There has been considerable concern among clinicians and program planners that the distinctive service needs of older homeless adults have not been well characterized or addressed clinically. Until now, the focus of attention has been on the considerably larger population of younger homeless adults (
1–
4). Yet as the population of the United States ages and baby boomers approach older age, the proportion of homeless individuals who are older adults may increase, although the availability of Social Security may continue to keep their numbers disproportionately low (
5).
Estimates of the percentage of the overall homeless population who are over 55 vary widely, from 3% to over 20% (
1,
6), but are generally considerably lower than the percentage of the U.S. population (24.3%) represented by adults over 55 (
7). Homeless older adults are more likely than younger homeless adults to be Caucasian, to be male, and to have physical health problems (
1,
4,
8–
11).
Some studies have found high rates of mental illness (
12) and substance abuse (
13,
14) among homeless older adults. Previous studies have found that compared with homeless younger adults, homeless older adults are more likely to report alcohol dependence but less likely to report drug dependence, psychotic symptoms, and posttraumatic stress disorder (
1,
8–
10).
It has been estimated that between 25% and 33% of homeless adults have a serious mental illness (
15). Serious mental illness is a risk factor for homelessness (
16) and makes the treatment more complex and challenging (
17). Homeless older adults with a serious mental illness represent a vulnerable population that is in need of research-informed treatment. Identifying the unique needs and areas of poorer outcome of homeless older adults may facilitate the development of interventions designed to address their specific needs.
To date, research published about homeless older people has been based on small local samples assessed at one time point and thus has yielded inconsistent results (
1,
8–
10). This study used data from Access to Community Care and Effective Services and Supports (ACCESS), (
18), a large, 18-site national demonstration project that assessed the impact of efforts to increase service system integration for homeless adults with a serious mental illness. ACCESS was funded by the Center for Mental Health Services of the U.S. Department of Health and Human Services. It remains an important and informative study of homeless adults with mental illness because of its extensive assessment, large sample size, and longitudinal data collection.
This study used data collected by the ACCESS project to compare baseline variables by age group and then used multinomial logistic regression to identify independent characteristics that differentiated the oldest group and the younger groups at the time of program entry. Finally, after control for baseline differences detected by multinomial logistic regression, outcomes of the age groups over a 12-month follow-up period were examined.
Methods
Sample and procedures
Data were obtained from the ACCESS program public database. Data collection took place between 1994 and 1998. All ACCESS clients received intensive case management services. Of the 18 data collection sites across the country, nine were given extra resources to increase system integration. The results indicated that although the nine experimental sites showed increased service system integration, there were no differences in client improvement at the experimental and the control sites (
19).
Participants were eligible if they had spent at least seven of the previous 14 nights at an emergency shelter, outdoors, or in a public building; had been identified as having a serious mental illness by a 30-item screening algorithm developed for a previous homelessness outreach study (
20); and were not engaged in more than minimal mental health treatment. Serious mental illness was defined as having symptoms of depression, mania, or psychosis, on the basis of self-report, or having been observed by an interviewer to have symptoms of psychosis unrelated to substance use. All sites had specialized community outreach teams to recruit homeless people with an untreated mental illness.
Written informed consent was obtained from all participants. Structured interviews were conducted at baseline and at three- and 12-month follow-ups.
Measures
Psychometric information and methods for confirming treatment fidelity were reported in a previous publication (
19). Demographic information about gender, race, years of education, marital status, employment, and money earned during the previous month was collected. Homelessness was assessed on the basis of sleeping location during the previous 60 nights. Literal homelessness was defined as sleeping outdoors, in an abandoned or public building or automobile, or at an emergency shelter. Being housed was defined as living in a hotel, boarding home, halfway house, residential program, institution, jail, or one's own or another's residence. Data about the individual's age during the first episode of homelessness, number of episodes of homelessness, and lifetime years of homelessness were also collected.
