Other concerns that might make physicians less likely to refer individuals to faith-based programs include whether the programs are as effective as traditional (secular) programs (
1,
2), whether they provide staff with training and qualifications comparable with what is offered in traditional programs (
1,
2), whether faith-based programs treat all faiths equitably (
1,
2), and whether they are appropriate for patients who may not endorse the program's spiritual or religious teachings (
1,
3,
4). If physicians have a low referral rate to faith-based organizations, many patients may not access a treatment that is widely available (Teen Challenge has more than 200 locations, in 49 states;
www.teenchallengeusa.com/locations), potentially as effective as traditional programs, and by some accounts less expensive (
1,
5–
7). Little is known about how physicians navigate these concerns.
This article describes a survey of primary care physicians and psychiatrists that included a vignette of a patient with an alcohol problem. The survey asked about the likely effectiveness of Alcoholics Anonymous (a faith-based program by some accounts) (
8–
10) as well as the likely effectiveness of pharmacologic therapy with a specialist and residential rehabilitation. It also asked about faith-based programs more explicitly: whether the physician knew of any nearby programs, whether he or she would refer patients there, and whether he or she considered spirituality to be critical to the success of 12-step programs. The primary hypotheses were that beliefs would differ between primary care physicians and psychiatrists and between religious and nonreligious physicians.
Methods
Survey
Between September 2009 and June 2010, we mailed a confidential self-administered questionnaire to a stratified random sample consisting of 1,504 U.S. primary care physicians and 512 U.S. psychiatrists age 65 or younger. The sample was generated from the American Medical Association Physician Masterfile, a database intended to include all practicing U.S. physicians. To increase minority religious group representation in the primary care sample, we used validated surname lists to create four strata and oversampled from these strata (
11–
13). We sampled 121 primary care physicians with typical south Asian surnames, 171 primary care physicians with typical Arabic surnames, 86 primary care physicians with typical Jewish surnames, and 1,126 additional primary care physicians (from all those whose surnames were not on one of these ethnic lists). The psychiatrist sample was not sufficiently large to warrant oversampling by ethnic surname. Physicians received up to three separate mailings of the questionnaire. The first mailing included a twenty-dollar bill, and the third offered an additional $30 for participation. Data were double-keyed, cross-compared, and corrected against the original questionnaires. The study was approved by the University of Chicago Institutional Review Board.
We presented the following vignette in the survey materials: “A 47-year-old man is admitted to the hospital with acute alcohol poisoning. After a medical detox, the patient says he has been drinking heavily for years and wants to get help. He has never been hospitalized or gone through rehabilitation before.” The survey included a split-ballot experiment that varied whether the vignette concluded with “He identifies himself as a Christian but says he has not been to church in months” or with “He identifies himself as a Christian but has never been a church-goer.” Each potential respondent was randomly chosen to receive one of these two versions. Identifying the vignette patient as Christian allowed more direct comparison with other literature that focuses on Christian faith-based organizations (
4,
5).
Physicians were asked about the likely effectiveness of three treatments: participation in a local chapter of Alcoholics Anonymous, pharmacological therapy by a physician who specializes in the treatment of addiction, and completion of a residential rehabilitation program. Response options included very effective, somewhat effective, not very effective, and not at all effective (these responses were dichotomized for multivariable analyses as very effective or less effective).
Physicians were then asked, “To the best of your knowledge, are there any explicitly faith-based alcoholism treatment programs (not including AA) in your area to which you could potentially refer this patient?” Response options were yes or no. If respondents answered yes, they were asked, “How likely would you be to refer this patient to one of those programs?” If respondents answered no (they do not know of a faith-based program nearby), the follow-up question was, “Assuming there were, how likely would you be to refer this patient to one of those programs?” The four response options were very, somewhat, not very, and not at all likely, which were dichotomized as very likely or less likely. Finally, we asked, “To what extent do you agree with the following statement: ‘An emphasis on spirituality is critical to the success of 12-step programs.’ ” Responses were dichotomized as agree or disagree.
