American Indian and Alaska Native (AI/AN) communities demonstrate high rates of alcohol and substance abuse and suffer disproportionately from their effects on physical and emotional health (
1,
2). This troubling phenomenon has persisted despite extensive research and efforts to improve prevention and treatment (
3–
6). Many argue that AI/AN communities' history of oppression and cultural eradication is the predominant cause of alcohol and substance use problems, and therefore AI/AN cultural beliefs and practices should form the foundation of clinical services (
7–
10). Various authors specifically link the disappearance of AI/AN traditions to increased substance and alcohol abuse (
11–
13). Similar paradigms construct substance dependence as a broken circle with mental, physical, and spiritual dimensions (
14,
15). Such notions draw from AI/AN worldviews that consider health to be directly related to a harmony among the individual, the family, the community, nature, and spirituality. Treatment models that correlate with these culturally based explanations emphasize a return to AI/AN traditions, holistic concepts of wellness (as opposed to discrete, disease-based models), and community-based treatment models that attempt to heal communities in order to heal individual community members (
16–
19).
Various tribes have revived traditional practices in order to develop culturally sound alcohol and substance abuse treatment programs (
20). Several treatment programs utilize spiritual dances and talking circles (a version of group therapy in which participants sit in a circle, often with a group elder leading) and smudging with sweet grass or sage (
21–
24). Naming ceremonies, storytelling, drumming and singing, and preparing traditional meals represent other tribal practices that treatment programs have integrated.
More holistic approaches to sobriety have also emerged, and one prominent example is the Red Road (Wellbriety), which blends AI/AN cultural beliefs and practices with Alcoholics Anonymous. According to creator Gene Thin Elk, the Red Road represents a “holistic approach to mental, physical, spiritual, and emotional wellness based on Native American healing concepts and tradition, having prayer as the basis of all healing.” Wellbriety emphasizes historical trauma as substance abuse's underlying cause and spiritual recovery as the key to attaining sobriety (
17,
18). Several programs rely on similar conceptual frameworks. San Francisco's Friendship House, for example, intertwines a “retraditionalization” program with more conventional substance abuse treatment approaches to “[heal] the soul wounds of Native Americans,” thereby facilitating sobriety (
24). AI/AN communities have also modified Western models of treatment. Alcoholics Anonymous, specifically its adaptation into Wellbriety, serves as the most visible manifestation, but motivational interviewing and the therapeutic community represent two additional examples (
11,
25).
These examples hint at promising, culturally informed approaches to address the enduring problem of alcohol and substance abuse in AI/AN communities. Cumulatively, however, the literature in this important area is limited. Most studies examining how substance abuse treatment programs integrate culture into their services have focused on individual programs and interventions and offer limited insight into the challenges of marrying traditional and biomedical models of care (
22,
23,
26–
29). No multisite studies of alcohol and substance abuse treatment programs for AI/AN communities have assessed this process on a larger scale. Based on 35 interviews conducted at 18 such treatment programs nationwide, this study used qualitative data analyses to determine how alcohol and substance abuse treatment programs for AI/AN communities are integrating culture into their services and to identify associated challenges.
Methods
Data for these analyses were drawn from the second phase of the Centers for American Indian and Alaska Native Health's Evidence-Based Practices and Substance Abuse Treatment for Native Americans project. This project focuses on how substance abuse treatment programs serving AI/AN communities use and perceive evidence-based treatments. The project also examines how these treatment programs design, implement, and assess their services and how they incorporate cultural, evidence-based concepts and healing techniques into these services. An advisory board supports this project. Members include administrators, providers, evaluators from the AI/AN substance abuse treatment community, and researchers with expertise in AI/AN substance abuse treatment and dissemination research.
The advisory board developed interview and focus group guides to generate open-ended conversations about the community the program serves, the services provided and how they were developed, the challenges of providing these services, and the participants' experience with a selected set of evidence-based treatments. The interview and focus group guides included open-ended stem questions designed to steer the conversation through key topics of interest to the research team. Most stem questions also featured probes to explore specific issues if they were not spontaneously identified in the interview or by group participants (such as whether the program felt pressure to provide specific treatments because of accreditation or reimbursement requirements). Copies of these guides may be found online at
www.ucdenver.edu/caianh/ebp.
