Since second-generation antipsychotic medications were introduced in 1992, their use by children and adolescents has continued to increase (
1–
4). Antipsychotic prescriptions for U.S. children and adolescents, hereafter referred to as children, have more than quadrupled, from 8.6 per thousand in 1995 to 39.4 per thousand in 2001 (
2,
5). An estimated 15% of individuals receiving antipsychotics are younger than 18 years old (
4). Studies suggest that approximately 1% of all child outpatient visits (
6) and an estimated 9% of all child mental health visits now include a prescription for antipsychotics(
5). Children enrolled in Medicaid, compared with other populations of children, have higher rates of use of antipsychotic medications (
6) and appear to have increased their use of antipsychotics at a rate comparable to that of non-Medicaid-enrolled children (
7,
8). Studies also suggest that substantial numbers of very young Medicaid-enrolled children receive antipsychotic medications (
9). However, recent studies suggest that the rate of growth of antipsychotic medication use by Medicaid-enrolled children may have flattened off after 2004 with the release of warnings on second-generation antipsychotic medications, required by the U.S. Food and Drug Administration, that alerted users to potential side effects such as weight gain, changes in glucose levels, and diabetes (
7).
Antipsychotics are indicated for the treatment of irritability associated with autistic disorder for children over five years old, schizophrenia for children over 13 years old, and bipolar mania for children over ten years old (
10). Historically, schizophrenia and adjustment disorder have been the diagnoses most commonly associated with antipsychotic use by children, but, in recent years, they have been surpassed by mood disorders such as depression and disruptive behavioral disorders such as attention-deficit hyperactivity disorder (ADHD) and conduct disorder (
2,
3,
11–
14). Effective psychosocial interventions exist for many of the disorders for which children are receiving antipsychotics (
15–
19), such as depression and ADHD. Because of lack of evidence of efficacy of antipsychotics among children with these disorders and concerns about the adverse metabolic effects of these medications on youths (
20,
21), the increased off-label use of antipsychotics for children has raised concerns regarding the overall quality of care being provided to children receiving antipsychotics.
In response to public concerns about the use of antipsychotics by children (
22,
23), efforts are under way to identify and subsequently decrease children's questionable use of antipsychotic medications. An important complement to these efforts is to understand and improve the use of appropriate psychosocial services among children receiving antipsychotics. Concern about children receiving antipsychotics while not receiving therapy has increased since a recent study found that a majority of young, privately insured children on antipsychotics do not receive even a single therapy session (
24). There is a paucity of data, however, regarding the extent to which other populations of children receiving antipsychotics are not receiving concurrent mental health therapy (hereafter called “concurrent therapy”). To better understand the receipt of concurrent therapy by children receiving antipsychotics, we examined utilization of concurrent therapy in a population of Medicaid-enrolled children. We studied the rate at which children starting antipsychotics are also receiving concurrent therapy. We also explored clinical and sociodemographic factors associated with concurrent therapy for children starting antipsychotics.
Methods
Population
From a population of approximately 242,000 Medicaid-enrolled children from six to 17 years of age, we identified 6,110 children aged six to 17 who started use of antipsychotics from November 1, 2006, through October 31, 2009. We used state-provided pharmacy data containing filled claims for all Medicaid antipsychotic prescriptions and examined the utilization of concurrent therapy in a large mid-Atlantic state for all children in counties in which behavioral health care is managed by the largest Medicaid-managed behavioral health organization (MBHO). All behavioral health services for all Medicaid-enrolled children in the geographic regions examined were coordinated and paid for by the MBHO. Minimal block-grant-funded mental health services were available in the regions, so the observed claims represent essentially all reimbursed mental health services for all Medicaid-enrolled children. Children who did not have Medicaid eligibility for more than 80% of observed days were also excluded from the analysis.
Variables
A new antipsychotic episode was defined as the first observed use of an antipsychotic following a clean period of 120 days without use of antipsychotics. The episode continued until there was a period of 120 days without the use of an antipsychotic. National Drug Codes were used to identify type of antipsychotic; accurate information about the prescribing physician was unavailable. Children with two or more therapy service claims (any combination of individual, group, family, or behavioral therapy) in the 30 days prior to starting an antipsychotic or at any point while receiving an antipsychotic were categorized as having received concurrent therapy. For children with more than one episode, we used the first episode.
We obtained sociodemographic variables such as race-ethnicity, age, Medicaid eligibility category, and gender from the state's membership and eligibility files. Race and ethnicity were categorized as white, African American, Latino, or other. Consistent with other analyses of Medicaid-enrolled individuals (
25), our analysis categorized children on the basis of their eligibility criteria, such as family income (those on Temporary Assistance for Needy Families), disability (individuals on Supplemental Security Income for medical or mental health disability), and placement in foster care.
