In recent years clinical practice guidelines have informed the treatment of posttraumatic stress disorder (PTSD) (
1). PTSD clinical practice guidelines have been published by the U.S. Department of Veterans Affairs and Department of Defense (VA/DoD) (
2), the American Psychiatric Association (APA) (
3), the United Kingdom National Institute for Health and Clinical Excellence (NICE) (
4), the Australian National Health and Medical Research Council (NHMRC) (
5) and the International Society for Traumatic Stress Studies (ISTSS) (
6).
In a recent review Forbes and colleagues (
1) highlighted a high level of consensus across guidelines. All guidelines recommend the use of selective serotonin reuptake inhibitors (SSRIs) and serotonin-norepinephrine reuptake inhibitors (SNRIs) in the pharmacological treatment of PTSD. Notable differences, however, are that VA/DoD, APA, and ISTSS guidelines recommend SSRIs and SNRIs and trauma-focused psychological therapies as first-line interventions (
2,
3,
6), whereas the NICE and NHMRC guidelines recommend them as second-line treatment when trauma-focused therapies are not available or acceptable to the patient (
4,
5).
Even so, the effectiveness of SSRIs for veterans with combat-related PTSD may be limited (
7); for example, veterans prescribed sertraline for 12 weeks had no differences, compared with placebo, in changes on the Clinician-Administered PTSD Scale (CAPS-2). This may partially explain the common prescribing of medications such as benzodiazepines and second-generation antipsychotics in veteran populations (
8).
VA/DoD, APA, and ISTSS guidelines (
2,
3,
6) caution providers about prescribing benzodiazepines. Specifically, the VA/DoD guidelines recommend “against the long term use of benzodiazepine to manage core symptoms of PTSD,” and the ISTSS guidelines state that “they are contraindicated for PTSD treatment.” Although acknowledging that benzodiazepines are widely used to treat PTSD-related insomnia, anxiety, and irritability, these guidelines emphasize the lack of evidence supporting benzodiazepines' ability to reduce core PTSD symptoms (
2) as well as the need for caution when prescribed to patients with a history of substance abuse (
6). Second-generation antipsychotics have been recommended as adjunctive therapy for patients with a partial response to first-line SSRIs or SNRIs (
3) and for patients who exhibit extreme hypervigilance, physical aggression, and psychotic symptoms (
6). Mood stabilizers have shown promising results in open-label trials, but lack of data demonstrating subsequent efficacy has precluded their being recommended by any PTSD clinical practice guidelines (
2,
3,
6).
The clinical judgment of the prescribing physician is integral to the use of such medications in PTSD treatment. This study used data from the Longitudinal Veterans Health Survey to examine patient factors that predict which veterans are most likely to receive medications from the following drug classes: benzodiazepines, second-generation antipsychotics, and mood stabilizers. We specifically sought to determine how prescribing these medications was associated with clinical considerations supporting a clear rationale for their use.
Our objectives were to investigate, first, what proportion of PTSD patients who received psychotropic medications were prescribed long-term benzodiazepines (defined here as two or more 30-day supplies of benzodiazepines), second-generation antipsychotics, and mood stabilizers. Second, we wanted to know what proportion of PTSD patients prescribed long-term benzodiazepines, second-generation antipsychotics, or mood stabilizers received them in the absence of a co-occurring diagnosis for which those medications have a clear indication. (We defined such diagnoses as anxiety disorders for benzodiazepine prescriptions, psychotic or bipolar disorders for second-generation antipsychotic prescriptions, and seizure or bipolar disorders for mood stabilizer prescriptions.) Third, among PTSD patients receiving such prescriptions, what proportion also received first-line recommended pharmacotherapy in the form of an SSRI or SNRI? Receipt of such first-line pharmacotherapy would indicate use of benzodiazepines, second-generation antipsychotics, and mood stabilizers as augmentation to a partial response to first-line pharmacotherapy. Fourth, after controlling for relevant co-occurring diagnoses for which these three drug classes have a clear indication, we sought to determine what other characteristics are associated with PTSD patients' receipt of these medications. We anticipated that prescribing of benzodiazepines would be associated with having more severe PTSD symptoms and would be negatively associated with concurrent substance use problems. We anticipated that second-generation antipsychotics or mood stabilizers might more likely be prescribed to veterans with more impaired functioning, as indicated by more severe PTSD symptoms, violent behavior, or recent psychiatric hospitalization.
This study contributes to the existing literature (
7–
9) by its examination of clinical characteristics that predict prescribing of benzodiazepines, second-generation antipsychotics, and mood stabilizers to veterans and whether such prescribing is consistent with a clinical rationale. Finally, we provide previously unreported data on PTSD-related prescribing patterns for veterans from the conflicts in Afghanistan and Iraq (Operation Enduring Freedom and Operation Iraqi Freedom; OEF/OIF).