Settings and participants
Eighteen substance abuse treatment programs serving AI/AN communities participated in the program case study component of this study, which is the focus of these analyses. These 18 programs reside within three tribes, one tribal consortium, and three urban organizations from seven Indian Health Service regions and seven states. Ten programs are located on reservations, three in nonreservation rural areas, and five in urban areas. Tribes or tribal nonprofit organizations operate these programs, all of which receive additional funding from Indian Health Services. The advisory board identified programs on the basis of their reputations for innovative clinical services and to ensure adequate representation of the geographic and cultural diversity of AI/AN communities. Each program approached agreed to participate. Seventy-seven service providers (22 individuals in clinical administrative positions and 55 frontline clinicians) at these 18 programs participated. Twenty gave interviews as key informants, and others participated in 15 focus groups. To assure participants that confidentiality would be protected, we did not collect demographic information from individuals. We maintained confidentiality in order to minimize participant discomfort (which is not uncommon in AI/AN communities given concerns about prior research abuses) (
30,
31) and to facilitate candid responses to our questions. Host tribes and organizations were also assured about maintaining confidentiality, which was a condition of their decision to participate in this research project.
Data collection
Data collection took place from August 2009 through July 2010. The Colorado Multiple Institutional Review Board reviewed and approved all procedures, which also underwent local review processes that always included an administrative review and sometimes included review by a research review committee or a formal institutional review board. At each participating program, we conducted one or more key informant interviews with program staff in clinical administrative positions as well as a focus group with program staff in frontline clinical positions. Because programs from a single tribe, tribal consortium, or urban organization often participated together, focus groups usually included representatives from multiple treatment programs. This arrangement required more effort from the interviewer to collect information about each program, but it allowed for richer conversation, especially given the small size of many of these programs. Key informant interviews lasted 60 minutes, and focus groups lasted 90 minutes (with additional time reserved for completing the consent process). Project directors had the option of distributing interview and focus group guides before the research team's visit. The principal investigator (DN) conducted all interviews, which were recorded; detailed notes were taken as a backup. For their participation, programs received clinical or training materials of up to $300 value. After reviewing a complete description of the study, each participant completed written informed consent.
Data analyses
All interviews were taped and transcribed. In only one instance was the recording quality so poor that we relied on detailed notes for analytic purposes. After transcription, all recordings were destroyed. Qualitative data were analyzed with NUD*IST Vivo software (
32). We applied the principles of grounded theory (
33) to code interview transcripts for key themes relevant to the purpose of this study (
34–
36). [Grounded theory is a research method used mainly in qualitative research. Key points extracted from text are marked as a series of codes. The codes are then grouped with similar concepts in order to generate categories. Through this process, major themes (categories) and subthemes (codes) are identified.] An initial review of the transcripts generated a tentative list of themes; we expanded and modified the coding framework in subsequent reviews. Theme and subtheme prevalence were also noted. RL performed the initial coding, which was reviewed by DN to establish consensus. After confirming major themes and subthemes, we identified exemplary quotes that captured these ideas.