Primary predictors were physicians' clinical specialty (primary care versus psychiatry) and their religious characteristics. Religious affiliation was categorized by self-report as non-Evangelical Protestant, Evangelical Protestant, Catholic (Roman Catholic and Eastern Orthodox), Muslim, Jewish, Hindu, other religion (including 24 Buddhists), and none or no religious affiliation. The importance of religion was assessed by asking, “How important would you say your religion is in your own life?” Response options were dichotomized as “not very important in my life/fairly important” or “very important/the most important part of my life.”
Statistical analysis
Stratum weights for the primary care physician sample were calculated to account for oversampling from the ethnic surname strata (the design weight). We also created a poststratification adjustment weight to correct for higher response rates among U.S. medical school graduates (versus international medical school graduates) and among physicians whose roles are primarily teaching or “other” (versus office-based, hospital-based, research, or administrative roles or roles identified as unclassified because of missing data). Weights were the inverse probability that a person with the relevant characteristic would be in the final data set. The final weight for each case or respondent was the product of the design weight and the poststratification adjustment weight. This method of weighting—widely used in population-based research (
14)—enabled us to adjust for sample stratification and variable response rates in order to generate estimates for the population of U.S. primary care physicians. Weights were not calculated for the psychiatrist sample because no disproportionate sampling by name strata was performed and because response rates by background variables available from the Masterfile did not differ significantly.