Methods
Sample, recruitment, and sources of data
Study participants were recruited as part of the Longitudinal Veterans Health Survey, an observational study of treatment outcomes among veterans with PTSD. The study respondents were a nationally derived sample of 482 VA patients who had received a DSM-IV diagnosis of PTSD (309.81) within the previous six months. All participants were between the ages of 18 and 69 and served in the Vietnam era or later periods. OEF/OIF veterans and female veterans were oversampled with further stratification by age. Patients received their PTSD diagnosis during any VA outpatient clinic visit between May 31, 2006, and December 7, 2007, and had received no PTSD diagnosis in the two years preceding that visit. Participants completed the baseline mail survey between August 11, 2006, and April 6, 2008.
Study procedures were overseen by the Stanford University Institutional Review Board. Written informed consent was obtained from all study participants. A total of 1,609 VA patients recently diagnosed as having PTSD were contacted by mail and telephone via the Dillman method (
10). Of 500 patients (31%) who agreed to participate, five were excluded because their surveys indicated pre-Vietnam service, 12 were excluded because their survey was completed more than six months after diagnosis, and one veteran later withdrew. Participants received a $10 VA canteen coupon for each survey completed. The final sample included 134 (28%) male OEF/OIF veterans, 109 (23%) female OEF/OIF veterans, 121 (25%) male veterans from prior periods of service, and 118 (24%) female veterans from prior periods.
To assess response bias, study participants were compared with 490 patients randomly selected from the sampling frame. We found little difference in psychotropic prescribing patterns between the two groups, with the exception of antiadrenergic prescriptions, which were prescribed more frequently in the random sample.
Measures
Data about medication type, amount, and refills were obtained from the DSS (Decision Support System) Pharmacy National Data Extracts database over the 12 months after patients first received their PTSD diagnosis. Prescriptions were searched for psychotropic medications with evidence to support their role in the pharmacotherapy of PTSD (
2–
6), in addition to benzodiazepines generally not recommended in the treatment of PTSD (
6). The National Patient Care Database (NPCD) Outpatient Event File and Inpatient Bedsection File were used to obtain diagnostic information.
Psychotherapy visits were determined from the NPCD. Symptom severity was assessed by averaging z scores for PTSD symptoms on the Impact of Events Scale-Revised (
11) depression symptoms on the Center for Epidemiologic Studies Depression Scale (
12), and the 12-item Short Form Mental Health Aggregate subscale (
13). Desire for care was assessed with a yes-no question: “Have you needed or wanted help for an emotional or mental health problem in the last six months?” (
14). Substance-related problems were assessed with the following two items from the self-report version of the Addiction Severity Index (
15): “In the past 30 days, how many days have you experienced alcohol problems such as craving, withdrawal, disturbing effects from using alcohol, or wanting to stop but not being able to?” And “In the past 30 days, how many days have you experienced drug problems such as craving, withdrawal, disturbing effects from using drugs, or wanting to stop but not being able to?” Any answer more than zero was taken as an indicator of potential substance use problems. Violence was assessed in the baseline survey with four questions about behavior in the past four months (for example, “Have you had a physical fight with someone? Threatened someone with a weapon?”). The resulting dichotomous variable was scored as positive if one or more questions were endorsed. Patient age, gender, index visit, clinic type, history of inpatient stays, and concurrent diagnoses were determined from the NPCD. OEF/OIF status and race and ethnicity were determined from survey data.
Analysis
We calculated prescription frequency in eight medication classes as a proportion of veterans who had at least one prescription for a psychotropic medication. The classes were SSRIs or SNRIs, second-line-recommended antidepressants, trazodone, nonbenzodiazepine sedatives or hypnotics (buspirone, cyproheptadine, eszopiclone, hydroxyzine, zaleplon, and zolpidem), antiadrenergic agents (clonidine, guanfacine, prazosin, and propranolol), mood stabilizers, second-generation antipsychotics, and long-term benzodiazepines. We investigated the proportion of veterans receiving long-term benzodiazepines, second-generation antipsychotics, and mood stabilizers in the absence of a clearly indicated diagnosis. Finally, within this subsample, we calculated what proportion of patients received such prescriptions after receiving an SSRI or SNRI prescription, overlapping with an SSRI or SNRI prescription, before receiving an SSRI or SNRI prescription, or with no SSRI or SNRI prescription in the year after the PTSD diagnosis.
Logistic regression models were then developed to predict three dependent variables: odds of receiving a long-term benzodiazepine prescription, odds of receiving a prescription for a second-generation antipsychotic, and odds of receiving a prescription for a mood stabilizer. Each dependent variable was regressed on the following variables: period of service, age, gender, race or ethnicity, treatment setting for diagnosis (mental health versus primary care), whether the patient had at least one psychotherapy visit in the year after diagnosis, whether the patient had received inpatient mental health care, symptom severity, whether the patient wanted help for mental health problems, presence of comorbid alcohol and drug abuse, and, finally, issues with violent behavior. Age, gender, race or ethnicity, desire for help, and the violence measure were not significant predictors in preliminary univariate analyses and hence were excluded from the multivariate analysis. Statistical analyses were performed with SPSS software, version 18.0 (
16).