Results
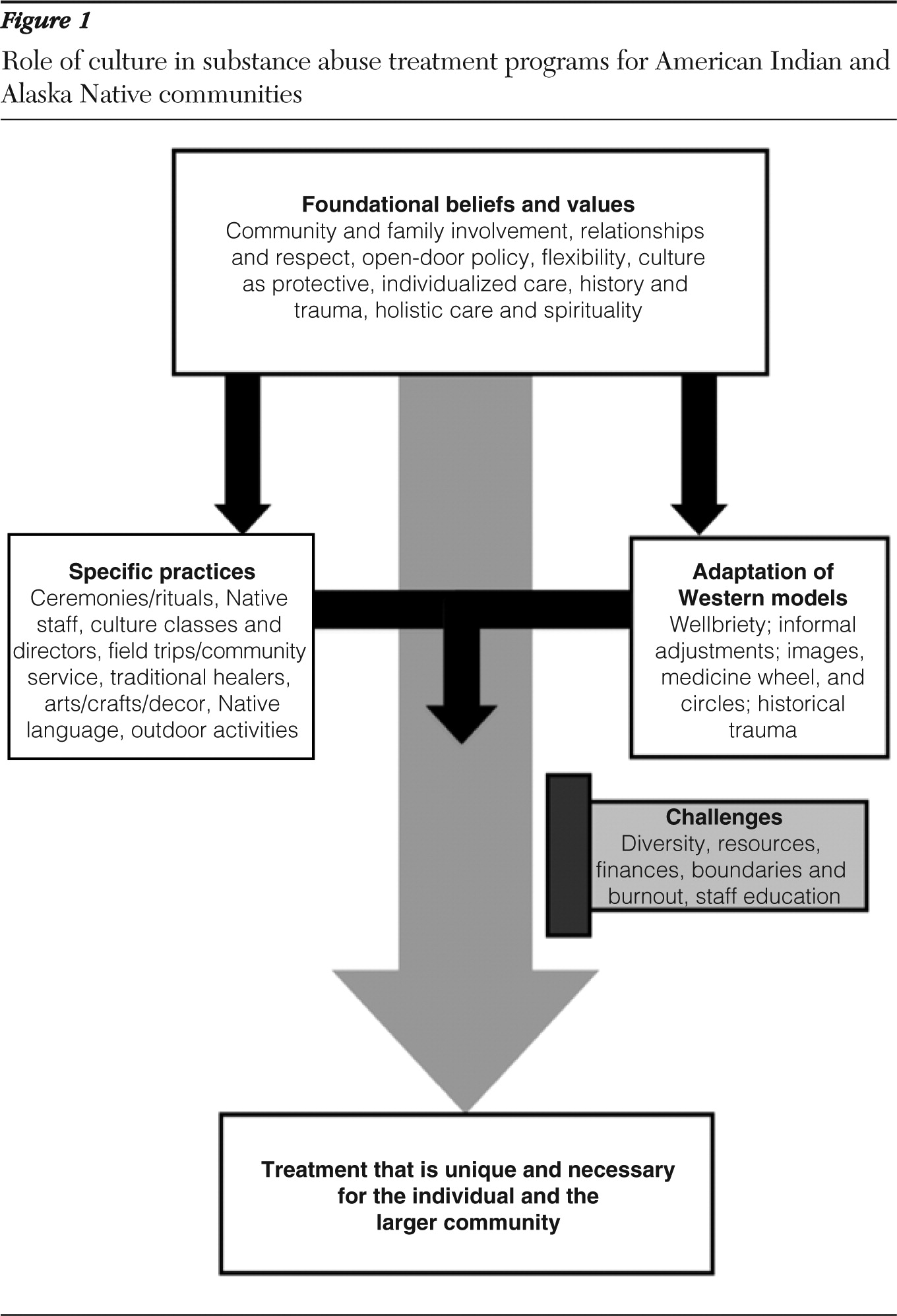
Alcohol and substance abuse treatment programs serving AI/AN communities integrate culture into their services in two discrete ways: by implementing specific cultural practices and by adapting Western models of treatment. More important than either intervention, however, are the foundational beliefs and values upon which they rest. We defined foundational beliefs and values as the core cultural constructs that validate and respect AI/AN experience and world view.
Figure 1 illustrates the relationship between these categories and the challenges of integrating cultural practices.
