As Operation Iraqi Freedom (OIF) and Operation Enduring Freedom (OEF) wind down, troops are returning from deployment in greater numbers than ever. National Guard (NG) soldiers increasingly have been relied upon by OIF/OEF. Approximately 75% of all NG soldiers have been activated since 2001 (
1). In at least two respects, NG soldiers are a unique population with regard to mental health and access to treatment. First, they must transition quickly and frequently between military service and civilian life. Second, unlike active military personnel, who have access to U.S. Department of Veterans Affairs (VA) services, coverage and access to health care vary in this population. Other obstacles include the need to take time off from civilian employment and the need to travel long distances to the nearest contracted provider. Adding to the challenges are the shortage of TRICARE providers taking new patients and a lack of appointments in the evening or on weekends (
2).
The evidence available to date suggests that NG soldiers have high levels of unmet need for mental health treatment (
3–
5). Specifically, mental health service use appears to range from about 44% to 53% (
5,
6). Two prior studies have provided information on specific types of care sought by NG soldiers for mental health problems (
5,
6). Gorman and colleagues (
5) reported sources of care among those who screened positive for mental health problems 45 to 90 days after returning from deployment. Seeing a physician at a military facility was most common (29%), followed by seeing a military chaplain (23%) and a mental health professional at a military facility (20%). Kehle and colleagues (
6) found that individual therapy (20%) and medication consultation (10%) were the most commonly used types of individual treatment during the three to six months after returning home from a 16-month deployment in Iraq.
A number of earlier investigations, including the study by Kehle and others (
6), have documented the correlates of mental health service use among NG soldiers. Kehle and colleagues (
6) examined treatment seeking among NG soldiers who were screened for mental disorders after the end of their deployment. They found that 50% of those who screened positive for posttraumatic stress disorder (PTSD) symptoms and 40% of those who screened positive for major depressive disorder had not sought treatment between two and three months after the screening (
6). Increased mental health service use among NG soldiers has been associated with PTSD symptom severity (
7) and with increased postdeployment stress or readjustment difficulty (
7,
8). Postdeployment adjustment difficulties have also been found to be associated with psychotherapy and medication use (
6) among NG soldiers returning from Iraq.
However, previous studies had a number of features that may limit their generalizability. First, to our knowledge, prior studies in this area have all exclusively recruited NG soldiers who have returned from OIF/OEF deployment within the past 12 months. Therefore, results may not be generalizable to the entire NG population. Second, with one exception—a study by Meis and others (
7) that assessed a volunteer sample of NG soldiers and their partners three months postdeployment and again 12 months later—previous studies have been cross-sectional. Therefore, it is difficult to confirm the sequence of mental health problems and use of mental health services. Given the complexities of accessing care associated with each form of military group membership, understanding predictors and barriers specific to NG soldiers is needed. NG soldiers who are deployed have access to VA services for five years postdeployment. Whether and to what degree access to these services (or lack thereof for those not deployed) affect mental health service use have not been examined.
This study aimed to address three questions. First, what is the prevalence of mental health service use among NG soldiers? Second, can we identify predictors of mental health service use among NG soldiers? Third, can we identify specific types of mental health services that are used by NG soldiers?
Methods
Study population and survey
Data were drawn from the Ohio Army NG Mental Health Initiative (OHARNG MHI). The OHARNG MHI is a dynamic longitudinal cohort of Ohio Army NG soldiers who are interviewed annually to assess mental health, substance use, and life experiences. All soldiers were asked to participate in the study with the option to opt out. Between June 2008 and February 2009, a total of 11,212 soldiers did not opt out of the study, and accurate contact information was available for 6,514 (58%) participants. Of these 6,514 soldiers, 4,198 were contacted before we reached our target sample of eligible participants (N=2,616); therefore, 2,316 (36%) participants had not been contacted when the baseline cohort closed. Among the 6,514 for whom contact information was received, 187 (3%) were ineligible (for example, because they were too young or were retired), 31 (1%) were disqualified (did not speak English or had problems hearing), and 1,364 (21%) did not wish to participate. The overall response rate was 43%, calculated as the number of participants who completed a survey or who consented but were ineligible divided by the number of working telephone numbers minus those that were disqualified (N=2,616+187/6,514–31).