Results
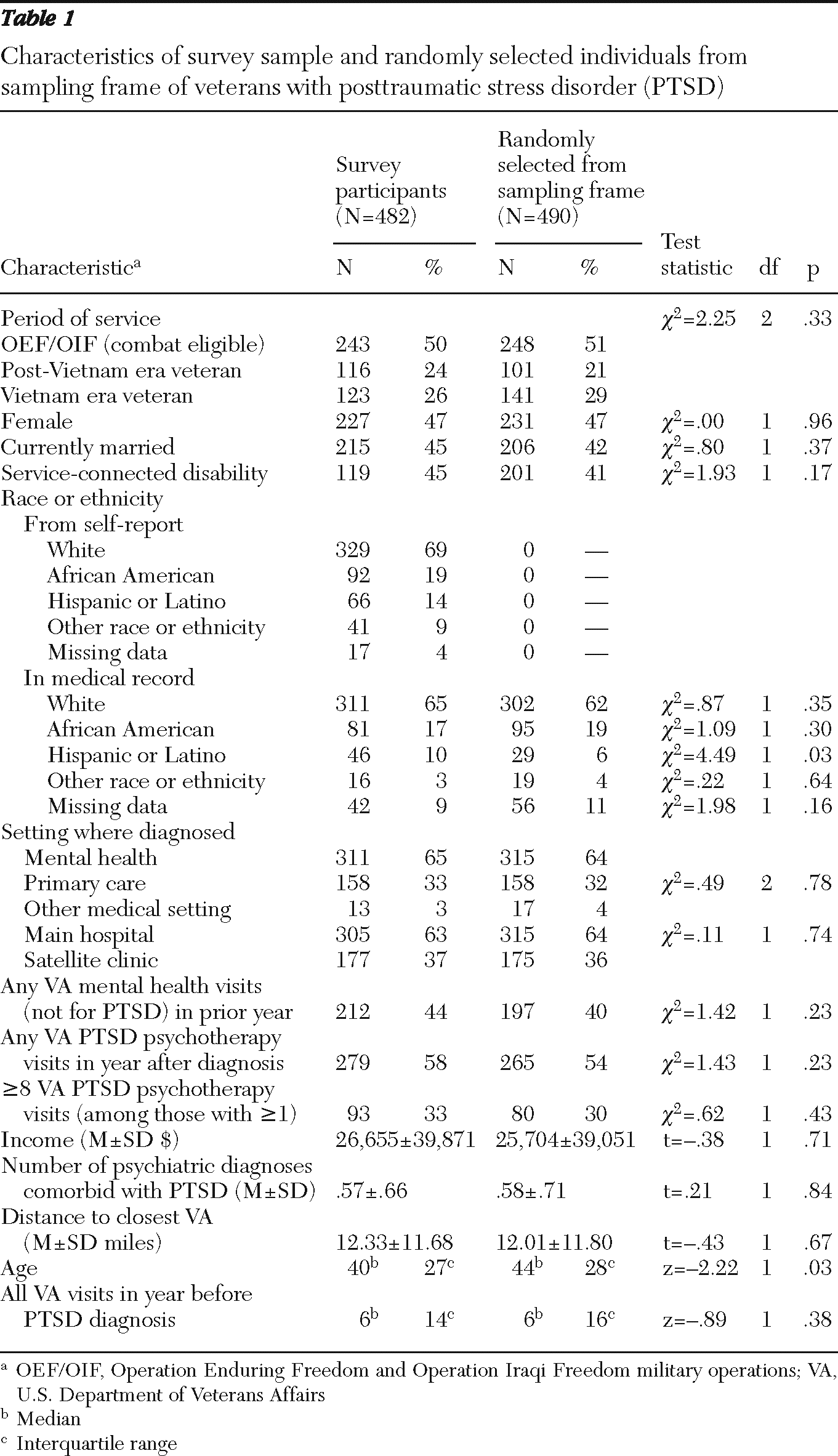
Table 1 presents data on demographic and other characteristics of the sample. As expected from the sampling strata, 47% of the sample were women, and 50% were OEF/OIF era veterans. A total of 81% (N=392) of the 482 sample patients were prescribed at least one of the psychotropic medications.