We used
ICD-9 diagnoses on claims to determine if a child had a diagnosis of a disorder for which a second-generation antipsychotic was indicated (schizophrenia, bipolar disorder, autism spectrum disorder, mental retardation). In our assignment of indicated diagnoses, we did not include restrictions by child age. For example, antipsychotics were considered indicated among all children with a diagnosis of bipolar disorder, not just children over age ten. A child was categorized as having an indicated diagnosis if the child had two outpatient clinical claims or one inpatient clinical claim (
26) in the 30 days prior to starting an antipsychotic or at any point while receiving an antipsychotic for any of the above disorders. We also identified the diagnosed disorders of children without a diagnosis for which a second-generation antipsychotic was indicated (depression, ADHD, conduct disorder). Children were categorized as having had prior inpatient mental health treatment if they had a psychiatric hospitalization in the 12 months prior to starting an antipsychotic. Consistent with other analyses of Medicaid data (
27,
28), children were categorized as living in an urban area if their county of residence had a population density greater than 1,000 individuals per square mile.
Analysis
We conducted descriptive analyses regarding the relationship between concurrent therapy and sociodemographic and clinical predictor variables, including race-ethnicity, Medicaid eligibility category, age, gender, community of residence, diagnoses, year of service, and prior psychiatric hospitalization. We conducted multivariate logistic regression analyses to examine the relationship between receiving concurrent therapy and our sociodemographic and clinical predictor variables. We present adjusted odds ratios (AORs) with 95% confidence intervals (CIs). Analyses were conducted with SAS for Windows, version 9.1 (
21), and the study was approved by the University of Pittsburgh Institutional Review Board.
Results
Sample characteristics
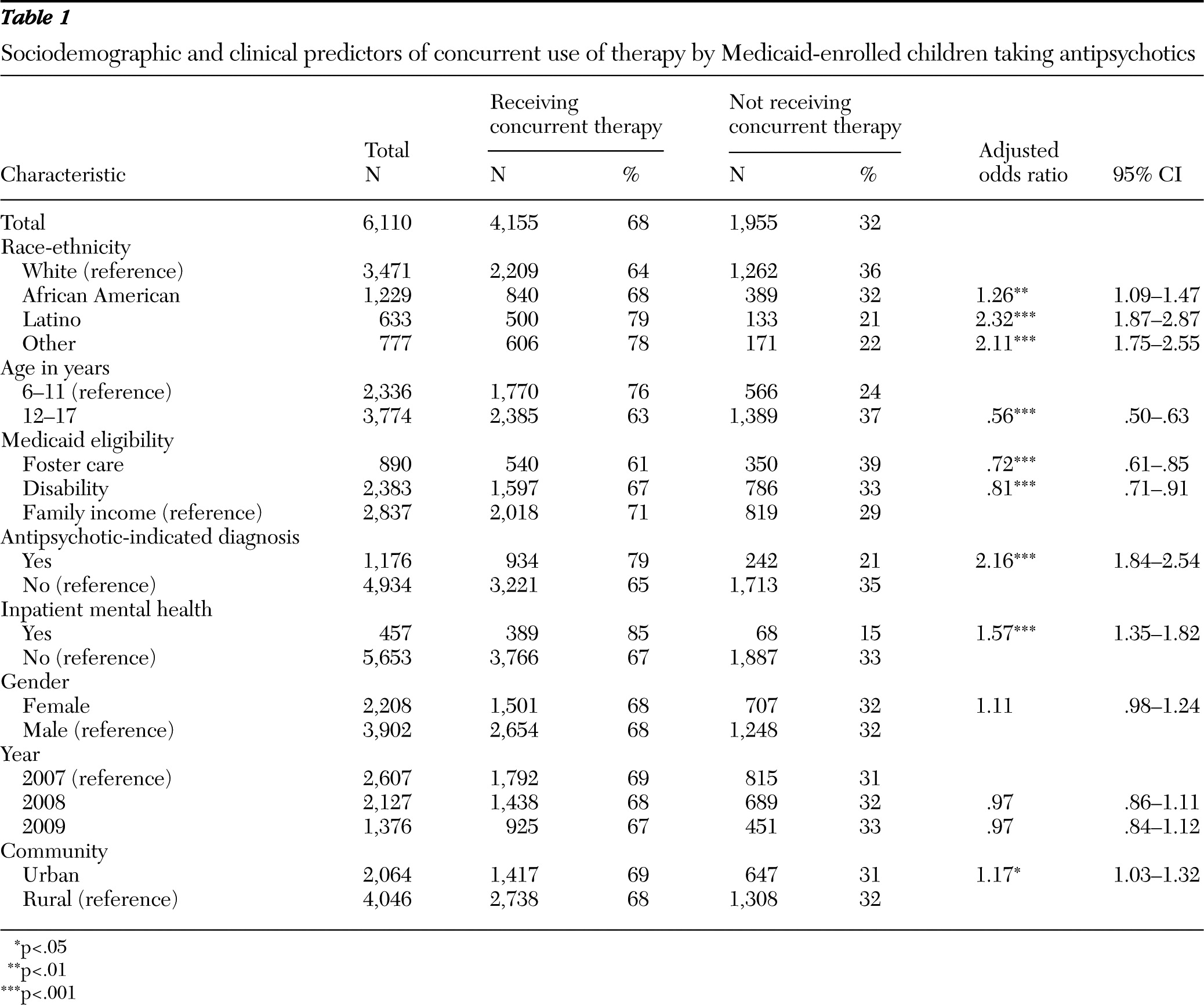
We identified 6,110 Medicaid-enrolled children who started using an antipsychotic from November 1, 2006, through October 31, 2009. The majority of children starting on antipsychotics were boys (64%, N=3,902), white (57%, N=3,471), 12–17 years old (62%, N=3,774), and living in rural communities (66%, N=4,046) (
Table 1). More were Medicaid eligible due to income (46%, N=2,837) than due to disability (39%, N=2,383). Relatively few of the children (19%, N=1,176) were diagnosed as having a disorder for which antipsychotics are indicated: 12% of these children were diagnosed as having autism, 7% as having bipolar disorder, and 1% as having schizophrenia. A majority of children receiving antipsychotics had diagnoses for which atypical antipsychotics were not indicated, such as ADHD (30% of children) and depression (26% of children). Eight percent of children (N=457) had been hospitalized in the year prior to starting an antipsychotic. The most common antipsychotics prescribed included aripiprazole (39%, N=1,767), risperidone (26%, N=1,610), quetiapine (25%, N=1,531), and ziprasidone (6%, N=368; data not shown), and duration of antipsychotic use was longer among children receiving concurrent mental health therapy (median=242 days, mean=320 days, CI=312–328) but still substantial among those not receiving concurrent mental health therapy (median=117 days, mean=184 days, CI=177–192).