Baseline interviews were conducted between November 2008 and November 2009 (wave 1). Participants were contacted for follow-up interviews one year later during wave 2 (November 2009–November 2010), and again during wave 3 (November 2010–November 2011). A total of 1,770 (68%) soldiers from the original group of 2,616 responded to the wave 2 follow-up survey; we restricted the final sample to soldiers who participated in both waves 2 and 3 (N=1,189). As reported previously (
9), our sample was demographically comparable to the entire OHARNG at time of sampling, although the sample participants were slightly older and less likely to be married. Factors associated with loss to follow-up between waves 1 and 2 included age (p<.001), with the youngest (18–25 years old) least likely to return; race (p<.05), with blacks least likely to return; marital status (p<.001), with those who were never married least likely to return; education (p<.001), with those having the lowest level of education least likely to return; and rank (p<.01), with enlisted individuals least likely to return. Factors associated with loss to follow-up between waves 2 and 3 included age (p<.01), with the youngest group least likely to return; marital status (p<.01), with those who were divorced, separated, or widowed least likely to return; education, (p<.001), with those having the lowest education (high school graduate, GED, or less) least likely to return; and psychopathology (p<.01), with those who had psychopathology less likely to return.
After giving informed consent, soldiers participated in telephone interviews that collected information on mental health, substance use, military experiences, and life events history. The study design was reviewed by the University of Michigan and the Case Western Institutional Review Board, and the informed consent of the participants was obtained after the nature of the procedures had been fully explained.
Measures
Sociodemographic factors included gender, age, race-ethnicity, income, health insurance status, education level, and marital status. Age was divided into categories of 18–24, 25–34, 35–44, and ≥45. Race categories included white, black, and other race, and ethnicity included Hispanic and non-Hispanic. Income was measured as ≤$60,000 or >$60,000. Insurance status was measured as a dichotomous variable indicating presence or absence of health insurance. Military factors included rank (officer or enlisted, cadet, or civilian employee status) and deployment experience (none, deployment to Iraq or Afghanistan, or other).
Clinical in-person validation study
We recruited a random subsample of 500 participants who were compensated for participating in an in-person clinical validation interview in addition to their telephone interviews (
10). In-depth, in-person interviews were conducted by clinicians at a location or setting familiar to the participant and lasted an average of two hours. Diagnoses of PTSD, depression, generalized anxiety disorder, and alcohol abuse and dependence as well as suicidal ideation were validated by comparing telephone interview diagnostic assessments with in-person diagnostic assessments.
Posttraumatic stress disorder
We assessed PTSD at wave 2 consistent with
DSM-IV criteria. To screen positive for PTSD, participants had to meet all
DSM-IV criteria. Criterion A1 (directly experiencing the traumatic event) was assessed with a list of 25 potentially traumatic non–deployment-related experiences and a list of 45 potentially traumatic deployment-related experiences. The list of potentially traumatic non–deployment-related experiences included items from the Life Events Checklist in the Clinician-Administered PTSD Scale (CAPS) (
11,
12) and items commonly used in population-based studies (
13). The list of potentially traumatic deployment-related experiences included the 25 nondeployment experiences asked in the context of deployment and an additional 20 experiences from the Deployment Risk and Resilience Inventory (
14). Criterion A2 (witnessing the event as it occurred to others) was assessed by asking participants whether they felt terrified or helpless while watching the occurrence of an event that they self-identified as the “worst.” Criterion B (re-experiencing the event), criterion C (avoidance and numbing), and criterion D (hyperarousal) were assessed by using questions from the PTSD Checklist–Civilian Version (PCL-C) (
15,
16). Finally, we assessed criterion E (greater than one month’s duration of symptoms) and criterion F (clinically significant impairment) by asking participants about the duration of their illness and degree of impairment. PTSD was validated in this sample with CAPS results from the clinical in-person validation study; the sensitivity, specificity, and Cronbach’s alpha, respectively, were comparable across deployment-related (.50, .93, and .95) and non–deployment-related (.47, .94, and .93) assessments (
10).