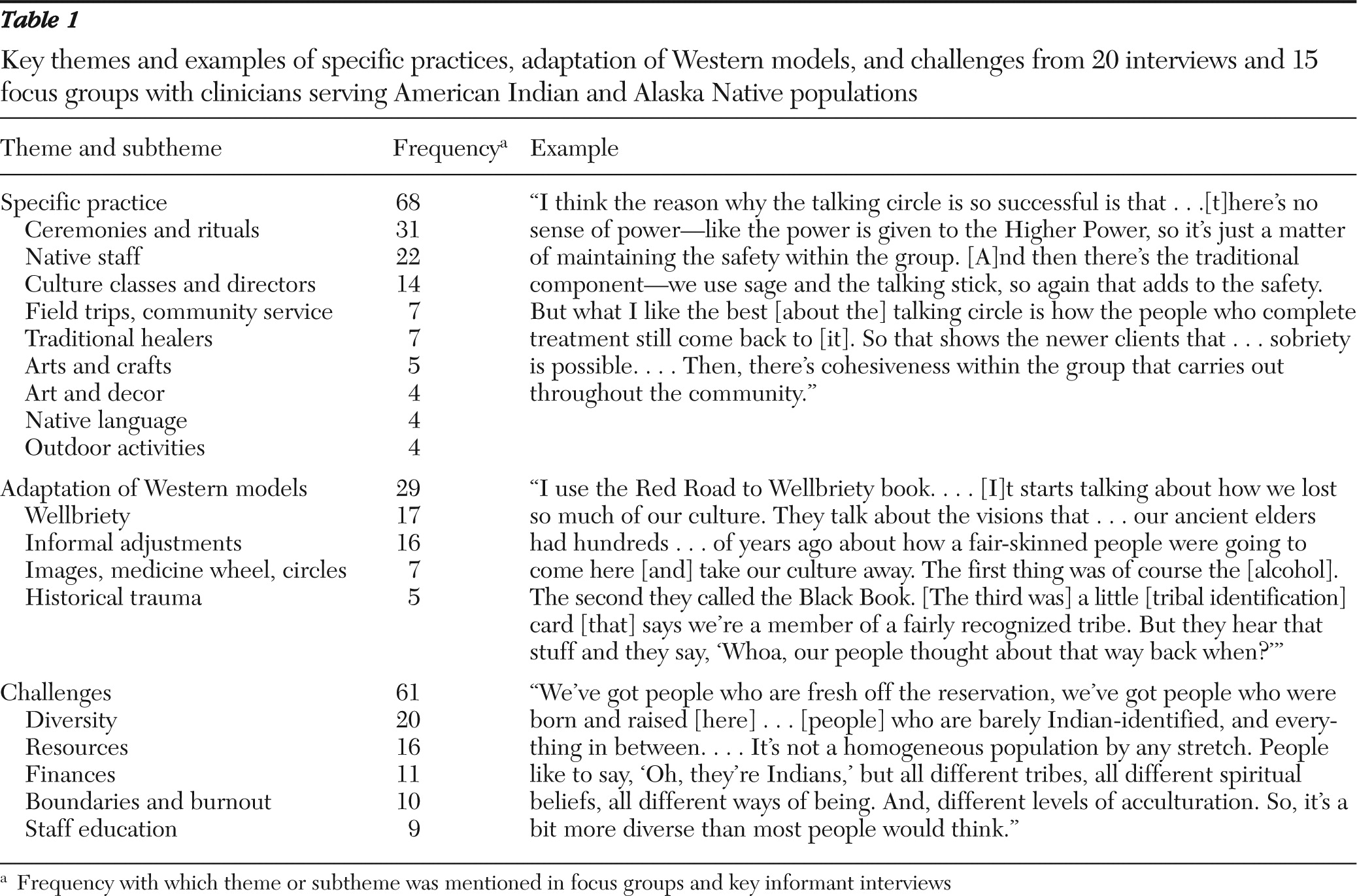
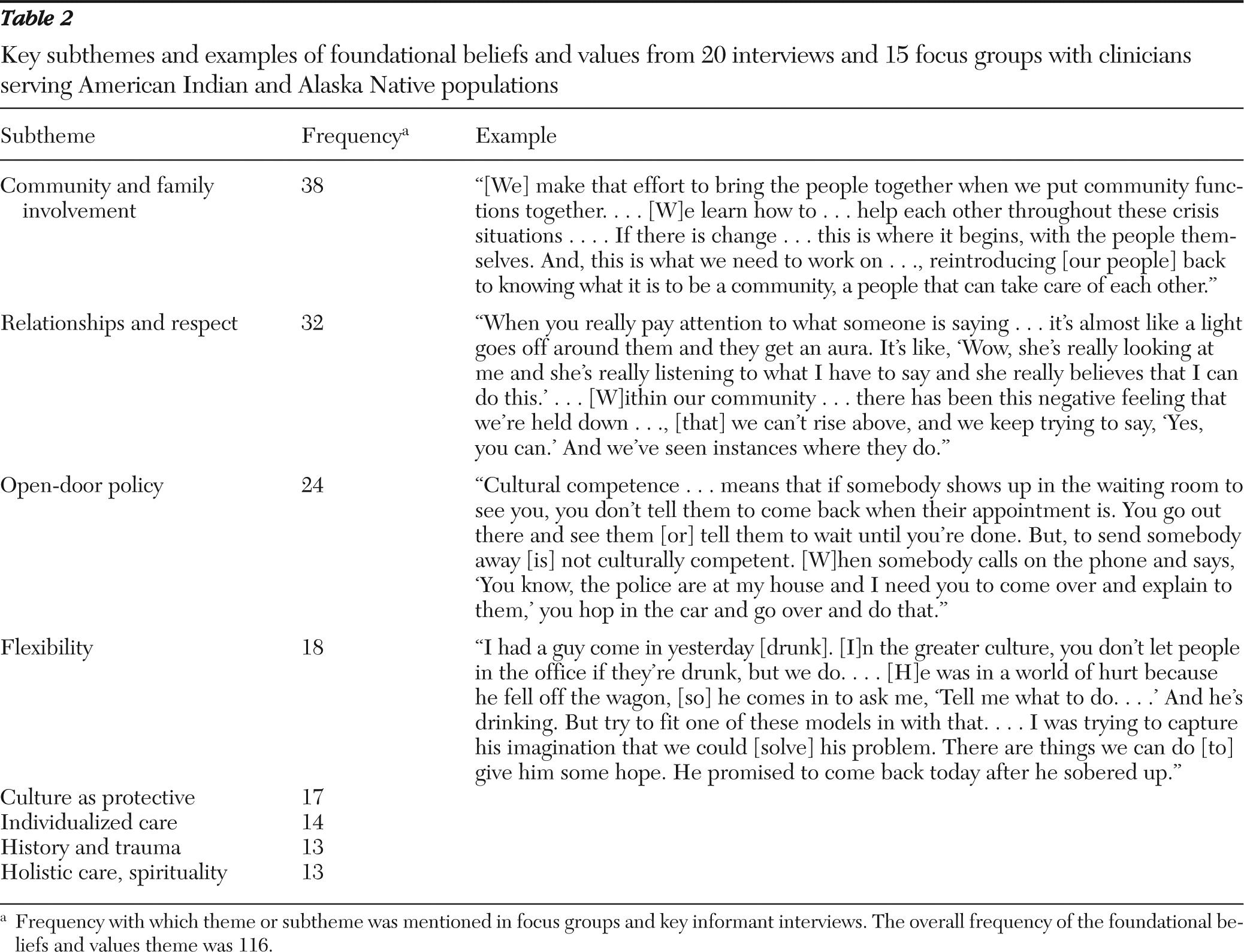
Tables 1 and
2 show the frequency of the most common themes and subthemes and provide exemplary quotations. [Expanded tables with additional exemplary quotations are available online as a data supplement to this article.]
Specific practices
Programs utilize various cultural practices, most frequently ceremonies and rituals, such as talking circles, sweat lodges, and sun dances. Group prayers, powwows, drumming, and musical performances also fall under this category. Clinicians considered these activities an opportunity to interact with clients personally. Clinicians also emphasized connecting clients to their traditional culture in order to reconnect them to their communities, to help them “find out who they are,” and to illustrate a positive aspect of treatment (as opposed to the pathology of substance abuse). Almost all programs hire staff who themselves are AI/AN and described a “different kind of relationship” between AI/AN staff and clients—one based on cultural ties and shared experience that facilitates trust and openness. Other common practices include teaching culture classes or hiring a cultural director to engage clients in community-based activities and mentoring from elders. Participants also noted arts and crafts projects, such as beading, pottery, and carving; field trips to sites of cultural significance; outdoor activities, such as camping, hunting, and fishing; and inviting a traditional healer to participate in treatment.