Psychiatric symptoms, alcohol use, drug use, and history of a suicide attempt were assessed with the relevant subscales of the Addiction Severity Index (ASI), a measure found to be valid with older adults (
21,
22). Scores range between 0 and 1, with higher scores indicating more severe symptoms. The ASI psychiatric score is calculated by equally weighing 11 questions about symptoms of sadness or anxiety, hallucinations, suicidal ideation, suicide attempt, whether one is currently prescribed psychiatric medication, and how much one is bothered by psychiatric symptoms. The ASI alcohol score is calculated by equally weighing six items about the number of days in the past 30 days one drank alcohol and felt drunk and the amount of money spent on alcohol, how much one is bothered by alcohol problems, and how important one feels it is to get treatment for these problems. The ASI drug score is calculated by equally weighing 11 items assessing over the past 30 days the number of days of use, the amount of money spent, and withdrawal symptoms related to several illegal drugs and how much one is bothered by drug problems and how important one feels it is to get treatment for these problems.
Selected items of the Diagnostic Interview Schedule (
23) and the Psychiatric Epidemiology Research Interview (
24) were used to create three composite scores: a depression score, a psychosis score, and an interviewer observation of overtly psychotic behavior. The depression score summed the number of depression symptoms reported by an individual from among a list of five symptoms that included depressed mood or decreased interest or pleasure, trouble concentrating, feelings of worthlessness or guilt, thoughts about death, and psychomotor agitation. The psychosis score assessed the frequency of ten psychosis symptoms; each symptom had a maximum value of 4 points, for a maximum total of 40 points. The interviewer-observation score represented the number of behaviors suggestive of psychosis, such as responses to internal stimuli, out of a possible 13, that were observed during the interview. Each behavior is rated on a scale of 0, not at all, to 4, a large extent, for a maximum score of 52.
Physical health was assessed by the total number of medical disorders endorsed from among a list of 17. Subjective health status was assessed with the question, “Compared to other people your age, would you say your health is excellent, very good, good, fair, or poor?”
Social support network size was calculated as the total number of people available from a list of nine roles, such as parent or friend, to help with three types of problems (short-term loan of $100, ride to an appointment, and someone to talk with if feeling suicidal), for a maximum total of 27 points (
25). Social support satisfaction was calculated as the average response to nine questions derived from the Lehman Quality of Life Interview, each rated from 1, terrible, to 7, delighted (
25). Quality of life was measured with a single item from the Lehman Quality of Life Interview (
26), “Tell me how you feel about your life overall right now,” scored on the same scale. A composite satisfaction with safety score was calculated by averaging a client's ratings in five categories of safety, from 1, terrible, to 7, delighted.
Early-life instability was assessed with the Family of Origin Instability Scale (
27), a 12-item scale that includes questions about family history before the client's 18th birthday, including history of abuse and financial difficulties. History of antisocial behavior was assessed with the Helzer Conduct Disorder Scale (
28), which includes nine yes-or-no questions that are based on the
DSM-III criteria for conduct disorder. Past legal involvement was assessed with questions from the ASI (
21).
Statistical analysis
Kruskal-Wallis and chi square analyses were used to compare baseline data among young (age 18 to 34), middle-aged (age 35 to 54), and older (age 55 and older) participants because of nonnormal distributions and nonequivalent distributions between groups. Significant Kruskal-Wallis results were analyzed for post hoc between-group differences with the Mann-Whitney U test. Effect size was calculated by using Cohen's d.
The homelessness research literature supports the use of a relatively young age to demarcate “older adult,” because homeless adults resemble nonhomeless adults who are ten to 20 years older (
6,
29). Multinomial logistic regression was used to identify characteristics that independently differentiated older homeless adults from the younger groups.
Next, baseline characteristics of the subgroups with and without follow-up data were compared to identify potential biases in the follow-up sample. Finally, after adjustment for potentially confounding baseline differences identified by multinomial logistic regression, a mixed-model analysis was used to compare outcomes between age cohorts at three-month and 12-month follow-ups.
