About one in five American adults smokes cigarettes (
1), even though cigarette smoking is the leading preventable cause of premature deaths in the United States (
2). Recent studies of smoking among individuals with schizophrenia and other severe mental illnesses have estimated that 52%–62% of adults with severe mental illnesses are current smokers (
3–
5), which is two to three times the rate in the general population. Studies have shown that among persons with severe mental illnesses, those who smoke are more likely to be white, to have hypertension, and to report greater stress, poorer quality of life, and lower satisfaction with various life domains than those who do not smoke (
6).
It has been suggested that many mental health providers believe that patients with mental illness use tobacco as an effective form of self-medication or coping, are not interested in stopping smoking, and think smoking is a low-priority concern in the face of psychiatric symptoms (
7). Yet recent studies suggest that these beliefs may be unfounded, and randomized controlled trials of tobacco cessation treatment integrated with mental health treatment have found that this integrated approach did not exacerbate psychiatric symptoms and can be effective in reducing cigarette smoking (
8–
10). Moreover, smoking cessation should not be regarded as a low priority in any mental health care setting because people are far more likely to die from tobacco-related diseases than from mental illness.
Less attention has been paid to another vulnerable segment of the population—chronically homeless adults—many of whom have severe mental illness or addiction problems. In the past, tobacco companies have placed a special marketing focus on homeless people, for example, by distributing free cigarettes at homeless shelters or giving away blankets with cigarette brand logos (
11,
12).
The 2003 Health Care for the Homeless User Survey found that 73% of homeless adults were current smokers, 9% had quit smoking during their lives, and 54% reported receiving advice from a health professional to quit (
13). Homeless adults with more numerous homeless episodes were more likely than others to have been advised to quit but were less likely to have successfully quit. Only a few other surveys of homeless adults have addressed smoking. One nine-site survey found that 69% of homeless adults were current smokers and 37% reported readiness to quit within the next six months. Those who had tried to quit in the past and those who had social support to quit were more likely to quit smoking. Nicotine replacement was found to be the most commonly preferred assistance method, and self-efficacy beliefs about quitting were greater when assistance was available (
14). Similarly, a small survey of homeless smokers in Massachusetts found that 44% were interested in smoking cessation counseling, and measures of self-efficacy and social support were associated with readiness to quit smoking (
15). One study that compared homeless and nonhomeless smokers found that homeless smokers were more likely to be white, to smoke more cigarettes, and to have started smoking at a younger age (
16). The study also found that both nonhomeless and homeless smokers understood the risks of smoking and benefits of quitting to a similar degree, but homeless smokers were less likely to be ready to quit smoking. Focus groups have reported that boredom and stress are common reasons for continued smoking, which is facilitated by the fact that tobacco use is accepted in many homeless settings (
17).
This study aimed to describe the prevalence rate of smoking among a large multisite sample of adults with chronic homelessness, identify sociodemographic and clinical correlates of smoking in this sample, and examine rates of change and predictors of change in smoking behaviors over one year in supported housing.
Methods
Sample
Data were examined for 754 chronically homeless adults at 11 sites that participated in a federal initiative called the Collaborative Initiative to Help End Chronic Homelessness (CICH) (
18). Data were collected from 2004 to 2009, and the program was focused on providing adults who were chronically homeless with permanent housing and supportive primary health care and mental health services. The 11 sites funded through CICH included Chattanooga, Tennessee; Chicago; Columbus, Ohio; Denver, Colorado; Fort Lauderdale, Florida; Los Angeles; Martinez, California; New York City; Philadelphia; Portland, Oregon; and San Francisco. Chronically homeless adults were defined as “an unaccompanied homeless individual with a disabling condition who has either been continuously homeless for one year or more or has had at least four episodes of homelessness in the past three years.”
Homeless adults were recruited by clinical staff at each site through community outreach. Each site developed a comprehensive plan to provide permanent housing, increase the availability of medical and mental health services, and ensure the sustainability of these efforts. There was no specific focus on smoking cessation treatment. All participants gave informed consent, and assessments were conducted by independent, trained evaluation staff at each site through interviews and self-report measures. Assessments were conducted at baseline and every three months until the 12-month follow-up. Participants were paid $15 per assessment, and procedures were approved by institutional review boards at each participating site.
Measures
Sociodemographic characteristics and diagnoses.
Data on age, gender, race-ethnicity, education, marital status, veteran status, and mental and substance use disorders were collected from participants by use of a structured form.