We used the chi square test to see if the experimental variable—whether the patient in the vignette had ever been a church-goer—was associated with any of the primary care physicians' or psychiatrists' responses. We then pooled data from both experimental arms and generated population estimates for psychiatrists' and primary care physicians' responses to each survey item measure. Next, we used multivariable logistic regression to test the primary hypotheses. Model 1 examined the effect of physician specialty, after adjustment for religious affiliation, importance of religion, sex, race, age, and region. Model 2 examined the effect of religion (affiliation or importance) after adjustment for sex, race, age, and region (primary care physicians and psychiatrists were analyzed separately). All analyses were conducted with the survey-design-adjusted commands of Stata SE statistical software, version 11.0.
Results
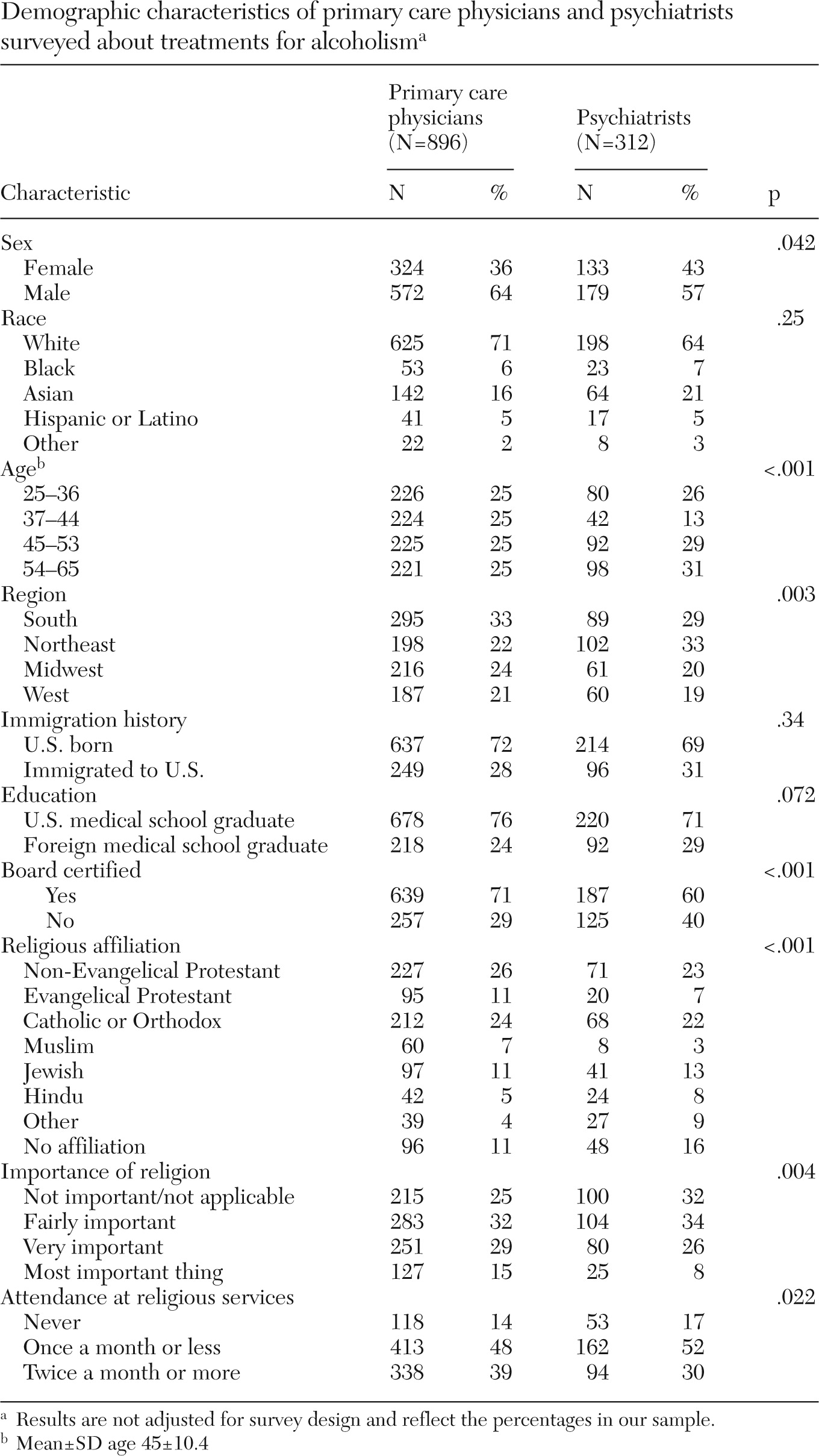
The response rate was 63% (896 of 1,427) for primary care physicians and 64% (312 of 487) for psychiatrists, after excluding 77 primary care physicians and 25 psychiatrists who had invalid addresses or were no longer practicing. The response rate for primary care physicians varied by stratum (p=.006): it was 53% (85 of 162) among those with Arabic surnames, 56% (63 of 112) among those with South Asian surnames, 70% (59 of 84) among those with Jewish surnames, and 64% (689 of 1,069) among the remaining physicians. In the primary care sample, graduates of U.S. medical schools were more likely than international medical school graduates to respond (65% versus 56%, p=.002). Primary care physicians whose practices were primarily teaching or “other” responded at a higher rate (75%, 103 of 138) than physicians whose roles were primarily office based, hospital based, research, administrative, or unclassified (62%, 793 of 1,288; p=.004). Response rates did not differ by age, gender, region, or board certification (
Table 1).
In the chi square analysis, the experimental variable—whether the patient had ever been a church-goer—was not associated with any of the primary care physicians' or psychiatrists' responses to the vignette (p≥.09 for all analyses).