Benzodiazepines
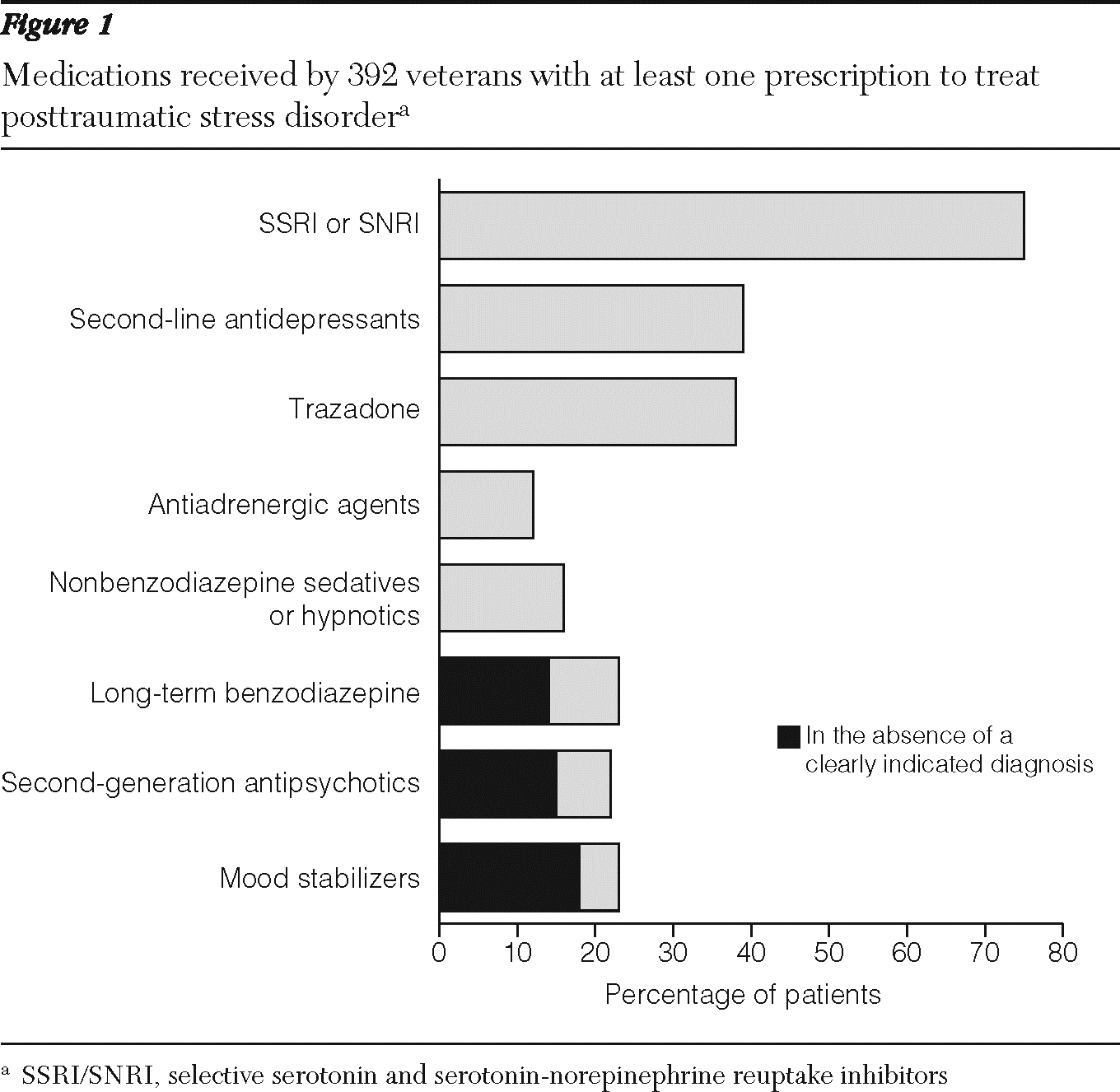
Long-term benzodiazepines were prescribed to 23% (91 of 392) of the veterans who received psychotropic medications (
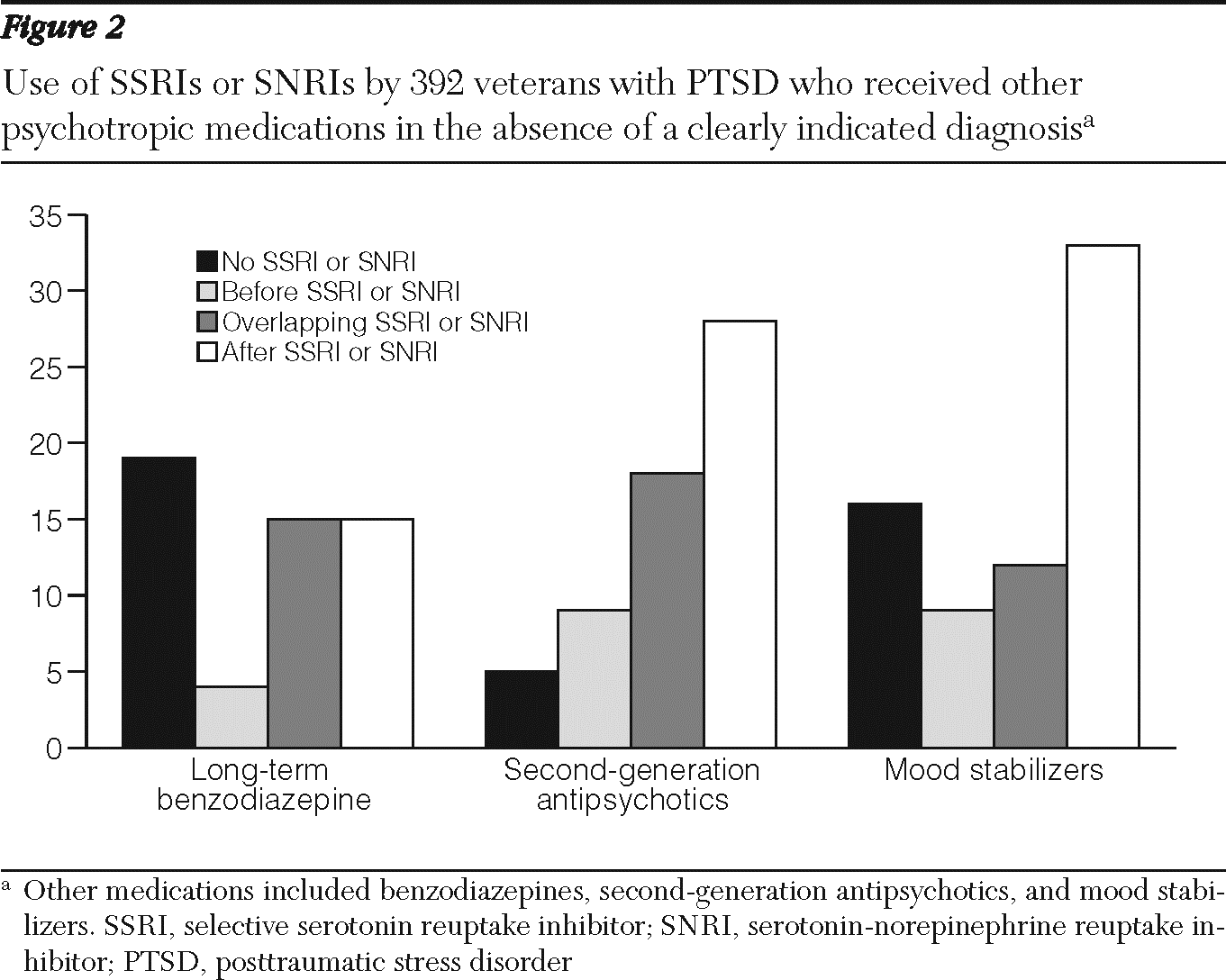
Figure 1). Fifty-three of these patients did not have a co-occurring anxiety disorder. Of these 53 patients, 15 received a long-term benzodiazepine after receiving an SSRI or SNRI, 15 received one along with an SSRI or SNRI, four received a benzodiazepine before receiving an SSRI or SNRI prescription, and 19 received a benzodiazepine without an SSRI or SNRI prescription (
Figure 2).
Having an anxiety disorder was the only significant predictor of receiving a long-term prescription for benzodiazepines in the logistic regression analysis (OR=3.20, p<.01). Overall symptom severity did not predict benzodiazepine use. However, in a post hoc analysis, we examined whether specific symptoms on the Impact of Events Scale and Center for Epidemiologic Studies Depression Scale were associated with long-term benzodiazepine use by patients without co-occurring anxiety disorders. Recipients of long-term benzodiazepines were more likely to indicate problems with restless sleep (OR=1.89, CI=1.20–2.96, p<.01) or with staying asleep (OR=1.41, CI=1.05–1.88, p<.05). Temazepam—typically prescribed as a sleep aid—was the most commonly prescribed benzodiazepine among PTSD patients without a concurrent anxiety diagnosis.
Second-generation antipsychotics
Second-generation antipsychotics were prescribed to 22% (87 of 392) of the veterans who received psychotropic medication (
Figure 1). Sixty of these patients did not have a co-occurring psychotic or bipolar disorder. Of these 60 patients, 28 received a second-generation antipsychotic after receiving an SSRI or SNRI, 18 received it overlapping with an SSRI or SNRI, nine received it before an SSRI or SNRI prescription, and five received it with no SSRI or SNRI prescription (
Figure 2).