Results
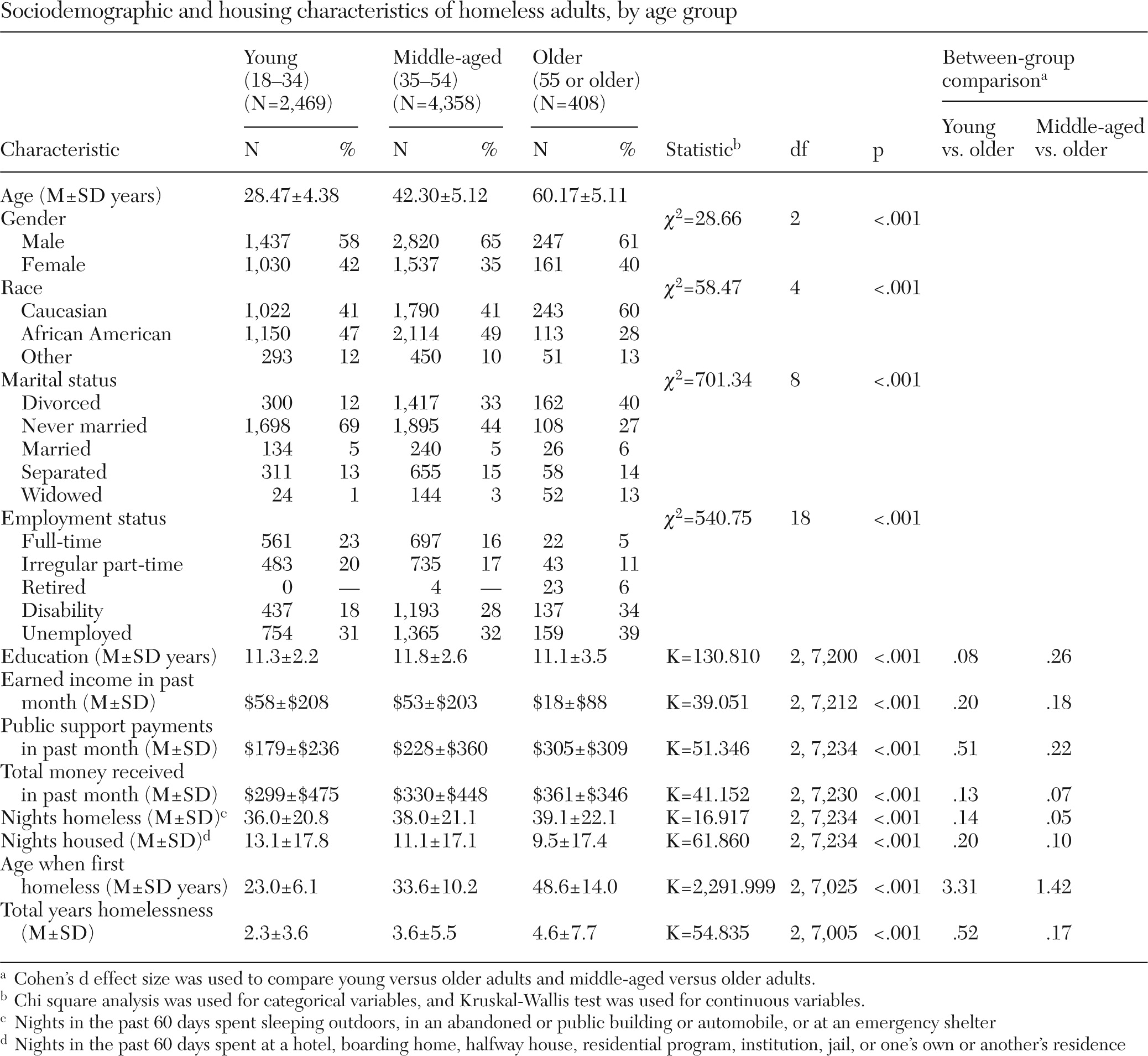
Baseline data were available for 7,235 clients. A total of 2,469 were age 18 to 34 and 4,358 were age 35 to 54. There were 408 adults age 55 or older. Of the older sample, 230 (56%) people were age 55 to 59, and 156 (38%) were age 60 to 69. A total of 20 (5%) individuals were age 70 to 79; one client was 85, and one was 95.
Baseline assessment
Table 1 provides a summary of demographic and homelessness characteristics at baseline. Primarily the older adults were male (61%), Caucasian (60%), and unmarried (94%).