Smoking status.
Participants were asked to describe their use of cigarettes in the previous three months with one of four responses, which were categorized into three smoking groups: nonsmoker (“I do not smoke”), self-limiting smoker (“I smoke, but I constantly try to reduce the number of cigarettes” or “I smoke, but I try not to smoke more than a certain number of cigarettes per day or week”), or regular smoker (“I smoke whenever I feel like it without counting the number of cigarettes.”). An additional item asked participants (yes-no) whether they had discussed smoking with a health care professional in the past year.
Employment and income.
Participants were asked the duration of their longest full-time job, how many hours they worked per week in the past month, and how much pay they received for work done in the past month. Participants were also asked the amount of public support income (for example, Social Security disability benefits, food stamps, and compensation from the Department of Veterans Affairs) they received in the past month.
Residential history.
Participants were asked about their lifetime history of homelessness and incarceration. Participants were also asked the number of nights that they stayed in the past three months in various settings, which were categorized into three categories: in own place (own apartment, room, or house), in an institution (halfway house, transitional housing, hospital, or jail), or homeless (shelter, outdoors, in a vehicle, or in an abandoned building).
Clinical status.
The Medical Outcomes Study Short Form–12 (SF-12) (
19) was used to assess physical and mental health. The psychoticism, depression, and anxiety subscales of the Brief Symptom Inventory (
20) were selected to measure subjective distress. The Addiction Severity Index (ASI) (
21) was used to assess alcohol and drug use in the past month.
Health service use.
Participants were asked the number of medical, mental health, and substance abuse treatment visits they made during the past three months.
Quality of life.
Subjective quality of life was assessed with one item from the Lehman Quality of Life Interview (
22). Social support was assessed by calculating the mean number of types of persons (clergy, roommate or neighbor, friend, service provider, adult child, spouse or significant other, sibling, other family member, or parent) that participants could “have counted on” in each scenario: short-term loan of $100, a ride to an appointment, or assistance if they felt suicidal (
23). Community integration was assessed with a measure that asked about participation in 16 common activities in the past two weeks, which was summed for a total score (
24).
Data analysis
Given the aims of the study, a large number of exploratory analyses were conducted. To reduce the possibility of inflated type I error, multivariate analyses were conducted with only significant variables identified in preliminary univariate analyses.
Smoking groups were compared on baseline characteristics with analyses of variance and chi square tests. Post-hoc group comparisons were made with Fisher's least-significant-difference test and pairwise chi square tests. A stepwise multinomial regression model was used to identify baseline variables independently associated with each of the three smoking groups at baseline. Forward stepwise selection was used based on the likelihood ratio statistic.
Participants' change in smoking group status was examined over a one-year period, and a chi square test for trend was conducted to examine the significance of the changes. The proportion of participants in each smoking group at baseline and 12 months was also compared. Change scores in smoking group, along with change in scores on the ASI alcohol and drug subscales over one year were created by subtracting baseline from one-year scores. Smoking group was treated as a three-level interval variable. Partial correlations between change in smoking group and change in other substance use were evaluated, with control for baseline substance use status. A linear mixed regression analysis was also conducted to examine the association of smoking group and scores on the ASI alcohol and drug subscales over time for all time points. Baseline scores on these subscales were controlled for, and an autocovariance structure was specified.
Finally, change in smoking group over one year was coded into a binary outcome variable—quit or limited smoking versus no change or increased smoking. A stepwise binary logistic regression analysis, using forward selection with the likelihood ratio statistic, was conducted to identify variables independently associated with quitting or limiting smoking during the one-year period of study in supported housing. All baseline variables and ASI change scores were included in the model.
Results
Of 754 participants who responded at baseline, 152 (20%) reported that in the past three months they had not smoked, 290 (38%) reported smoking but limiting themselves, and the largest group of participants, 312 (41%), reported regularly smoking with no limitations. A total of 449 participants (60%) reported that they discussed smoking with a health care provider in the past year. Thus, among the 602 participants who reported smoking, 48% tried to limit their smoking and 75% discussed smoking with a health care provider.