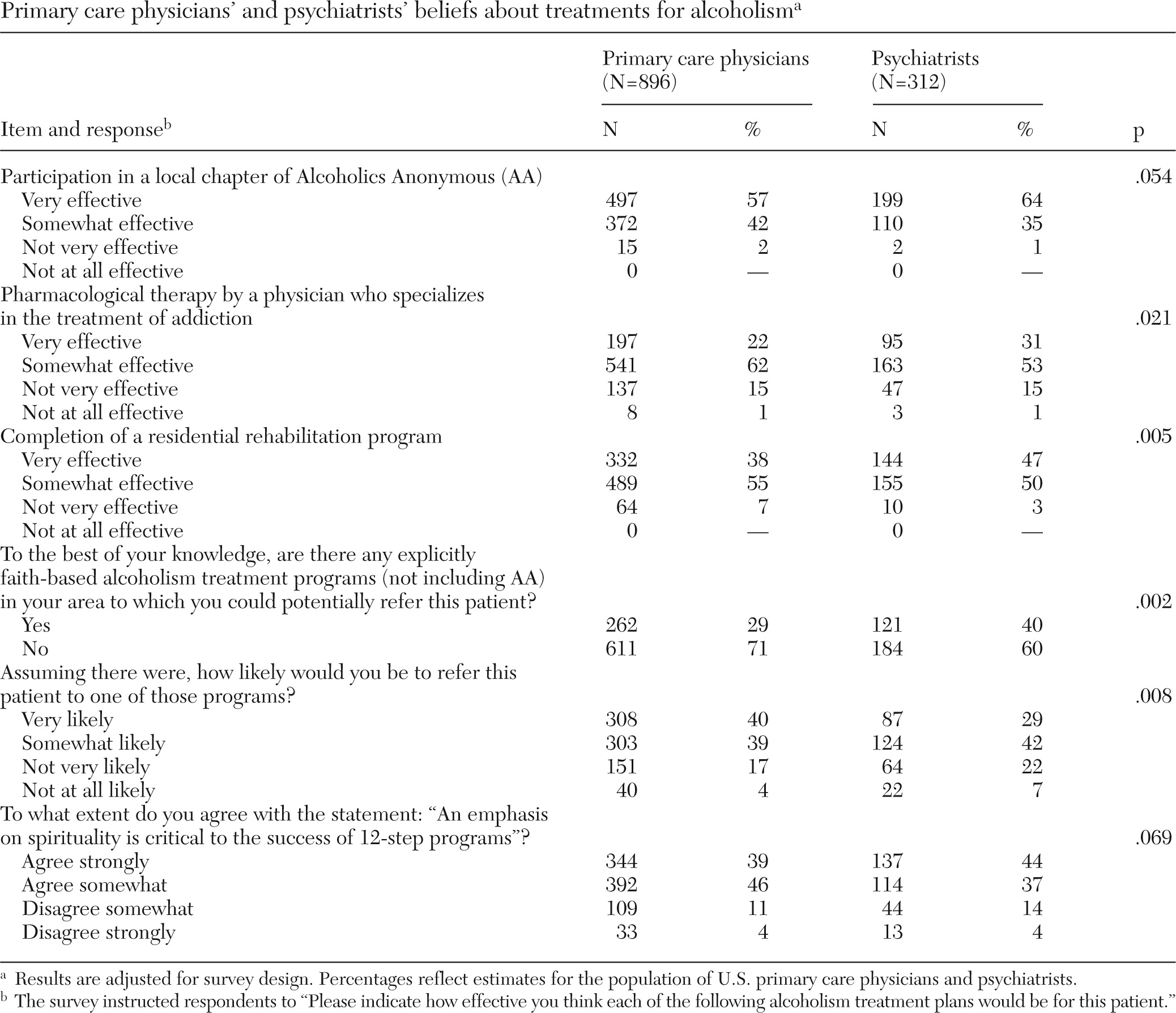
Participation in Alcoholics Anonymous
More psychiatrists (64%) than primary care physicians (57%) thought the vignette patient's participation in Alcoholics Anonymous would be very effective (
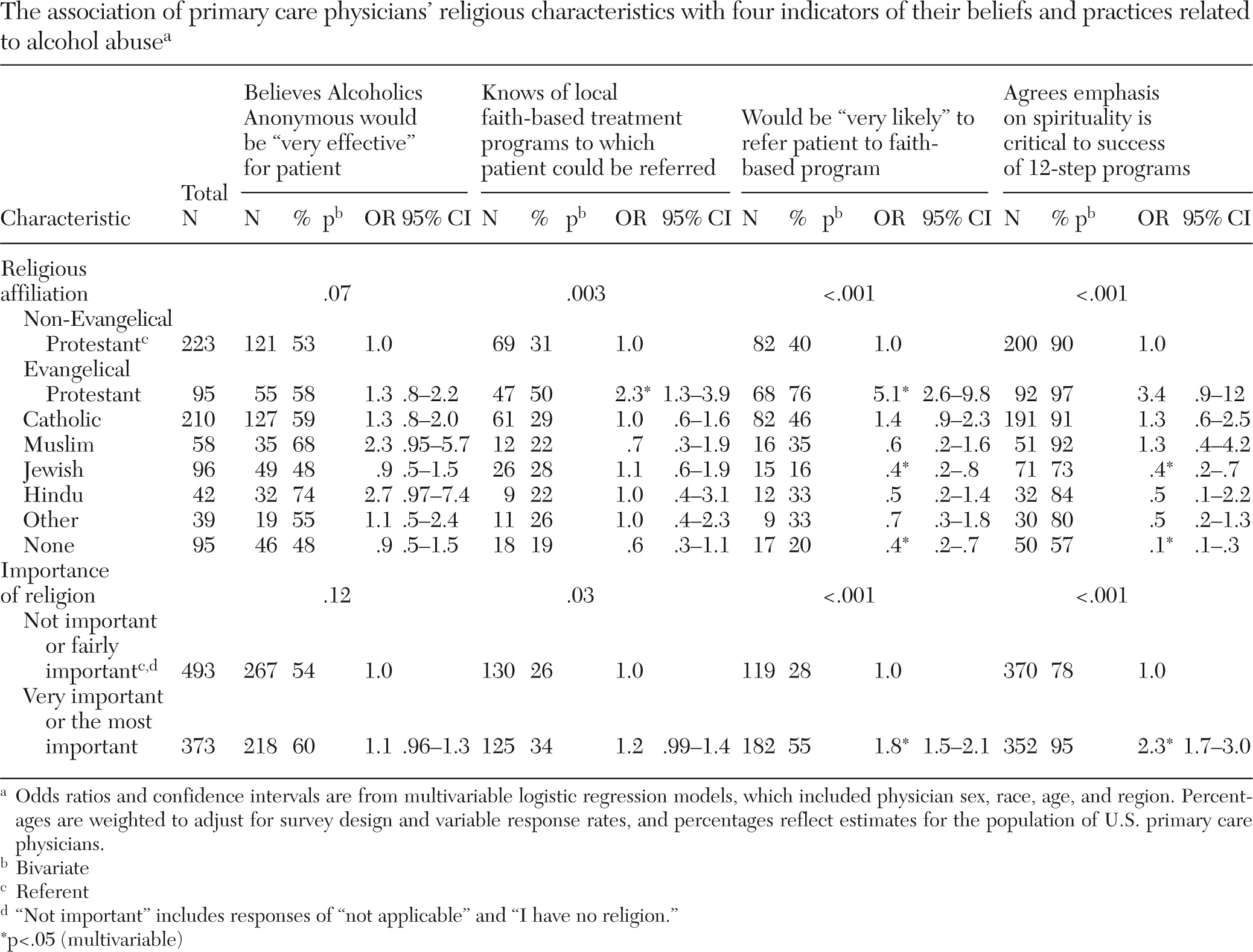
Table 2) (odds ratio [OR]=1.2, 95% confidence interval [CI]=1.1–1.4, model 1). Primary care physicians' beliefs did not vary with religious affiliation or the importance of religion (
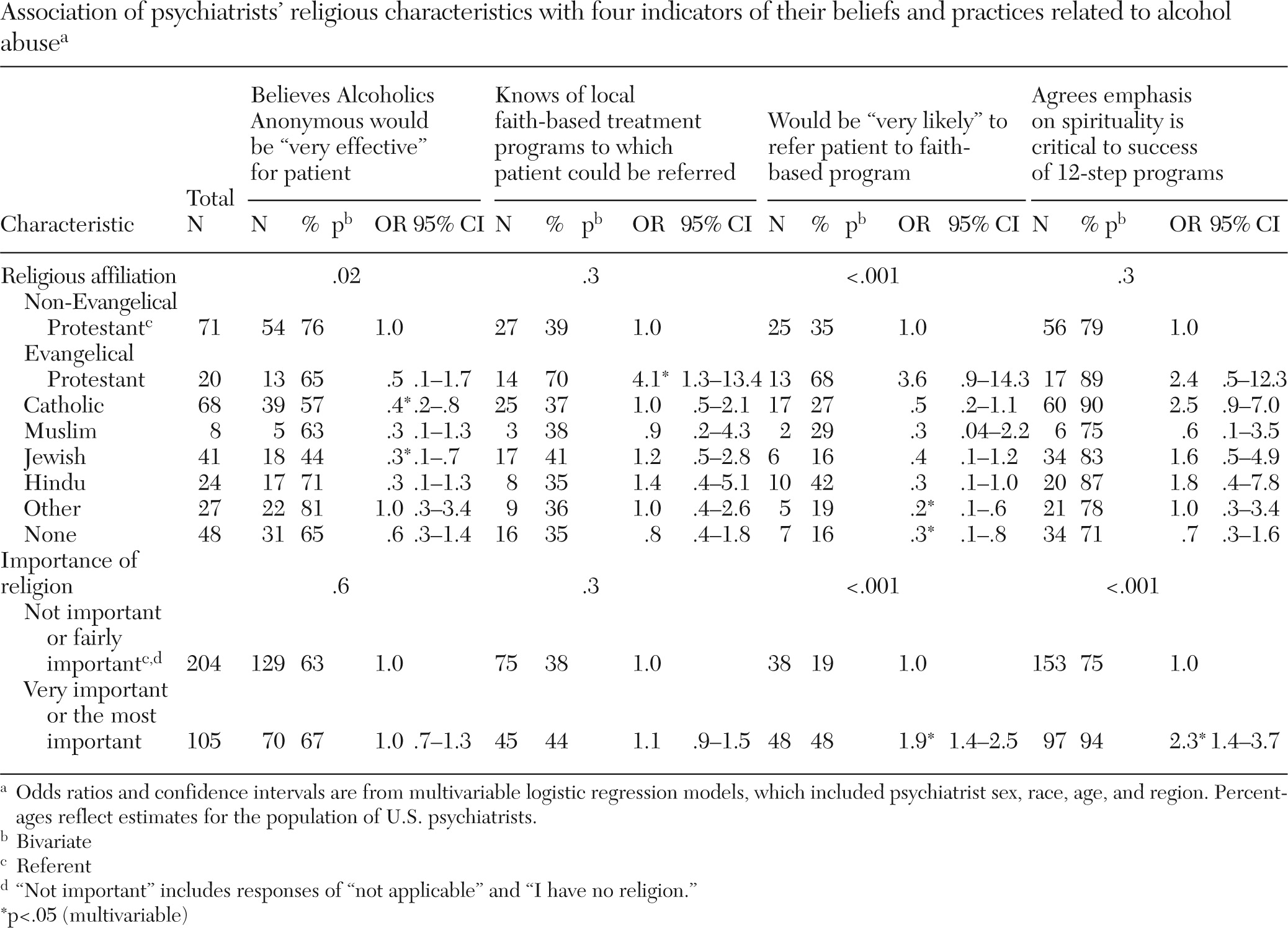
Table 3; model 2). Psychiatrists' beliefs showed some variation by religious affiliation. Whereas 76% of non-Evangelical Protestants (referent) believed that participation in Alcoholics Anonymous would be very effective, this belief was less common among Jewish psychiatrists (44%; OR=.3) and Catholic psychiatrists (57%; OR=.4) (
Table 4; model 2).
Pharmacological therapy
Psychiatrists (31%) were more likely than primary care physicians (22%) to believe that pharmacological therapy by an addiction specialist would be very effective (
Table 2) (OR=1.3, CI=1.1–1.6; model 1). Primary care physicians' beliefs varied with religious affiliation. Although 16% of non-Evangelical Protestants (referent) thought pharmacological therapy with a specialist would be very effective, the belief was more common among Catholics (23%, OR=1.9, CI=1.1–3.3), Muslims (44%, OR=4.6, CI=1.8–11.7), and those practicing some “other” religion (32%, OR=2.7, CI=1.2–6.5) (model 2). Psychiatrists were not analyzed by religious affiliation because of low cell counts. Their beliefs about pharmacological therapy did not vary with the importance of religion (model 2).