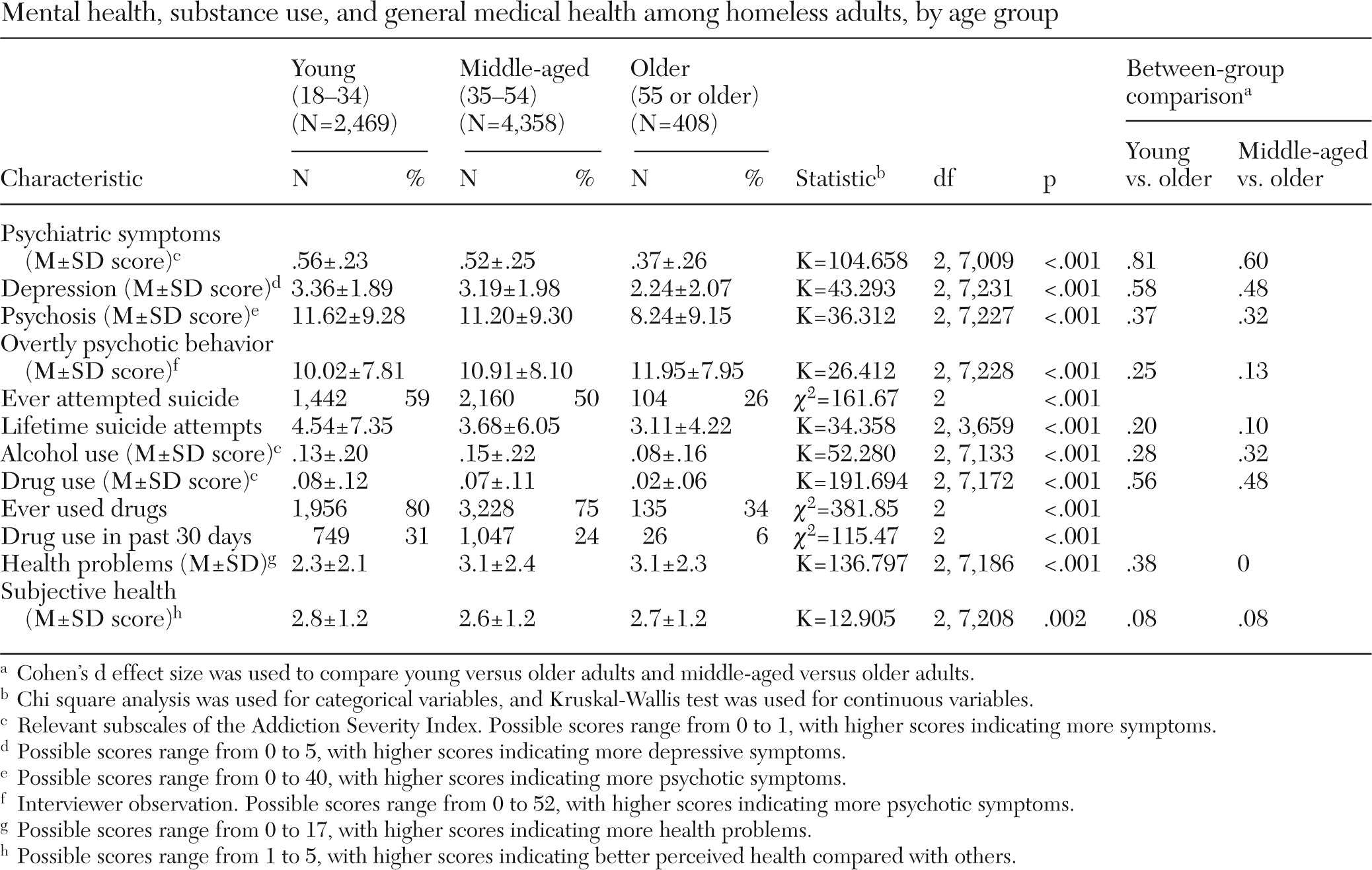
Table 2 summarizes mental health, substance use, and physical health variables at baseline. Compared with members of the other age groups, the older adults reported significantly fewer symptoms of depression and psychosis and significantly fewer general psychiatric symptoms (ASI psychiatric score). The effect sizes were largest for general psychiatric symptoms. History of a suicide attempt was prominent among all three age groups—young (59%), middle-aged (50%), and older (26%). The ASI score for alcohol use was lowest among the older group; the ASI score for drug use was highest among the young group and lowest among the older group. The number of medical conditions endorsed by the older adults was equivalent to the number endorsed by the middle-aged adults but more than the number endorsed by the young adults.