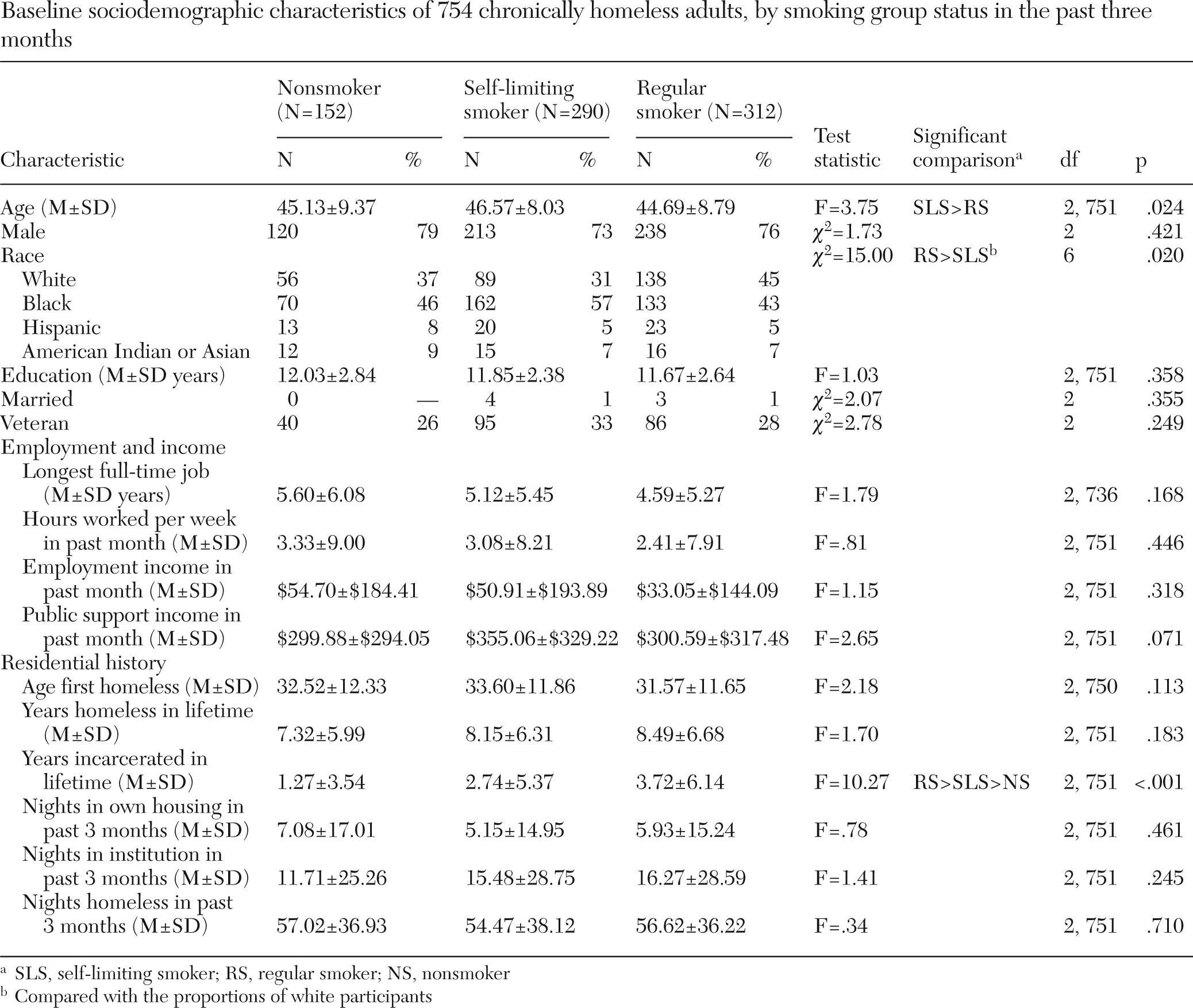
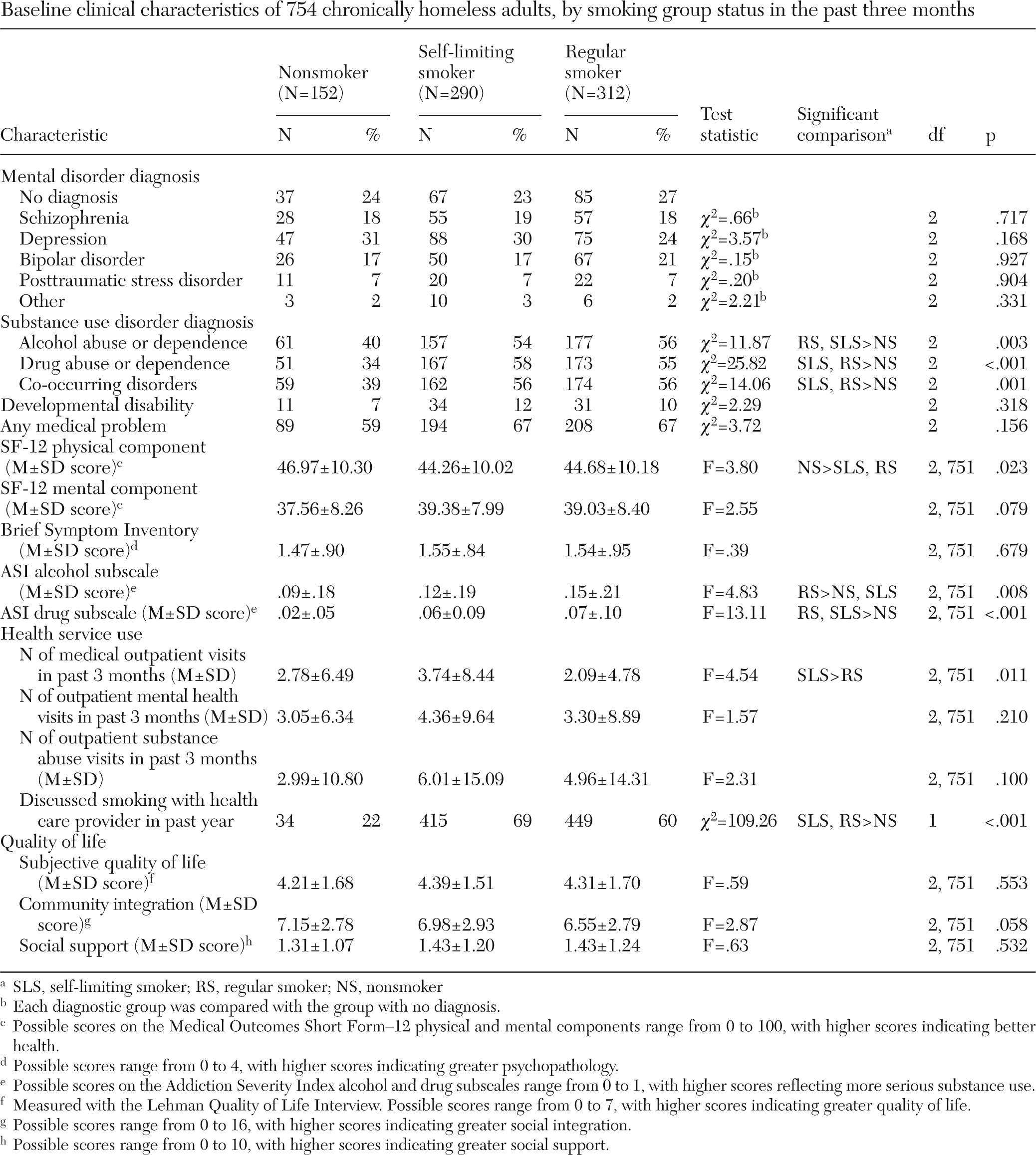
Several univariate differences in baseline characteristics were found between the three smoking groups (
Table 1 and
Table 2). The self-limiting smokers were older than the regular smokers; the regular smokers reported more years of lifetime incarceration and were more likely to be white than the self-limiting smokers; and the self-limiting smokers reported more years of incarceration than the nonsmokers. Nonsmokers had higher SF-12 physical component scores (indicating better health) than self-limiting and regular smokers. But there were no differences in diagnoses of mental disorders (excluding substance abuse diagnoses), employment, income, residential history, or quality of life.
Compared with nonsmokers, regular smokers and self-limiting smokers were more likely to have a diagnosis of alcohol abuse or dependence, a diagnosis of drug abuse or dependence, a dual diagnosis, and higher scores on the ASI drug subscale. Among the three smoking groups, regular smokers had the highest scores on the ASI alcohol subscale and self-limiting smokers reported a greater number of medical outpatient visits in the three months before baseline. As expected, both self-limiting smokers and regular smokers were more likely to have discussed smoking with a health care provider in the past year.