Depression
The Patient Health Questionnaire–9 (PHQ-9) (
17) was used to evaluate depression symptoms at wave 2 on the basis of
DSM-IV criteria. Each of the nine questions is scored as 0 (not at all) to 3 (nearly every day), with total scores ranging from 0 to 27. Individuals who met criteria for either major depressive disorder or other depressive disorder and reported that his or her symptoms seemed to have occurred together were identified as having depression. Other depressive disorder was diagnosed if two to four depressive symptoms were present for at least “more than half the days” in the past two weeks, and one of the symptoms was depressed mood or anhedonia. Major depressive disorder was diagnosed if five or more of the nine depressive symptoms that constitute
DSM-IV criteria were present for at least more than half the days in the past two weeks, and one of the symptoms was depressed mood or anhedonia. This algorithm was validated against the depression module in the Structured Clinical Interview for DSM-IV Axis I Disorders (SCID I) (
18) and yielded moderate sensitivity (.51), high specificity (.83), and a Cronbach’s alpha of .66 (
10).
Generalized anxiety disorder
To assess generalized anxiety disorder, participants were administered the Generalized Anxiety Disorder Assessment (GAD-7) (
19) at wave 2. The GAD-7 evaluates co-occurring symptoms on a scale of 0, not at all, to 3, nearly every day, with possible scores ranging from 0 to 21. To screen positive for generalized anxiety disorder, a person must have a score of ≥10, have symptoms for at least six months, and report functional impairment. Validated against the generalized anxiety disorder module in the SCID I, generalized anxiety disorder had low sensitivity (.04), high specificity (.96), and a Cronbach’s alpha of .72 (
10).
Alcohol use disorders
A single variable called alcohol use disorders included both alcohol abuse and alcohol dependence, both of which were assessed by using the Mini-International Neuropsychiatric Interview (
20) at wave 2 to evaluate the presence of
DSM-IV criteria. Participants who displayed one or more of the maladaptive patterns that constitute criterion A of substance abuse and whose symptoms led to impairment or distress screened positive for alcohol abuse. Alcohol dependence was classified as displaying three or more of the maladaptive patterns that constitute criterion A of substance dependence and having symptoms that have led to impairment or distress. Validated against the SCID I, alcohol abuse had moderate sensitivity (.40), high specificity (.80), and a Cronbach’s alpha of .57; alcohol dependence had higher sensitivity (.60), comparably high specificity (.81), and a Cronbach’s alpha of .76 (
10).
Mental health service use
To assess past-year use of mental health services at wave 3, participants were asked, “Since we last spoke, did you ever go to see any of the following professionals or self-help groups for problems with your emotions or nerves or for problems with your use of alcohol or drugs?” Participants were then asked whether they received such services through a physician; a psychiatrist; a psychologist; a minister, priest, rabbi, or other spiritual advisor; “another type of mental health professional”; or a self-help group, such as Alcoholics Anonymous and Narcotics Anonymous. Participants were allowed to endorse multiple provider categories. This set of questions was derived from the National Comorbidity Survey (
21).
Statistical analysis
First, we computed chi square statistics examining the relationship between independent variables that were measured at wave 2 and mental health service utilization at wave 3. In addition, we calculated crude odds ratios (ORs) and confidence intervals for mental health service use at wave 3 after adjustment for each independent variable. The variable for “mental health need” was coded positive if any of the mental health conditions described above were present at wave 2.
Second, we performed a multivariable logistic regression analyzing predictors of mental health service use within the entire sample. We included as predictors the independent variables from wave 2 that were significantly related to use of mental health services at wave 3. Third, we performed multivariable logistic regression with the same model but only among participants who had a mental disorder. We performed sequential logistic regressions in the order indicated by
Tables 2 and
3. All comparisons and statistical tests were performed in SAS 9.2.
Results
Mental health service use
Fewer than one in five soldiers (16%) used mental health services in the past 12 months. Several variables were associated with significantly increased odds of using mental health services within the past 12 months at wave 3: being female; insured; divorced, separated, or widowed; and non-Hispanic black or other non-Hispanic race-ethnicity; having poor general medical health; and having mental health need, including suicidal ideation, at wave 2 (
Table 1). Age, income, rank, and deployment experience were not significantly associated with mental health service use.
Predictors of mental health service use
After adjusting for all factors that were significantly associated with mental health service use, being female (OR=1.7), non-Hispanic black (OR=2.3), Hispanic (OR=2.6), and insured (OR=2.8) and having poor general medical health (OR=1.9) and mental health need (OR=4.8) were associated with increased service use (
Table 2).