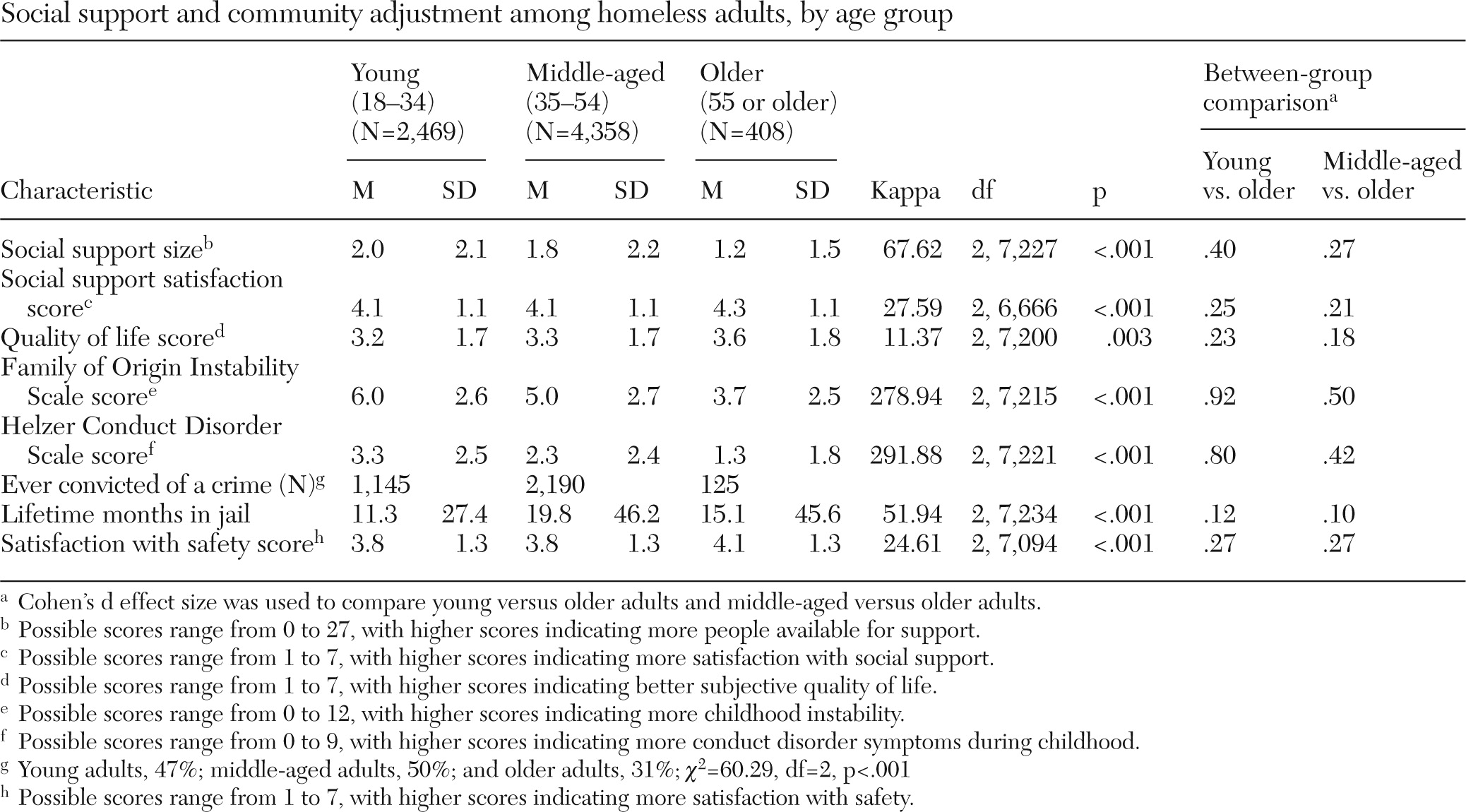
Table 3 summarizes social support variables at baseline. Compared with participants in the younger age groups, the older adults had the fewest social supports but expressed greater satisfaction with them. The older adults reported higher quality of life and higher satisfaction with safety. They had the most childhood stability and the fewest conduct disorder symptoms.