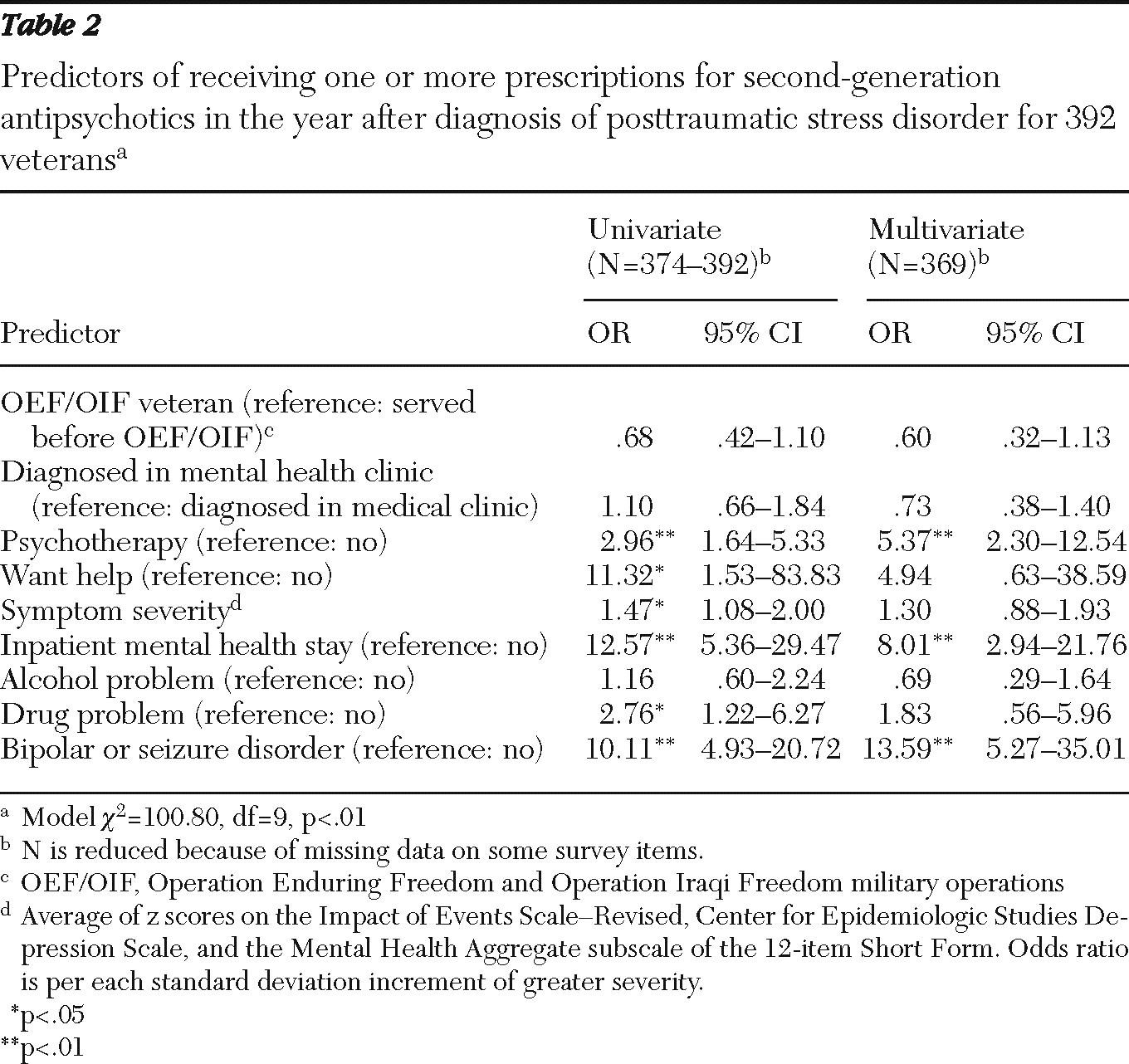
Table 2 shows predictors of receiving a prescription for a second-generation antipsychotic. In addition to having a concurrent psychotic disorder, predictors of receiving a prescription for a second-generation antipsychotic included having a mental health inpatient stay (odds ratio [OR]=8.01, p<.001) and having at least one psychotherapy visit (OR=5.37, p<.001).