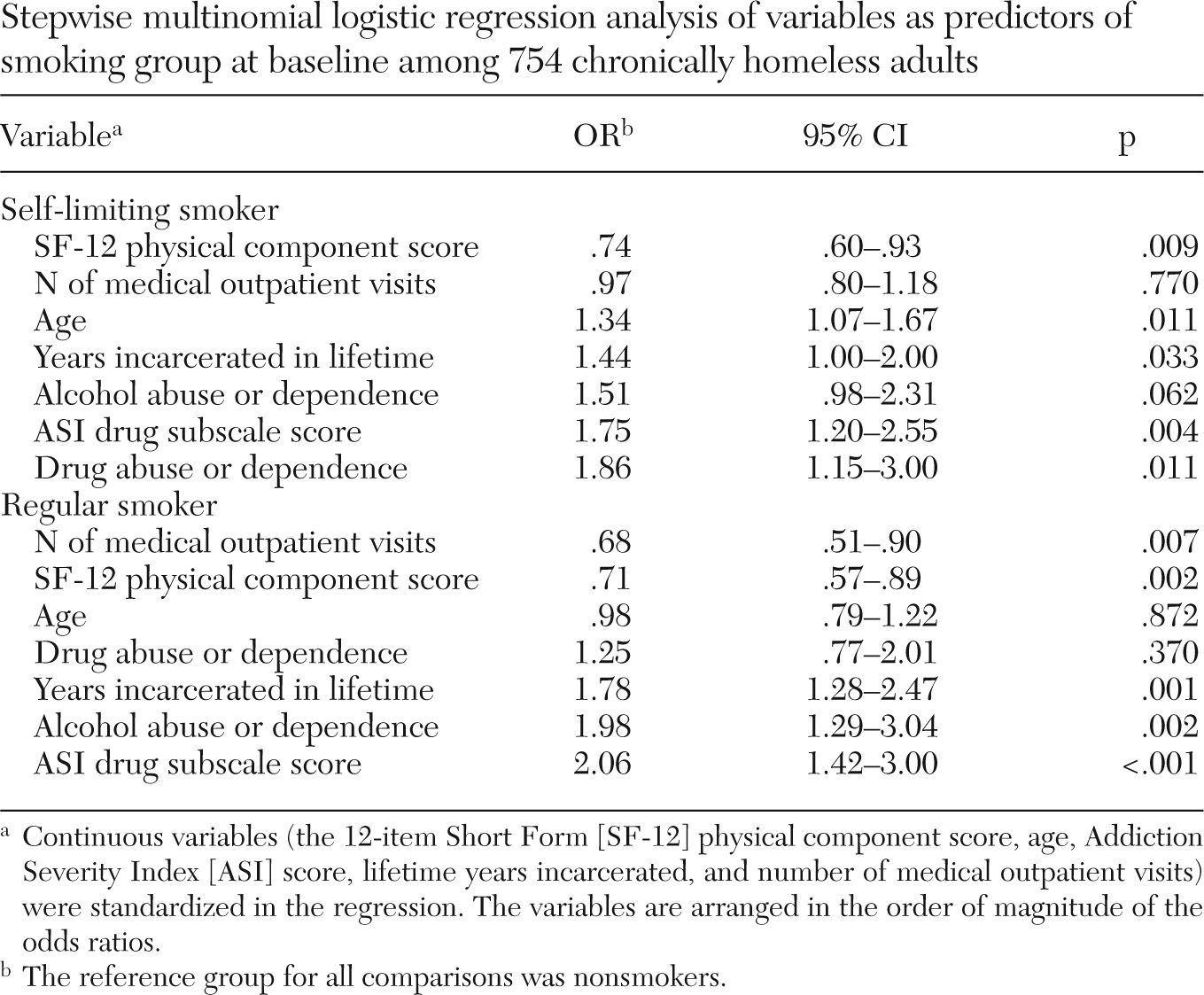
A stepwise multinomial regression was conducted to examine the independent association between significant baseline variables and smoking group at baseline. Similar significant risk factors for smoking were found for self-limiting and regular smokers (
Table 3). A diagnosis of an alcohol or drug use disorder, a lower SF-12 physical component score, older age, more years incarcerated, and a higher score on the ASI drug subscale significantly increased the likelihood of being either a self-limiting smoker or a regular smoker. Scores on the ASI drug subscale had the strongest association with being a smoker (odds ratio [OR]=1.75 for self-limiting smokers, OR=2.06 for regular smokers).
Over the one-year study period, no significant change was found in the proportion of participants in each smoking group. Across time points, nonsmokers accounted for 20%–22% of participants, self-limiting smokers for 37%–43%, and regular smokers for 37%–41%. The results were similar when data were analyzed for only participants who provided data at both baseline and 12-month follow-up (N=582).