Multinomial logistic regression was used to identify independent significant differences between age groups (the older adults were the reference group). The variables found to be significantly different were data collection site, work status, marital status, gender, depression score, years of education, money received through public support, years homeless, psychosis score, history of suicide attempt, number of medical problems, Family of Origin Instability Scale score, Helzer Conduct Disorder Scale score, and social support network size.
Outcome assessment
Sample representativeness.
A total of 331 of the older adults, 81% of the original sample, were available for 12-month follow-up. Compared with those who were not available at follow-up, the older adults assessed at the follow-up were older by approximately two years and had worse social support satisfaction, greater instability in their family of origin, and more drug use (data available on request). At 12-month follow-up, middle-aged adults (N=3,513, 81%) had fewer lifetime years homeless and more medical and psychiatric problems than those not available for follow-up. Young adults who were available at the 12-month follow-up (N=1,925, 78%) had more lifetime suicide attempts than young adults who were not available at the follow-up.
Alcohol and drug use scores of those who were retained in the study were compared with scores of those who dropped out. There was no significant effect for alcohol use score, but those who dropped out of the study had a slightly higher drug use score than those who continued to participate for 12 months. No adjustment was made for baseline differences in alcohol and drug use by the two groups, which may represent a limitation to the analysis.
Outcomes.
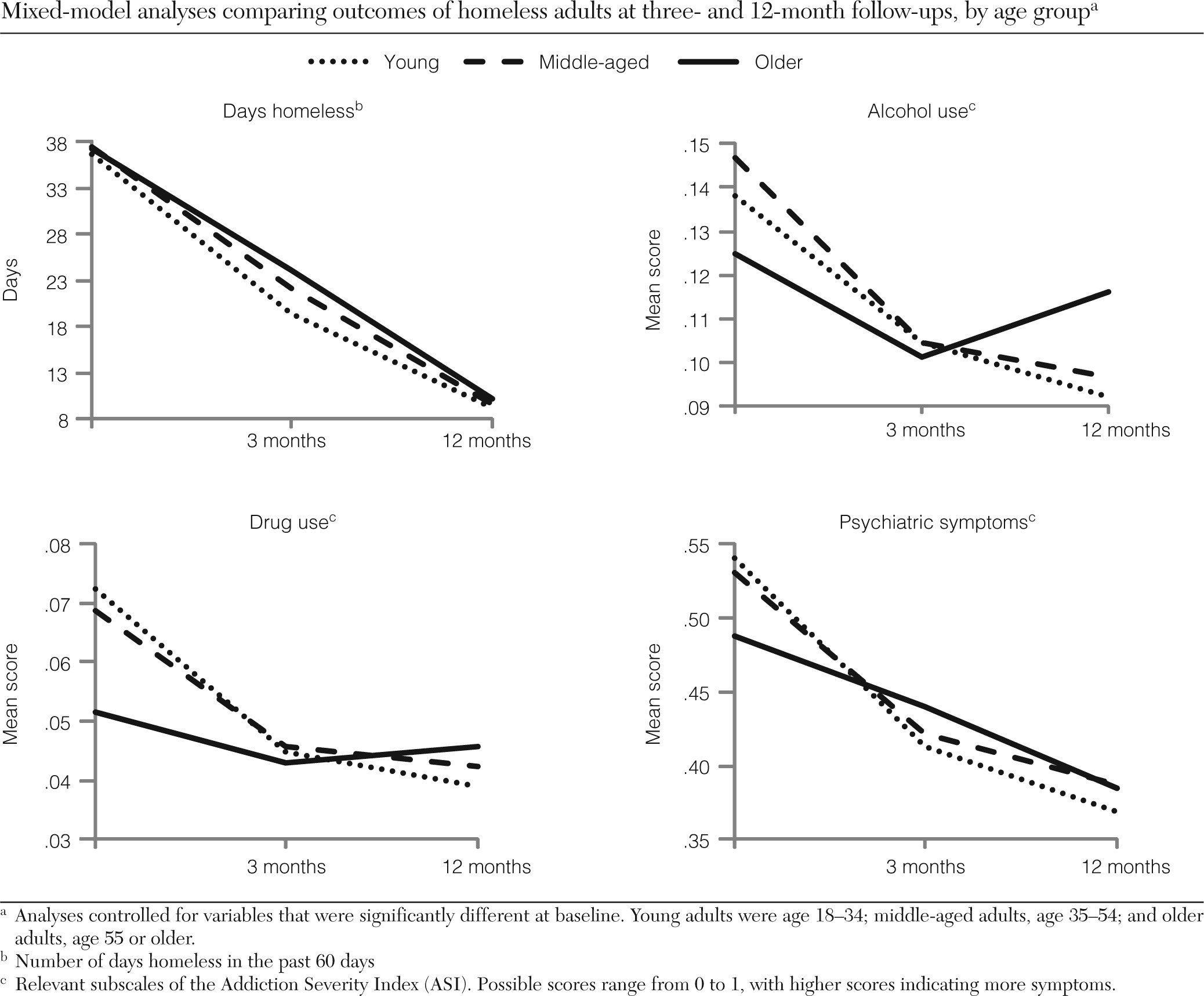
The mixed-model analysis compared the three age groups at three time points (baseline and at three-month and 12-month follow-ups) after adjustment for all baseline variables found to be significantly different in the multinomial logistic regression (
Figure 1). All age groups had a decrease in days homeless over the one-year period (age effect, F=8.74, df=2 and 18,000, p<.001; time effect, F=1,186.94, df=2 and 18,000, p<.001; and interaction of time × age, F=4.02, df=4 and 18,000, p=.003). At three-month follow-up, older adults had significantly more days homeless than the other age groups (
Figure 1).
The older adults had the lowest alcohol use score at baseline, but they had the highest score at one-year follow-up, given that use declined faster among the younger age groups and use among the older clients increased from three months to one year (time effect, F=52.18, df=2 and 18,000, p<.001; interaction of time × age, F=3.97, df=4 and 18,000, p=.003) (
