parochial treatment in the past year.
Table 2 also presents odds ratios from a weighted logistic regression of the use of single treatment type on race that adjusted for the same key factors. There was no significant relationship between blacks, Hispanics, or whites and use of conventional treatment only. Compared with whites, blacks had 66% lower odds and Hispanics had 62% lower odds of using psychotropic medication only. Blacks had 42% lower odds of seeking unconventional treatment only and 66% lower odds of seeking CAM only compared with whites. Hispanics had only 15% lower odds of seeking unconventional treatment only and 29% lower odds of seeking CAM only compared with whites. However, compared with whites, blacks had 60% greater odds and Hispanics had 36% greater odds of seeking unconventional, parochial mental health treatment.
Discussion
It is crucial to consider all types of mental health treatment, both conventional and unconventional, to more accurately assess racial differences in treatment-seeking behavior. After adjustment for all other factors, this study found that blacks and Hispanics were significantly less likely to report seeking all types of mental health treatment except parochial medicine. In fact, blacks and Hispanics had approximately 30% greater odds than whites of seeking any parochial treatment in the past year.
Examination of the use of single treatment types showed that blacks and Hispanics were less likely than whites to report the use of medication only, unconventional treatment only, and CAM only but equally likely to seek only conventional mental health treatment. However, compared with whites, they are significantly more likely to report use of parochial medicine only as a type of unconventional mental health treatment. Hence, this suggests that unconventional parochial medicine may be more appealing than other treatment types to blacks and Hispanics.
These findings are consistent with research indicating that the use of parochial treatment as a type of unconventional mental health treatment may be more common among treatment-seeking blacks and Hispanics because of the greater importance of religion in their communities and because this type of treatment does not require payment (
16,
19–
21). Consistent with current research, these findings suggest that blacks and Hispanics may face cultural barriers of mistrust in seeking conventional and CAM mental health treatments.
Interestingly, the reasons often used to explain why blacks and Hispanics are more critical of and less likely to use conventional mental health treatment are similar to the reasons used to account for the overall use of unconventional medicine. In particular, research reveals that individuals commonly choose unconventional medicine because of its emphasis on holism and empowerment and because the values it espouses are complementary to their own (
28,
29). Little or no research has examined whether these attributes explain the variation in use of unconventional medicine by race or ethnicity. However, it is possible that only parochial treatment provides blacks and Hispanics with the advantages commonly attributed to unconventional treatment, which may explain its increased use among these groups.
The analysis also revealed that there were no significant racial differences in seeking only conventional mental health treatment in the past year. However, whites were significantly more likely to report the use of psychotropic medication only. Given that psychotropic medication is the most commonly used type of mental health treatment (
5,
30,
31), unwillingness to use this type of treatment among blacks and Hispanics is a crucial source of the treatment disparity. In fact, the well-established racial difference in the use of conventional mental health treatment may be mostly attributed to blacks' and Hispanics' aversion to the use of psychotropic medication.
This study is limited in that it was restricted to questions included in the 2005–2007 NSDUH data; this restriction limits the usefulness of several variables. For example, the use of mental health treatment was measured by the respondent's report of treatment used one or more times in the past year. Thus we could not differentiate between those who may have sought treatment only once and those who received more adequate treatment. In addition, data about the use of CAM and parochial treatment were derived completely from self-reports. Whether such treatment was as effective as conventional mental health treatment or even qualified as a type of treatment at all is beyond the aims of this study.
Finally, it is important to note that because the NSDUH is representative only of the noninstitutionalized U.S. population, those who were incarcerated or seeking inpatient mental health treatment at the time that the survey was administrated were excluded, which may have biased the findings. Regardless, the benefits of using the NSDUH greatly outweigh these limitations, given that no other large-scale, nationally representative data set contains as extensive information about conventional and unconventional mental health treatment.
Although this analysis showed that the use of parochial medicine did not decrease the racial disparity in mental health treatment-seeking behavior, it represents an important contribution to this body of literature. No other research to date has directly examined this issue by using a similarly inclusive definition of mental health treatment that incorporates both conventional and unconventional treatment and differentiates between CAM and parochial medicine. Hence, this study has the potential to serve as a starting point for future research by providing a new approach and theoretical framework.
Conclusions
The greater importance of religion in the black and Hispanic communities may both promote and hinder seeking appropriate mental health treatment. The cultural beliefs that encourage blacks and Hispanics to seek parochial medicine as a type of mental health treatment may also discourage them from using psychotropic medication; this paradox must be more clearly understood in order to decrease the racial disparity in treatment-seeking behavior.
Future research should evaluate whether unconventional types of mental health treatment are effective and if so, whether they are effective for all levels of psychological distress and types of mental illness. Furthermore, additional research should examine not only why blacks and Hispanics are more likely to use parochial medicine but also how this knowledge can be applied to overcoming cultural barriers that discourage racial minorities from seeking conventional treatment. In particular, qualitative interviews of respondents who use these types of unconventional mental health treatments would be a helpful next step in revealing how, why, and when participants access these types of treatments and how their use varies among blacks, Hispanics, and whites. This article is a first step in addressing how mental health treatment might eventually become equally accessible and appealing to everyone who needs it.
Acknowledgments and disclosures
The author thanks thesis advisor Heather Turner, Ph.D.; thesis committee members Karen Van Gundy, Ph.D., and Cliff Brown, Ph.D.; and everyone in Heather's spring 2010 publishing course for invaluable critiques, suggestions, and moral support.
The author reports no competing interests.