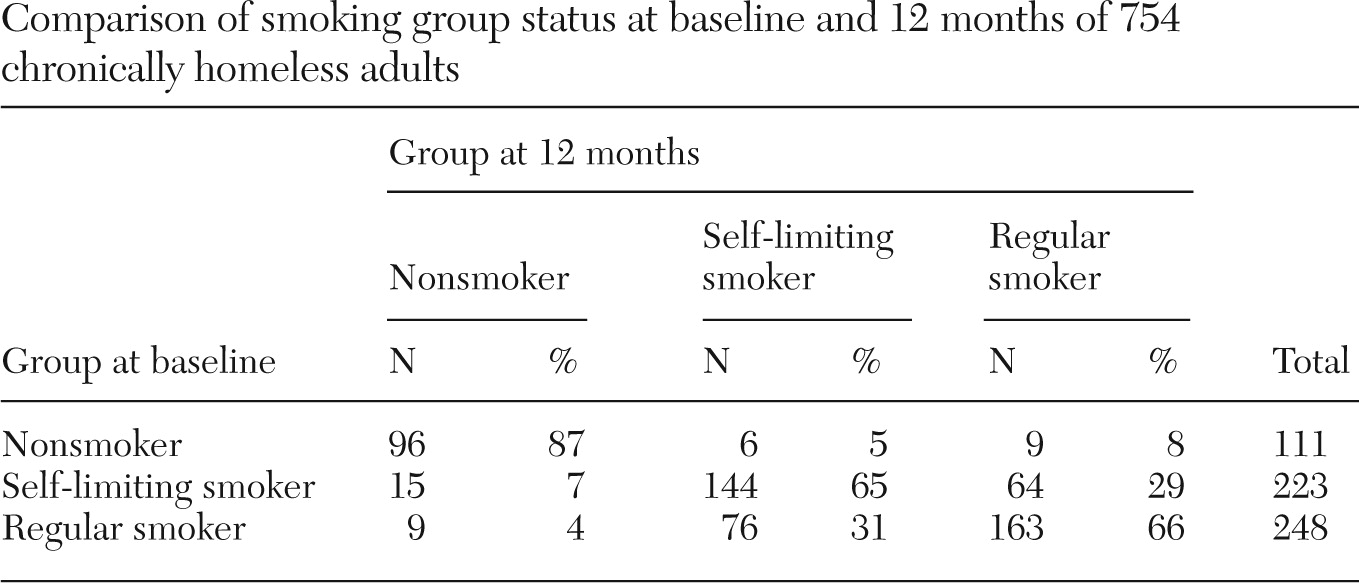
Table 4 shows the proportion of participants in each smoking group at baseline in terms of their smoking group status at 12-month follow-up. Most nonsmokers at baseline remained nonsmokers at 12 months, and most smokers at baseline remained smokers at 12 months, although the proportions of self-limiting smokers who became regular smokers and of regular smokers who became self-limiting smokers were about 30%.
Given the strong associations at baseline between smoking group and scores on the ASI alcohol and drug subscales, we examined these associations over time. When the analysis controlled for baseline values of these variables, changes in ASI alcohol scores and ASI drug scores were both positively associated with changes in smoking status over a one-year period (r=.12, p=.005, and r=.12, p=.003, respectively). On the basis of observations from all time points over one year, the ASI alcohol and drug scores were also both positively associated with smoking status (r=.17, p<.001, and r=.18, p<.001). This was confirmed by a linear mixed regression analysis, which found that when the analysis controlled for baseline ASI alcohol scores, smoking group was significantly associated with ASI alcohol scores over time (F=17.26, df=2 and 2,565, p<.001). Nonsmokers had an ASI alcohol least-square mean score of .09±.01; for self-limiting smokers this score was .10±.00, and for regular smokers it was .13±.00. A similar effect was seen for smoking group on the ASI drug scores over time (F=16.66, df=2 and 2,564, p<.001) when the analysis controlled for baseline ASI drug scores. Nonsmokers had an ASI least-square mean score of .04±.00; for self-limiting smokers this score was .05±.00, and for regular smokers it was .06±.00.