Figure 1). The same pattern was observed for drug use score, with the older adults having the lowest scores at baseline but the highest scores at one-year follow-up (time effect, F=72.74, df=2 and 18,000, p<.001; interaction of time × age, F=6.32, df=4 and 18,000, p<.001). On the ASI psychiatric score, the older adults had the lowest score at baseline, and the score decreased over time for all age groups. The rate of decline was significantly greater among both groups of younger adults and greatest for the youngest adults versus the older adults (time effect, F=362.88, df=2 and 18,000, p<.001; interaction of time × age, F=10.30, df=4 and 18,000, p<.001). At one-year follow-up, young adults had the lowest ASI psychiatric score of any age group.
There was also a significant main effect for data collection site, but it did not have an impact on the significant interaction effects for age and days homeless, ASI psychiatric score, drug use score, and alcohol use score. There were no significant interactions of time and age group on any other outcome, including depression score, public support payments, subjective health, quality of life, and suicide attempt.
Discussion
This study found that at baseline, homeless adults who were older consistently had better mental health and fewer, but more satisfying, social supports than the younger groups. Over a one-year period, all age groups experienced a decrease in days homeless. The older adults had the lowest substance use and psychiatric scores at baseline, but over time the other age groups experienced more rapid and larger decreases of such scores. At the one-year mark, young adults had the lowest scores for substance use and psychiatric symptoms. Although differences in the scores of the three age groups over time were statistically significant, the change in ASI psychiatric score was more clinically meaningful than the changes in ASI drug and alcohol scores.
At baseline, the older adults had markedly less current and lifetime substance use than the younger age groups. Although the age differences were statistically significant for alcohol and drug use, the effect size was larger for drug use. Over time, substance abuse by the two groups of younger adults decreased sharply, but among the older adults, substance use decreased by the three-month follow-up but had returned to its original levels at the one-year follow-up. Overall, the rate of substance use by the older adults was relatively low compared with rates of substance use reported by other studies of homeless and nonhomeless older adults (
30). Two other studies found that homeless older adults had lower rates of drug use, but higher rates of alcohol use, compared with younger adults (
8,
9).