Adaptation of Western models
Relying on established, Western models of care and adapting them for AI/AN communities is the second discrete way that alcohol and substance abuse treatment programs for AI/AN communities integrate culture into their services. This practice takes place formally through the implementation of Wellbriety and other Western models (for example, the Matrix [37]) that have already been adapted for AI/AN communities. Individual programs also create novel “blended” treatment manuals that incorporate AI/AN imagery, such as medicine wheels, totem graphics, and circular motifs. More commonly, however, adaptations transpire informally when a clinician spontaneously makes minor alterations (usually verbally) in his or her interactions. For example, clinicians may incorporate historical trauma or allude to medicine wheel imagery. Most frequently, programs emphasized their reliance on Wellbriety, which combines the 12-step approach of Alcoholics Anonymous with AI/AN teachings. Programs either directly utilize the Wellbriety model or integrate aspects of it into their Western models of treatment.
Foundational beliefs and values
An emphasis on community and family, the importance of relationships and respect for clients, an open-door policy that welcomes clients into a homelike setting, and the conviction that AI/AN culture and tradition support sobriety represent the most critical beliefs and values guiding treatment at alcohol and substance abuse treatment programs for AI/AN communities. Along with flexibility and offering individualized care, these principles provide the foundation and context that facilitate implementing specific cultural practices and adapting Western models. More important, these foundational beliefs and values function independently as critical components of culturally based care that validate and incorporate AI/AN experience and world view.
Community and family involvement, the most frequently cited foundational component, is stimulated by organizing community-wide social and cultural events, supporting clients beyond program walls (at home or at school, for instance), and bringing spouses and children into programming. One clinician described how “you have to be involved in the community [to] work here—that's part of the program.” Multiple participants reported reintegrating clients into their families and communities in order to sustain sobriety. Conveying an equally prominent foundational value, one clinician related, “It's all about building relationships with people. … If you don't have that …, there's no hope for change.” Meaningful relationships based on respect facilitate empowerment and self-esteem, considered critical given AI/AN communities' shared history of oppression and mistreatment. Such relationships are also therapeutic. One clinician explained, “Our people are traumatized. … What they need is a lot of TLC coming in …. When you give TLC to people who need it, it's amazing what it does to their level of motivation.”
Numerous programs endorse open-door policies that allow clients to ask for help beyond their scheduled appointment times. “Because if you refuse them help, like you close the door and say ‘I'm too busy,’ ” one clinician explained, “they will never come back.” Creating such a receptive environment facilitates a homelike atmosphere where clients feel comfortable asking for help. Flexibility, specifically bending rules and modifying treatment modalities, emerged as another therapeutic approach that allows clinicians to accommodate their clients' multiple, complex needs. For clients who do not meet criteria for treatment, one clinician described how “we may change some things and try to help them through those challenges … and help them complete their program versus just discharging them.” Another clinician, capturing the importance of flexibility, described shaping treatment “so that it fits our population instead of trying to get our population to fit the therapy.” Individualized, client-centered care works in conjunction with flexibility to generate the most therapeutic (and at times, unconventional) care. Last, multiple programs underscore how culture protects against substance abuse by restoring clients' identity and nurturing the values necessary to heal AI/AN communities. “When they set foot into a Native organization where they feel comfortable, they start to heal,” one clinician related. “It's that cultural identity coming back.”
Challenges
The complex diversity of AI/AN populations represents the most frequently identified challenge of implementing culturally based services, with diversity stemming from degree of acculturation, tribal affiliation, religious beliefs, and rural versus urban background. Clinicians and administrators described how culturally sensitive care for one AI/AN client might be insensitive or offensive to another. Lack of resources, specifically traditional healers and the funds to hire staff knowledgeable about cultural practices, emerged as another significant barrier. Other challenges include pressure from grants to implement evidence-based treatments, billing insurance companies for cultural practices, and the potential for burnout and personal boundary violations among clinicians in the context of offering comprehensive, individualized care. Beyond the challenges unique to implementing culturally based care, programs emphasized barriers affecting all aspects of care more broadly, citing, for example, inadequate public transportation and child care services in rural regions and limited socioeconomic resources.