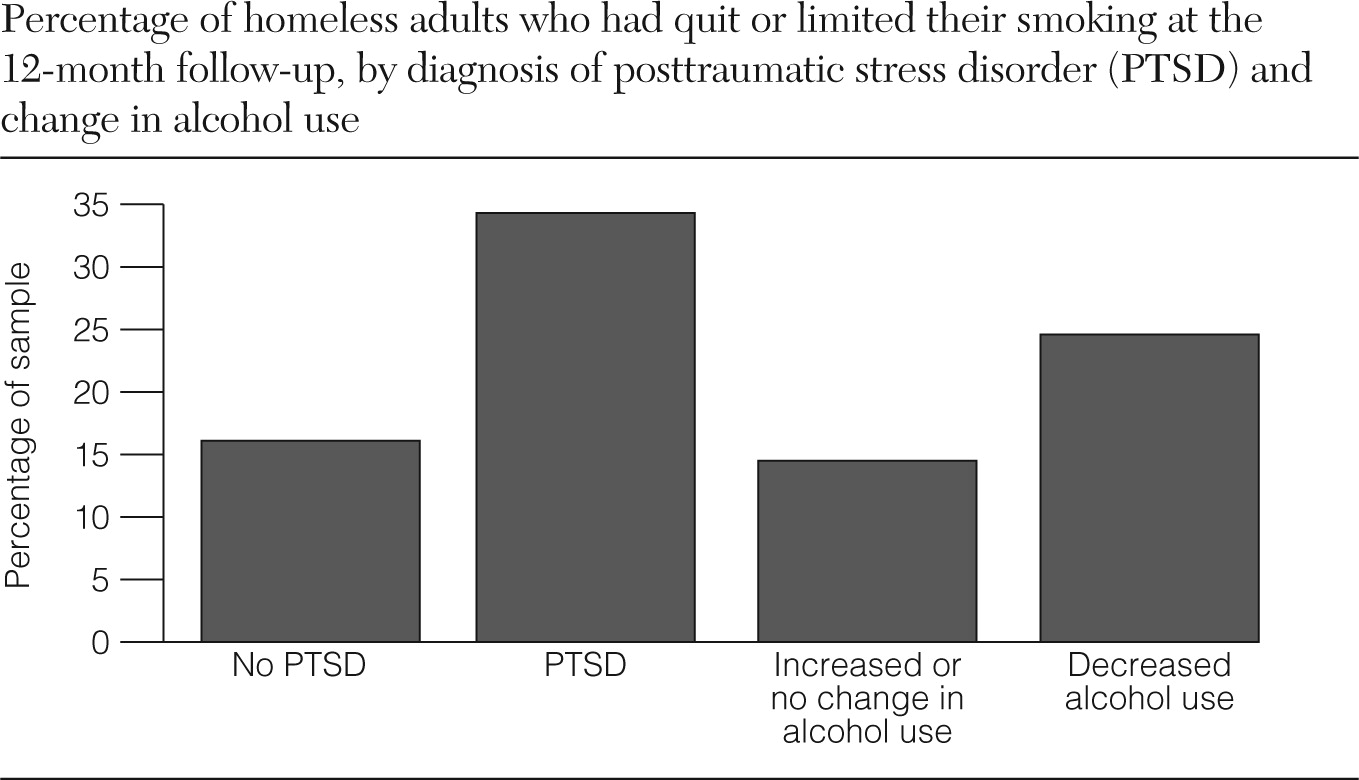
To examine predictors of quitting or limiting smoking over time, a stepwise binary logistic regression was conducted using all baseline variables and change scores on the ASI alcohol and drug subscales to predict over one year either quitting or becoming a self-limiting smoker versus making no change or smoking more. In the final model, the only significant variables were a diagnosis of posttraumatic stress disorder (b=1.21, SE=.45, p=.007, OR=3.36) and change score on the ASI alcohol subscale (b=.26, SE=.11, p=.020, OR=1.30) (
Figure 1).
Discussion
This study found that among a large sample of chronically homeless adults, 80% reported cigarette smoking in the past three months. This point prevalence rate is similar to but slightly higher than previous estimates among homeless adults (
13,
14) and among people with severe mental illness (
3–
5). The findings of this study suggest that smoking may be even more prevalent in the chronically homeless population, although a more representative sampling may be needed.
Among homeless smokers, about half reported that they tried to limit their smoking, and accordingly, more than half reported that they had discussed smoking with a health care provider in the year before entering supported housing, which is similar to estimates in previous studies (
13,
15). This finding is encouraging because it suggests that most homeless clients have at least been asked by their providers about smoking, which casts some doubt on the belief that health care providers delay addressing smoking in order to address more salient primary mental health and psychosocial problems (
7). However, this study did not document whether homeless smokers were referred to or received any smoking cessation treatment. There has been virtually no research on smoking interventions targeting homeless people, although preliminary data from pilot studies have shown that cognitive-behavioral therapy, motivational interviewing, and pharmacotherapy are feasible and may be effective (
25–
27). Development and empirical evaluation of specific interventions for this population are needed.