Predictors of concurrent therapy
Sixty-eight percent (N=4,155) of children starting antipsychotics were receiving concurrent therapy (
Table 1). Seventy-five percent (N=3,098) of those receiving concurrent therapy had received it prior to starting antipsychotics, and 15% (N=636) started therapy in the 30 days after starting an antipsychotic. The mean±SD number of therapy sessions during the antipsychotic episode was 23.9±42, with a median of 7.0 sessions. After adjustment for other factors, we found that use of concurrent therapy was significantly lower among white children than among children from other racial-ethnic minority groups. Use of concurrent therapy was also significantly lower among 12- to 17- year-old children compared with children ages six to 11 years (63% versus 76%; AOR=.56). Children who were Medicaid eligible due to family income (71%) had higher rates of concurrent therapy compared with children who were Medicaid eligible due to disability (67%) or children in the child welfare system (61%).
We also found that children who were living in urban communities were significantly more likely than those in rural communities to receive concurrent therapy (69% versus 68%; AOR=1.17). Children with a diagnosis for which there is an antipsychotic indication were significantly more likely to receive concurrent therapy compared with those without such a diagnosis (79% versus 65%; AOR=2.16). Children with a psychiatric hospitalization within the year prior to starting an antipsychotic were significantly more likely to receive concurrent therapy than were individuals without such prior hospitalization (85% versus 67%; AOR=1.57). There was no significant difference by gender or by year in receipt of concurrent therapy when controlling for other factors, and the type of antipsychotic was not associated with receipt of concurrent therapy.
Discussion
In our examination of Medicaid-enrolled children starting on antipsychotics, we found that approximately 68% received concurrent therapy. Multiple studies have documented the increased use of antipsychotics by children (
2–
4,
7,
8,
13,
24,
29,
30), including increased prescribing of antipsychotics for children by primary care providers. Given concerns about the increased use and off-label use of these medications by children with more severe emotional and behavioral disorders, our findings suggest that for the majority of Medicaid-enrolled children, these medications are not serving solely as substitutes for nonpharmacologic interventions. There remain, however, a substantial number of children receiving antipsychotics who do not appear to be receiving any formal psychosocial intervention, despite the existence of effective psychosocial interventions for the disorders most commonly being diagnosed among children receiving antipsychotics.