Completion of a residential rehabilitation program
More psychiatrists (47%) than primary care physicians (38%) believed that a residential rehabilitation program would be very effective (
Table 2) (OR=1.2, CI=1.1–1.4; model 1). Primary care physicians' and psychiatrists' beliefs about residential rehabilitation did not vary with religious affiliation or the importance of religion.
Awareness of local faith-based programs
More psychiatrists (40%) than primary care physicians (29%) were aware of faith-based treatment programs nearby (
Table 2) (OR=1.4, CI=1.2–1.6; model 1). Among primary care physicians, Evangelical Protestants were significantly more likely than non-Evangelical Protestants to know of a faith-based treatment program in their area (50% and 31%, respectively; OR=2.3;
Table 3, model 2). Among psychiatrists, more Evangelical Protestants than non-Evangelical Protestants knew of a faith-based treatment program in their area (70% versus 39%, respectively; OR=4.1;
Table 4, model 2).
Willingness to refer
Psychiatrists (29% very likely) and primary care physicians (40% very likely) did not significantly differ in their likelihood of referring individuals to faith-based programs (
Table 2) (OR=.9, CI=.8–1.1; model 1). Among primary care physicians, 40% of non-Evangelical Protestants were very likely to refer the vignette patient to a faith-based program (referent). Significantly more Evangelical Protestants were very likely to refer the vignette patient (76%, OR=5.1), whereas smaller proportions of Jewish physicians (16%, OR=.4) and unaffiliated physicians (20%, OR=.4) were very likely to refer (
Table 3, model 2).
Among psychiatrists, 35% of non-Evangelical Protestants were very likely to refer patients to a faith-based program. However, a smaller proportion of psychiatrists with no religious affiliation were very likely to refer patients to such programs (16%, OR=.3;
Table 4, model 2).
The importance of religion also played a role. Compared with physicians who consider religion unimportant or not very important, more physicians who considered religion very important or the most important part of their lives were very likely to refer the patient to a faith-based program. This pattern was observed for primary care physicians (55% versus 28%, OR=1.8;
Table 3) and psychiatrists (48% versus 19%, OR=1.9;
Table 4, model 2).
Of note, physicians who knew of a faith-based program nearby were more likely than physicians who did not know of any nearby program to refer the patient to a faith-based program. This was true for primary care physicians (55% versus 32% very likely, OR=2.1, CI=1.4–3.1) and psychiatrists (41% versus 21% very likely, OR=2.9, CI=1.5–5.4) and was significant after adjustment for religious affiliation, importance of religion, sex, race, age, and region.
Spirituality as critical
Most respondents agreed somewhat or strongly that an emphasis on spirituality is critical to the success of 12-step programs (85% of primary care physicians and 81% of psychiatrists) (
Table 2, model 1). Among primary care physicians, 90% of non-Evangelical Protestants (referent) believed spirituality is critical. However, a smaller proportion of Jews (73%, OR=.4) and of physicians with no religious affiliation (57%, OR=.1) agreed (model 2).
Compared with those who considered religion unimportant or fairly important, physicians who considered it very important or the most important part of their lives were more likely to consider spirituality critical to 12-step program success; this was true for primary care physicians (95% versus 78%, OR=2.3;
Table 3, model 2) and psychiatrists (94% versus 75%, OR=2.3;
Table 4, model 2).
Discussion
In this national survey, psychiatrists appeared more optimistic than primary care physicians about the effectiveness of Alcoholics Anonymous, pharmacological treatment, and residential rehabilitation to treat alcoholism. Some of this difference is likely attributable to psychiatrists' receipt of special training in addiction medicine during residency and through continuing education. Beyond this, though, opinions could be shaped by psychiatrists' and primary care physicians' seeing slightly different patient populations (for example, primary care offices may have more patients who are resistant to psychiatric treatment, often an important component of recovery from addiction). Alternatively, primary care physicians and psychiatrists may have different thresholds for calling a treatment effective.