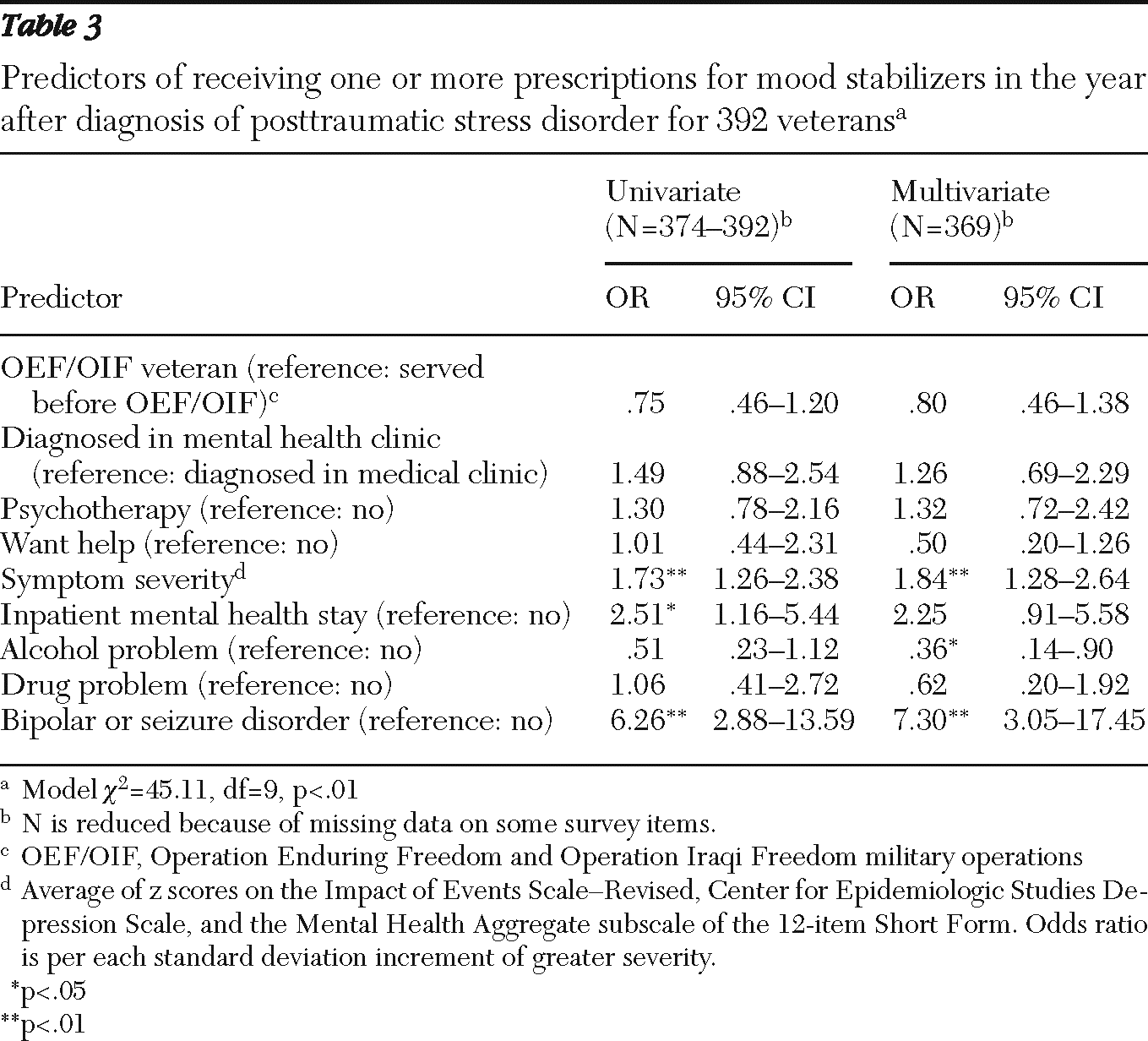
Mood stabilizers
Eighty-eight (22%) of the 392 veterans who received psychotropic medication were prescribed a mood stabilizer (
Figure 1). Seventy did not have a co-occurring seizure or bipolar disorder. Of these 70 patients, 33 received the mood stabilizer after receiving an SSRI or SNRI, 12 received it along with an SSRI or SNRI, nine received it before receiving an SSRI or SNRI prescription, and 16 received it alone (
Figure 2).
Table 3 shows predictors of receiving a prescription for mood stabilizers. In addition to having a concurrent seizure disorder or bipolar disorder, more severe symptoms (OR=1.84, p<.001) predicted receiving a mood stabilizer. Self-reporting problems with alcohol use significantly reduced the likelihood of being prescribed a mood stabilizer (OR=.36, p<.03).
Discussion
Previous studies have noted that benzodiazepine and second-generation antipsychotic prescribing among VA patients with diagnosed PTSD was substantial (
8,
9). Benzodiazepine prescribing in the absence of a co-occurring anxiety disorder was seen in 14% of our sample. We highlight the importance of adequate screening for substance abuse given that we were not able to support our hypothesis that PTSD patients who self-reported substance use problems would be less likely to receive benzodiazepines than were those without such problems. In addition, some previous research has shown that veterans with PTSD and a concurrent substance use disorder had an increased risk of being prescribed long-term benzodiazepines (
17).
Our post hoc analysis suggests that benzodiazepines may be being prescribed for sleep disturbances. Although this may be justified, clinicians should consider that benzodiazepines' effects are often short lived, can potentially interfere with the effectiveness of evidence-based psychotherapies for PTSD, and may be accompanied by significant adverse effects (confusion or sedation) and a risk of dependency (
2). Also, although benzodiazepines are among the most well-studied medications to treat insomnia, it is unclear whether prescribers were also utilizing more conservative, behavioral therapies (
18).