Our results are consistent with others demonstrating that a substantial number of children receiving antipsychotics are receiving them for nonindicated disorders (
2,
3,
6,
8,
9,
24,
31). Efficacious interventions, including psychosocial interventions and medications other than antipsychotics, exist for the majority of emotional and behavioral disorders of children, and the current standard of care recommends that evidence-based medications or psychosocial therapies be implemented prior to the use of nonindicated medications (
32–
38). Given recommendations that psychosocial interventions should generally be considered before pharmacologic interventions (
38,
39), efforts should be made to ensure that clinicians and families are aware of all treatment options and that families have access to adequate trials of effective and appropriate psychosocial interventions and nonantipsychotic medications before proceeding with antipsychotics for their children.
Whether a child receives concurrent therapy may also be influenced by factors other than access to mental health specialty care, such as the preference of family members. A family's choice regarding the use of medications, therapy, or both in the treatment of a child's mental disorder is often a complicated one, influenced by a range of factors. These factors include the perceived benefits of medication and therapy by parents and adolescents (
40) and the willingness of family members and children to participate in therapy and use medications. They also include the prior experiences of family members and other trusted individuals with respect to medication and therapy as well as parent and child perceptions regarding the stigma related to the use of mental health services. In addition, insurance design, reimbursement strategies, availability of specific types of psychotherapy, and wait lists may all contribute to failure to receive psychosocial services.
Our finding that children from African-American, Latino, or other racial-ethnic minority groups were more likely than white children to receive concurrent therapy was consistent with prior studies showing that for the treatment of other mental disorders, African Americans and Latinos find the use of other classes of psychotropic medications less acceptable than do whites and, in many cases, appear to prefer receiving nonpharmacologic interventions (
41,
42). However, currently relatively little empirical information is available regarding how those factors influence parents' choice to use antipsychotic medications versus therapy in the treatment of their children, and further research is needed to understand why parents' choice of different treatment modalities varies among sociodemographic groups.
The results of this study must be viewed in the context of its limitations. Our study relied on administrative data that lack rich clinical and social information. Such information, such as the severity of illness and the family's socioeconomic and environmental situation, likely explain substantial variation in use of psychosocial interventions. We note, however, that all individuals were publicly insured and lived in regions with generous mental health benefits. As a result, these factors may play less of a role in our findings than might be the case in a more heterogeneous population. The generous Medicaid mental health benefits may also contribute to higher rates of mental health specialty care than would be seen in other regions.
We do not know if our findings would generalize to areas or states with more restrictive Medicaid mental health benefits. We also do not know if our findings would generalize to a commercially insured population; such insurance commonly reimburses a more limited range of psychosocial treatment options than many states have made available under Medicaid through Home and Community-Based Services waivers. We did not have information on the prior use of medications or therapy. As is common in analyses of Medicaid claims data, we were unable to determine the specialty of the prescribing physician, the discipline of the mental health provider delivering therapy, or other emotional and behavioral services children may have been receiving from non-mental-health clinicians, such as pastoral counselors or school psychologists. We were liberal in our definition of an indicated diagnosis and would have found fewer children receiving antipsychotics for indicated diagnoses if we had restricted our definition to children of specific ages. Finally, although the mean number of sessions received by children receiving therapy was 24, we were unable to determine the nature of the therapy being provided or if the therapy sessions were clinically appropriate, high in quality, or of sufficient duration.These, of course, are the factors that are most relevant to a child's clinical and functional outcome.
Conclusions
Despite these limitations, our findings help to inform our understanding of the treatment received by children being prescribed antipsychotics. Our findings suggest that even with the rapid growth in the use of antipsychotics, they are not being used solely as a substitute for therapy for a majority of children. There remain, however, a substantial number of children receiving antipsychotics who are not receiving any therapy. A number of current efforts are intended to decrease the use of antipsychotics among children, but for children who continue to receive these medications, more information is needed to better understand the factors contributing to the lack of concurrent therapy. Antipsychotics are likely to continue to play an important role in the treatment of severe emotional and behavioral disorders for a relatively small number of children. For these children and their families, it is important that they be aware of and have access to those effective psychosocial interventions that can increase the likelihood of positive clinical outcomes.
Acknowledgments and disclosures
This work was supported by the Department of Psychiatry, University of Pittsburgh, and the Community Care Behavioral Health Organization. The authors are indebted to Judy Dogin, M.D., and the Community Care Performance Management Committee for useful feedback and comments on the manuscript and to Emily Magee, Shari Hutchison, Laura Greenberg, and Amanda Ayers for research assistance.
This research was done when Dr. Stein was an employee of the Community Care Behavioral Health Organization. The other authors report no competing interests.