In interpreting the data, it is important to consider the greater impact of a given amount of alcohol on an older adult because of age-related changes in the metabolism of alcohol (
31,
32) and the increased risk for adverse alcohol-medication interactions among older adults because of the increased use of medications (
33).
This study found that older adults had the lowest ratings for overall psychiatric symptoms at baseline but that these age differences disappeared at one-year follow-up because of more rapid improvement among the two younger groups of adults. Past research has found that among homeless adults, rates of psychosis symptoms were lower among older versus younger adults but that rates of other psychiatric symptoms among the two groups were comparable (
8,
9).
Lifetime history of suicide attempt was more likely to be reported by the younger groups of homeless adults. Among nonhomeless samples, older adults are among the age groups with the highest rates of completed suicide, and among older adults, Caucasian men have the highest rates of completed suicide. Yet older adults have the fewest nonlethal attempts (
34,
35). The relatively lower rates of past suicide attempts among the older subsample of this study might be due to a combination of better mental health at baseline and a greater likelihood that suicide attempts would be successful.
The longitudinal data show that among older adults, substance use scores improved at a slower rate or did not change compared with the scores of young and middle-aged adults, who demonstrated improvements in substance use scores and across all of the primary measures of outcome. Although the mixed model controlled for baseline differences, it is possible that the lower levels of substance use at baseline among the older adults had an impact on the data analysis. Interpretation of age-related longitudinal changes in substance use should be cautious given the small significant changes. The reasons for these age differences are unclear but may reflect that younger people possess greater behavioral malleability or that current interventions lack efficacy in addressing the specific needs of homeless older adults.
Methodological limitations of this study include the exclusion of homeless adults without mental health diagnoses, selection bias, time elapsed since data collection, lack of cognitive assessment, and incomplete follow-up rates. Given the study's inclusion criteria, the results are applicable only to homeless adults with a mental health diagnosis who are willing to participate in an intervention project; however, that is clearly the population of greatest concern to mental health practitioners.
The ACCESS data collection, dating from 1994 to 1998, are now over a decade old, and cohort effects may be relevant. However, such effects are unlikely to account for all of the age-related differences found by this study. There has been research predicting that the baby boomer cohort will lead to an increase in substance use among homeless older adults (
36). Recent research has shown an increase in drug-related admissions and a decrease in alcohol-related admissions among older adults, but alcohol dependence remains the most common substance use diagnosis among older adults (
37).
Although there have been some increases in homeless services since the data were collected, going forward, budget cuts may cause future services to resemble those of the past; in addition, the ACCESS study provided participants with greater services than were available in the community, thus creating a treatment environment similar to what is available in the community currently. The older data remain valuable because they represent the largest collection of longitudinal data about homeless older adults with mental illness, a subgroup that is rarely studied.
Conclusions
This study found that among homeless adults with mental illness, the older clients scored lower than younger clients on baseline measures of mental health and substance use and higher on baseline measures of social adaptation, reflecting less severe problems. Over a one-year period of active community-based case management, housing improved substantially for all age groups. The comparison of psychiatric and substance use variables between age groups showed a distinct pattern of difference, however, with lower severity at baseline and less improvement over time among the older adults. In particular, the lack of improvement in alcohol use over time among the older adults suggests a need for interventions tailored for their age group; these age-related longitudinal findings would be strengthened through replication in future research.
Although the differences in baseline and longitudinal outcomes among age groups were statistically significant, the small magnitude of the differences suggests that some may not be clinically meaningful and that one must be cautious in drawing implications for clinical service delivery or policy. For example, treatment of homeless adults may justifiably emphasize outcomes such as drug use, given the high rates of drug use on average among the homeless population. However, treatment of homeless older adults may be improved by focusing on utilizing these individuals' small but high-quality social support networks and other strengths that allow for survival in a high-risk environment.
Acknowledgments and disclosures
The authors report no competing interests.