Prescription of second-generation antipsychotics in the absence of a clearly indicated diagnosis was observed in 15% of this sample. Second-generation antipsychotic prescriptions were more common among veterans receiving psychotherapy or among those who had been hospitalized, suggesting that clinicians use such medications for patients who are not responding to other forms of treatment. Previous studies have noted patterns of significant second-generation antipsychotic prescribing in the VA and have warned about the potentially serious side effects of this class of medications (
1). Consistent with these concerns and with recommendations of clinical practice guidelines (
2,
3,
6), three-quarters (77%) of second-generation antipsychotic prescriptions for PTSD patients without bipolar or psychotic disorders either augmented (30%) or followed (47%) a prescription of a first-line SSRI or SNRI.
Concerns about the role of second-generation antipsychotic prescriptions in the treatment of PTSD have been further emphasized by recent research findings that, among patients with military-related PTSD with SSRI-resistant symptoms, six-month treatment with the second-generation antipsychotic risperidone did not reduce PTSD symptoms compared with placebo (
19). These findings raise the issue of whether the risk-to-benefit ratio of this class of medications is favorable enough to justify use for individuals with PTSD. Our study did not have data on whether prescribers had instituted appropriate monitoring for metabolic side effects, an additional key requirement of clinical practice guidelines. Of note, in our study quetiapine was the most commonly prescribed second-generation antipsychotic. This, again, hints toward sleep disturbance as a possible reason for prescribing because quetiapine is often used to treat nocturnal PTSD symptoms, secondary to the apparent ineffectiveness of SSRIs or SNRIs (
20).
Mood stabilizers were prescribed to 18% of our sample in the absence of a clearly indicated diagnosis. This finding is of particular interest given that treatment guidelines have typically reported insufficient evidence to recommend their use in PTSD and may reflect symptom-guided medication selection by prescribers (
8). Patient factors that predicted mood stabilizer prescribing were higher levels of self-reported symptom severity and lower levels of alcohol misuse. The former observation may be explained by physicians' caution regarding prescribing second-generation antipsychotics, which in recent years have come to be associated with significant metabolic side effects. The later observation may reflect clinicians' sensitivity to the hepatoxicity associated some mood stabilizer medications, which would likely be exacerbated by concurrent alcohol misuse.
There are a number of limitations to our study: First, we could not completely determine the diagnoses or symptoms for which the clinician was prescribing the medication. Second, we did not have access to information on actual medication adherence. Third, the 31% response rate, although consistent with other recent survey studies of veterans and military personnel (
21,
22), was low and raises some questions of generalizabilty. We were encouraged in finding few differences between the survey sample and a comparison sample randomly drawn from the population. Finally, a limitation of the database meant we were unable to assess receipt of guideline-concordant psychotherapy, which is another vital aspect of evidence-based treatment for PTSD.
Conclusions
Ultimately, clinical practice guidelines are successful if they are accepted by practitioners and viewed as useful (
1). Prescribing patterns in our sample appeared consistent with clinical practice guidelines in the following ways: first-line use of an SSRI or SNRI was the most common prescribing practice in this sample. In addition, benzodiazepine prescribing appeared to be primarily targeted to PTSD-related sleep disturbance. Second-generation antipsychotics were typically used as adjunctive treatment and often targeted to individuals requiring hospitalization. Although this pattern of prescribing is in alignment with previous guideline recommendations, recent research findings may call for even more stringent use of second-generation antipsychotics in the future. We also found concerning deviations from clinical practice guidelines: mood stabilizers were prescribed to nearly one in four patients in our sample and usually in the absence of a clearly indicated diagnosis. Furthermore, many mood stabilizers and benzodiazepine prescriptions were written in the absence of first-line SSRI or SNRI prescriptions.
Our study findings emphasize the importance of continuing education regarding careful screening for substance use disorders before prescribing benzodiazepines for veterans with PTSD. Furthermore, additional training regarding behavioral therapies for PTSD-related insomnia may translate to less reliance on benzodiazepine prescriptions. If second-generation antipsychotics continue to be prescribed as adjunctive treatment for PTSD, ensuring appropriate monitoring of related metabolic side effects will be important. Future research should address, in controlled studies, the symptoms at which mood stabilizers are being targeted and their efficacy in treating PTSD. In addition, efficacious and safe treatments that provide relief from nocturnal PTSD symptoms would be worthy of further investigation.
Acknowledgments and disclosures
This work was supported by the VA Office of Academic Affiliations Advanced Fellowship Program in Mental Illness Research and Treatment; VA Sierra-Pacific Mental Illness Research, Education and Clinical Center; the VA National Center for Posttraumatic Stress Disorder; and the VA Palo Alto Health Care System. The views expressed are those of the authors and do not necessarily reflect the official policy or position of the VA or the U.S. government.
The authors report no competing interests.