One question generated by the findings is how homeless individuals maintained their nicotine use with such limited incomes. The cost of cigarettes can be prohibitively expensive, especially for those who are regular smokers. It is not clear how or whether the study participants paid for their cigarettes. A prior study found that homeless adults often shared cigarettes with others, smoked remade cigarettes, or smoked discarded cigarette butts and filters (
28). Further investigation is needed on how much money homeless people spend on cigarettes and whether increases in income may lead to increased spending on tobacco, as one study found among beneficiaries of Social Security Disability Insurance (
29). In those cases, money management interventions, which have been found to be somewhat effective for alcohol and drug abuse (
30), may be helpful in promoting nicotine cessation, although this needs to be empirically studied. When correlates of smoking were examined, alcohol use and especially drug use showed some of the strongest independent associations. This is consistent with findings from the Health Care for the Homeless User Survey (
13) and is not surprising given the high prevalence rate of smoking in the general population among persons who abuse alcohol and drugs (
31,
32). Being older, having more lifetime years of incarceration, and poorer physical health also increased the likelihood of being a smoker, and similar correlates were found for those who smoked but tried to limit their cigarette use and those who smoked without monitoring their use. Gender, education, and socioeconomic status were not associated with smoking, contrary to findings for adults in the general population (
1). This may reflect the fact that most chronically homeless adults are male with low levels of education and from low socioeconomic backgrounds. Being in a supported housing program had no effect on smoking behavior over time, which is not surprising because the programs did not focus on providing smoking cessation treatments. However, supported housing programs should consider integrating tobacco cessation services with mental health treatment because this approach has been found to be effective (
8–
10). Change in smoking behavior was found to be associated with change in alcohol and drug use over time, suggesting that tobacco cessation treatment should be provided concurrently with substance abuse treatment, as other researchers have argued (
33,
34). A meta-analysis has shown that smoking cessation interventions provided concurrently with addictions treatment can enhance sobriety (
35). There has been limited research on what types of smoking interventions are most effective for the homeless population, but chronically homeless adults are likely to be more receptive to approaches that take into account their stage of change (
36) because they may be more focused on a variety of other problems.
Multivariate analyses showed not only that reductions in alcohol use predicted quitting or limiting smoking over time but also that participants who had PTSD were more likely to quit or limit their smoking. It is not clear why PTSD would be associated with reduced smoking; however, this finding may be reframed as reflecting the fact that people with severe mental illnesses (schizophrenia, bipolar disorder, or major depression) were less likely to quit or limit their smoking than those with PTSD. Some studies have shown that individuals with severe mental illness have a particularly hard time quitting smoking (
37,
38) and may need additional support and assistance.
This study had several limitations worth noting. Most measures, including those of smoking behaviors, were based on participant self-report. Smoking behaviors were assessed simply, and no data were collected on intent to quit smoking or attempts to quit. The study design was observational, and significant findings were largely associational; therefore, directionality and causality cannot be inferred. A large number of analyses were conducted, which increases the possibility of type I error, although it is notable that the multivariate analyses included only significant variables identified beforehand. Further replication and intervention studies are needed to understand how to best reduce mortality from smoking-related diseases among homeless people.
Conclusions
This study found that alcohol and drug use, which are major risk factors for homelessness, were associated with smoking among chronically homeless adults, suggesting that smoking cessation treatment should be integrated with substance abuse treatment. More than three-quarters of chronically homeless adults in the study reported current smoking, and about half of homeless smokers tried to limit their cigarette use and had spoken to a health care professional in the past year about smoking. However, there are virtually no smoking cessation interventions specific to homeless people. This study demonstrates the need for more attention to smoking among chronically homeless adults because, even though quitting smoking must compete with a range of other goals for homeless adults, smoking is the most preventable cause of death.
Acknowledgments and disclosures
The CICH Funder's Group, representing the U.S. Department of Housing and Urban Development, the U.S. Department of Health and Human Services, and the Department of Veterans Affairs, provided essential support and guidance to this evaluation. This material is also based on work supported by the Office of Research and Development, Veterans Health Administration. The views presented here are those of the authors and do not represent the position of any federal agency or of the United States government.
The authors report no competing interests.