Predictors of service use among those with mental health need
Among the 227 participants with mental health need at wave 2, 85 (37%) used mental health services in the 12 months prior to wave 3. Being non-Hispanic black (OR=4.1) was the sole significant predictor of mental health service use at wave 3 when all other variables were entered into the model (
Table 3).
Type of mental health service use
Of those with mental health problems who used any mental health service, over half saw a physician (59%) or a psychologist (51%), and nearly half (45%) saw a psychiatrist (
Table 4). Over a quarter (28%) reported seeing clergy or a spiritual advisor, and a relatively small percentage (10%) reported use of self-help groups.
Mental health need at baseline and mental health service use
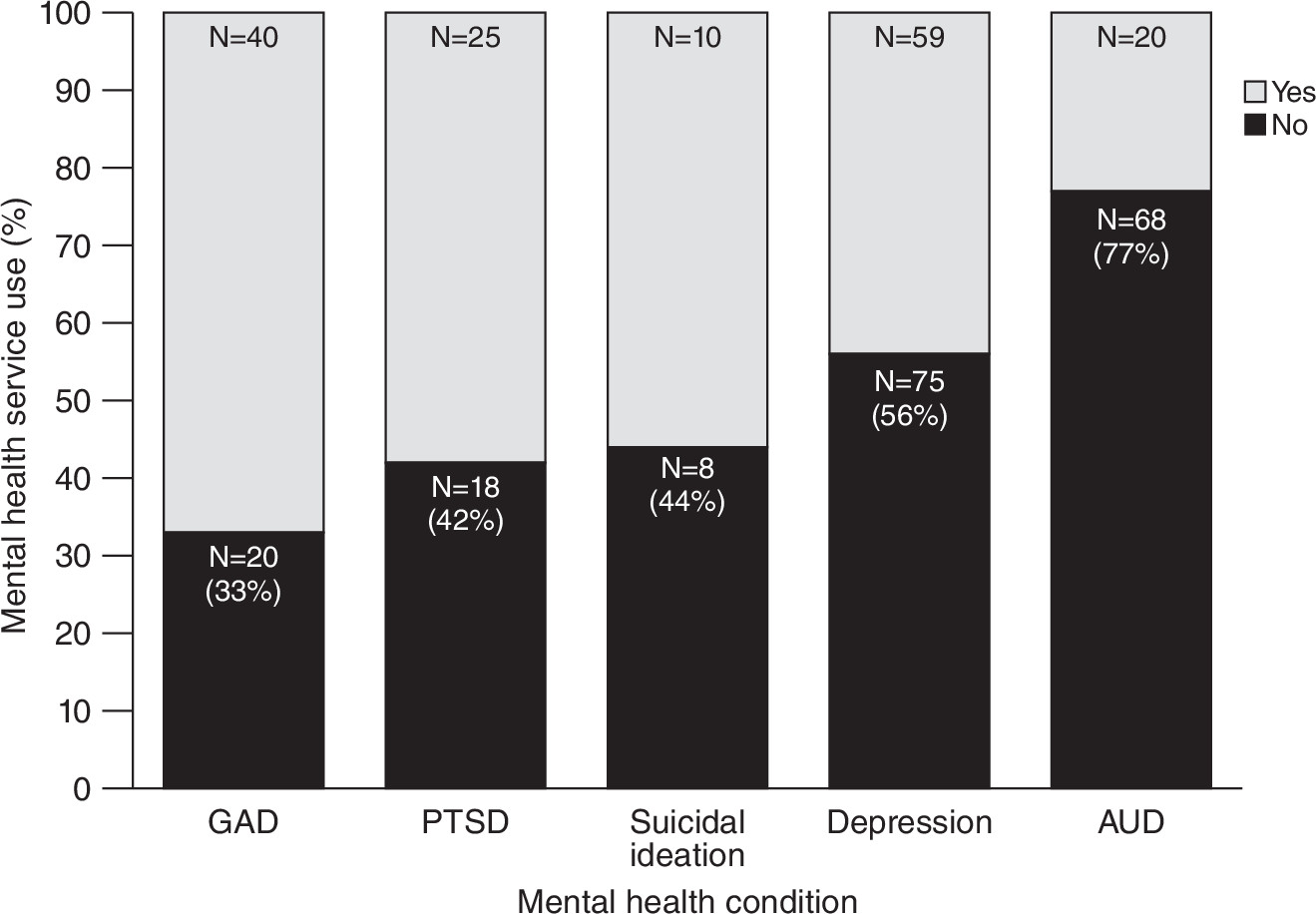
As shown in
Figure 1, mental health need at wave 2 was associated with differential use of services during the following 12 months. Participants with depression or alcohol use disorders were less likely than participants with other mental health problems to access mental health services. There was also a dose-response relationship between number of disorders and prior-year use of mental health services. [A figure illustrating this relationship is available online as a
data supplement to this article.]