Physicians' enthusiasm for Alcoholics Anonymous has been noted before (
15) and is in line with evidence showing that more frequent attendance at meetings is associated with less drinking (
16). Perhaps more surprising, however, is that so many physicians believed that the spiritual component is critical to the success of 12-step programs—an important consideration since Laudet (
17) reported that 61% of clients (N=101) believe “the religious aspect of 12-step groups is an obstacle for many.” The centrality of spirituality was a prominent theme among early theorists (
9) and is still commonly encountered (
5,
18), but recent literature has also emphasized the social changes that occur in Alcoholics Anonymous (
19–
22), the value of finding (or becoming) a sponsor (
18,
19), and the acquisition of life skills for staying sober (
5,
9,
18).
To date, empirical research on spirituality and addiction has been mixed. A 1995 survey of residents of Oxford House (a self-governed communal living environment for recovering alcoholics) found that 43% had no spirituality before joining the program and only 11% noted an increase in their spirituality from their experiences with the program (
22). However, Kelly and colleagues (
19), who conducted a lagged mediational analysis, found that Alcoholics Anonymous attendance was associated with increases in spirituality or religiosity (especially among those with low initial spirituality or religiosity) and that the effect of Alcoholics Anonymous attendance on drinking outcomes was partially explained by its effect on increasing spirituality or religiosity.
In our survey, 79% of primary care physicians and 71% of psychiatrists were at least somewhat likely to refer the patient to a faith-based program. These numbers are comparable with the number of patients who are referred to Alcoholics Anonymous (79.4% in a survey of substance abuse program directors in the Department of Veterans Affairs [23]). However, in our study, referrals varied dramatically with the physician's own religiosity and with knowledge of a local faith-based program to which to refer the patient. This finding suggests that physicians who were more familiar with local faith-based programs (perhaps through religious or professional ties) felt more comfortable referring patients there.
In this vignette experiment the patient was nominally religious, but this did not dissuade most physicians from referring him to a faith-based program or from anticipating that Alcoholics Anonymous would be very effective. Moreover, varying the patient's church background did not affect physicians' willingness to refer the patient to a faith-based treatment program or their confidence in Alcoholics Anonymous. Whether to refer nonspiritual patients to spiritually oriented programs has been a controversial topic for some time (
16). The 1995 American Psychiatric Association practice guidelines recommended nonspiritual self-help groups (such as Rational Recovery) for patients not comfortable with the spiritual focus of Alcoholics Anonymous (
24). Likewise, Galanter and colleagues (
3) proposed that patients with low spirituality might find it easier to accept programs not oriented toward the 12-step model. Tonigan and colleagues (
21) observed that patients who were atheists were more likely (65.4%, N=17) than religious patients (28.7%, N=87) or spiritual patients (35.2%, N=242) never to attend Alcoholics Anonymous. However, Tonigan and colleagues concluded that although atheists were less likely to attend Alcoholics Anonymous, those who did increased their abstinence.
The study has limitations. Survey results may differ from clinical experiences, and nonresponders may differ from responders. Surveys can assess tendencies, but treatment plans are multidimensional and are negotiated amidst dialogue that a survey cannot replicate. The views observed in this survey may not be representative of addiction specialists (including addiction psychiatrists or chronic pain specialists). Faith-based programs are highly variable, making assessment of the group as a whole difficult. Religion, spirituality, and faith were not sharply differentiated because they are such closely related terms. Future studies might examine whether beliefs differ when programs are described as religious, spiritual, or faith based. We did not observe an effect of manipulating the patient's religious characteristics. Future surveys might increase the degree of religious separation in order to find where opinions start to diverge. Many physicians were unaware of local faith-based programs, but the survey did not differentiate whether this was because physicians were unaware or because no programs exist in that location. The survey did not directly measure the availability of faith-based programs.
Acknowledgments and disclosures
This study was supported by grants from the Greenwall Foundation and the John Templeton Foundation and by grant 1 K23 AT002749 from the National Center for Complementary and Alternative Medicine. Funding agencies did not participate in study design, data acquisition, analysis, interpretation, writing, or submission of the manuscript.
Dr. Curlin served as an advisor to Boehringer Ingelheim Pharmaceuticals, Inc. The other authors report no competing interests.