Discussion
This project represents the first multiprogram study of how alcohol and substance abuse treatment programs serving AI/AN communities integrate culture into services. Our finding that culturally based care includes traditional practices and Western models of care adapted for AI/AN communities is consistent with descriptive and case-based studies (
18–
24,
26–
29,
38). However, the critical emphasis on foundational beliefs and principles—defined as core cultural constructs that validate and respect AI/AN experience and world view—represents a novel finding, one that calls for a more profound understanding of AI/AN history, reality, and perspective when providing services. This emphasis also questions conventional conceptions of culturally based care. As one administrator commented, “It's not just about … the ceremonies. … It's about being responsive to the community, which [means] being culturally competent.” Involving community and family, emphasizing relationships and respect, and maintaining an open-door policy form the foundation for culturally relevant interventions. Rebuilding existing treatment modalities upon this foundation and advancing all foundational beliefs and values independently enable cultural adaptation and modification in substance abuse treatment programs for AI/AN communities.
To address the substance abuse treatment needs of diverse communities, an emerging body of literature describes the importance of marrying culture with evidence-based interventions and other treatment manual-based interventions (
39,
40). Our findings share points of continuity with theoretical frameworks that illustrate this process. These frameworks suggest that similar cultural constructs, including family, respect, spirituality, and traditionalism, should be integrated into substance abuse prevention and treatment in order to gain acceptance from ethnic and racial minority groups (
39,
41). These frameworks also distinguish between surface modifications (for example, implementing relevant language, music, and food) and deep structures, or the cultural, social, historical, environmental, and psychological factors that influence the target health-related behavior. Surface structures increase acceptance of messages, whereas deep structures convey relevance and determine impact (
42,
43). Conceptualizing the prominence of foundational beliefs and values as the backbone of care has a correlation with these deep structures (
Figure 1). Several studies that have examined the role of culture in substance abuse interventions for other minority communities align with our emphasis on community, family, relationships, respect, and the role of history and trauma (
44–
46). These particular themes, common to various minority communities, suggest a starting point for devising guidelines that operationalize the cultural adaptation of substance abuse treatment paradigms.
This study's primary shortcoming involves the sampling of programs. Because we selected programs that provide innovative services, we were unable to address the tremendous diversity of AI/AN communities. We hope to pursue this matter during the final phase of this project, which involves a nationwide survey of substance abuse programs serving AI/AN communities that explores similar themes through quantitative methods. Because we did not obtain demographic information from clinicians and administrators, we were unable to examine the relationship between factors such as ethnicity and years of experience and descriptions of culturally based care, but the small sample size would have likely precluded such analyses.
Conclusions
For these 18 substance abuse treatment programs serving AI/AN communities, culturally based care goes beyond traditional practices and adapting Western models of care. Instead, these approaches are derived from foundational beliefs and values that reflect these communities' worldview, shared history, and current challenges. We defined these foundational beliefs and values as the core cultural constructs that validate and respect AI/AN experience and world view. Our observation that culturally based care informs the foundation and structure of substance abuse treatment programming and extends into the larger community carries significant implications for other diverse communities. Our findings might help other substance abuse treatment programs integrate culture into their services in order to develop unique treatment strategies that concurrently heal individuals and their surrounding communities.
Acknowledgments and disclosures
This work was supported in part by grant R01-DA022239 from the National Institute on Drug Abuse. The authors also acknowledge the Centers for American Indian and Alaska Native Health's Substance Abuse Treatment Advisory Board, which includes the following members: Gregory A. Aarons (University of California, San Diego); Annie Belcourt (University of Colorado Denver); Gordon Belcourt and Kathleen Masis (Montana-Wyoming Tribal Leaders Counsel); Sarah G. Conti (Pagosa Springs, Colorado), Dennis Dahlke (Peaceful Spirit Alcohol Recovery Center), Raymond Daw (Navajo Department of Behavioral Health Services), Daniel Dickerson (United American Indian Involvement/University of California, Los Angeles), Darren Dry (Jack Brown Center), Alexandra Fickenscher (emeritus) and Candace Fleming (Centers for American Indian and Alaska Native Health); John Gastorf (Cherokee Nation Behavioral Health); Craig Love (Westat); Traci Rieckmann (Oregon Health and Sciences University); and Paul Spicer (University of Oklahoma).
The authors report no competing interests.