Discussion
Three main findings emerge from our study. First, we found that 16% of a representative sample of NG soldiers used mental health services in the 12-month follow-up period. Among participants with mental health need, 37% reported service use. Second, both demographic (being female and insured) and general medical and mental health factors predicted service use in the general sample of NG soldiers. Third, among participants with mental health need, being black emerged as the only significant predictor of service use.
Compared with prior studies using NG samples, we found lower rates of mental health service use. Specifically, in our sample, 16% reported using mental health services in the past year compared with rates of between 30% and 50% reported by previous studies (
6). Previous samples were recruited from among NG soldiers who had previously been deployed (
5), and our study used a representative sample of Ohio NG soldiers. This sample included, but was not limited to, those who had recently returned from deployment. It seems reasonable that a sample of NG soldiers who had returned from deployment very recently might have higher levels of mental health service use than a general sample, such as the one in this study.
In this study we examined the potential role of demographic characteristics and mental health problems in predicting mental health service use. We found, not surprisingly, that mental health need was a stronger predictor of mental health service use than any other factor and remained statistically significant after controlling for all other variables measured. This finding is fairly consistent with previous results on predictors of mental health service use. For instance, Kehle and others (
6) found that positive screens for PTSD and depression were significantly more likely than negative screens to be associated with receiving psychotherapy or medications. It is also important to note that insurance remained a strong and significant predictor of service use among those with mental health need. This finding, indeed, suggests that lack of insurance may be a barrier to service use for this population, drawing a sharp contrast with active duty soldiers, who can rely on VA services. In fact, Gorman and others (
5) have noted that the cost of mental health services was an issue for 37% of NG soldiers who met criteria for at least one mental health problem. Once a reserve soldier is assigned to a specific unit, however, barriers to seeking mental health care—such as needing to take time off work for an appointment, providers’ limited office hours, or lack of access to a military treatment facility or VA provider—decline substantially compared with obstacles faced by NG soldiers in their civilian life. Yet, barriers to mental health treatment among reservists remain a unique challenge.
Two central limitations of our study should be noted when interpreting results. First, our sample was representative only of the Ohio NG, and, therefore, the findings may not generalize to other state-level NGs. Second, we did not have information about several factors—such as fear of stigma, cynicism, and concern that use of mental health services would prohibit redeployment and career advancement—that have been found to be related to use of mental health services in active military populations (
22–
26). Future studies that examine these factors as determinants of mental health may more fully help to understand mental health service use in this population.
Conclusions
The results suggest that there is a substantial level of unmet need for mental health treatment among NG soldiers. Efforts toward identifying NG soldiers with a need for mental health services and improving access to care might be warranted.
Acknowledgments and disclosures
This study was funded in part by the Congressional Department of Defense Appropriation W81XWH-O7-1-0409/W81XWH-10-1-0579 sponsored by Congresswoman Marcy Kaptur of Ohio’s Ninth Congressional District.
Dr. Calabrese receives research support from, has consulted to, has served on the advisory boards of, or conducts continuing medical education supported by Abbott, AstraZeneca, the Brain & Behavior Research Foundation (formerly the National Alliance for Research on Schizophrenia and Depression), Bristol-Myers Squibb, Cephalon, Cleveland Foundation, Dainippon Sumitomo, Eli Lilly, EPI-Q, Inc., Forest, France Foundation, GlaxoSmithKline, Janssen, Johnson & Johnson, Lundbeck, Merck, NARSAD, Neurosearch, OrthoMcNeil, Otsuka, Repligen, Sanofi Aventis, Schering-Plough, Pfizer, Servier, Solvay, Stanley Medical Research Institute, Sunovion, Supernus, Synosia, Takeda, and Wyeth. The other authors report no competing interests.