Behavioral health problems, including serious psychological distress and substance use disorders, are associated with higher rates of morbidity, mortality, and disability. It has been estimated that the global societal costs associated with behavioral health problems exceed $2 trillion annually and are expected to continue to grow (
1). Previous studies have found significant associations between behavioral health and economic conditions. For example, many studies examining mental health and the economy found associations between unemployment and mental health problems (
2–
12), between unemployment and mental health service utilization (
13), and between detrimental economic events (such as reduced income, financial strain, loss of investment wealth, food insufficiency, and recession) and mental health problems (
5,
8,
14–
16).
Studies of economic conditions and substance use provide conflicting results. Some studies suggest that adverse economic conditions lead to increased substance use, perhaps in response to stressors associated with an economic downturn or increased availability of leisure time due to unemployment (
6,
17–
22). Other studies suggest that reductions in income during adverse economic conditions lead to decreased substance use (
23–
27). These conflicting findings may result from differences among the studies in the choice of economic measures, such as unemployment, poverty, and gross domestic product contraction; measures of substance use, such as per capita consumption, self-reported individual consumption, and alcohol sales data; and level of analysis, for example, individual level versus population level (
5). In addition, most substance use studies use alcohol consumption levels to identify problematic substance use rather than diagnostic criteria for an illicit drug or alcohol use disorder (
28,
29).
Few studies have assessed the degree to which the economic situation in a community is associated with an individual’s mental health and substance use, after controlling for the individual’s own economic situation, such as employment status and family income (
30). Combining individual-level and community-level data, such as overall economic well-being at the state level or county-level unemployment, provides a more comprehensive picture of the relationship between behavioral health and the economic environment. Theory suggests that behavioral health is a function of socioeconomic, biological, and environmental factors (
31). The economic climate may affect behavioral health directly at the individual level through various economic consequences, such as underemployment, job loss, or income loss. However, severe economic conditions also may affect individuals who remain employed or do not experience personal income contraction (
5). For example, employed individuals living in a community with high unemployment or job layoffs may suffer anxiety about the prospect of losing their jobs (
5).
This study examined the associations between several diverse measures of macroeconomic conditions and the following outcomes: serious psychological distress, substance use disorders, and mental health service utilization. Particularly, this study examined the effects of the housing market on behavioral health outcomes—a relationship that has not been widely examined despite the critical role of housing in the recent economic climate. We used data from the National Survey on Drug Use and Health (NSDUH), providing nationally and state representative data on mental health and substance use among the U.S. civilian, noninstitutionalized population ages 18 or older, to best capture the complex relationships between the economy and behavioral health.
Methods
Data
This study examined restricted-use data from approximately 21,100 persons ages 18 or older who participated in the NSDUH in 2008, 2009, or 2010. The NSDUH is a cross-sectional survey conducted annually by the Substance Abuse and Mental Health Services Administration (
32). Data are collected by interviewers in personal visits to households and noninstitutional group quarters via personal interviewing and audio computer-assisted self-administered interviewing. We used the pooled NSDUH data from 2008–2010, a period corresponding with the recent recession and characterized by considerable variation in macroeconomic indicators. In particular, the recent recession, which has been labeled as the most severe economic downturn in the United States since the Great Depression (
33), represented a period of dramatic change in economic conditions, including an extended duration of high unemployment and a severe mortgage crisis.
To ensure individuals were exposed to similar periods of changing economic conditions across states, the analysis included the first 18 months of each state’s recession period. Moreover, because the outcome measures refer to experiences in the previous 12 months, the sample included only adults who were interviewed in months 13 through 18 of this period. Six states (Alaska, Minnesota, North Dakota, Oklahoma, South Dakota, and Wyoming) with recession periods of less than 18 months were excluded from the analysis.
Outcome Measures
Our outcome measures comprised past-year serious psychological distress, substance use disorders, and mental health service utilization. Persons experiencing serious psychological distress were identified on the basis of the Kessler Psychological Distress Scale (K6), a nonspecific psychological distress indicator of past-year mental health problems, such as anxiety and mood disorders (
7,
34,
35). The K6 assesses the frequency with which a respondent experienced six symptoms of nonspecific psychological distress during the one month in the past 12 months in which the respondent reported feeling at his or her worst emotionally. Respondents with a score of ≥13 (possible scores range from 0 to 24) are considered to have serious psychological distress (
7,
34). Persons with substance use disorders in the past 12 months were identified by using criteria specified in
DSM-IV (
36,
37), including dependence on or abuse of alcohol or illicit drugs. Mental health service utilization was defined as receipt of any mental health services, including outpatient or inpatient mental health treatment or use of prescription medication for a mental health problem, in the past 12 months (
34,
38). Because we considered utilization an indicator of treatment access, we limited our analyses of mental health service utilization only to persons with serious psychological distress. This allowed us to analyze the association between service utilization and covariates among a selected sample identified as in need of such services (persons with serious psychological distress).
Covariates
The main explanatory variables of interest were three variables designed to capture states’ recent macroeconomic conditions. An a priori expectation was that a worse economic climate would be associated with poorer behavioral health outcomes. The State Coincident Indexes (SCIs) of economic activity (
39) summarizes each state’s current economic conditions. SCIs are based on four state-level economic indicators: nonfarm payroll employment, the unemployment rate, average hours worked in manufacturing, and wages and salaries (
40). SCIs rise as economic conditions improve and fall as conditions deteriorate (
41). For each individual sampled, we derived the past-year average SCI for the state in which he or she resided.
The SCI composite score does not include housing market measures. Therefore, we also included the serious mortgage delinquency rate, which captures a state’s recent housing market experience (
42). This measure is defined as the proportion of home loans in foreclosure or 90 days past due on payment. For each individual sampled, we derived the past-year average serious mortgage delinquency rate for the state in which he or she resided. The labor market condition faced by each individual was captured by the past-year average unemployment rate for the county in which he or she resided. For ease of interpretation, we developed categorical variables (quartiles) of the macroeconomic measures for inclusion in our model.
We also controlled for individual-level demographic and socioeconomic characteristics, such as age, gender, race-ethnicity, educational attainment, employment status, family income as a percentage of federal poverty level (FPL), health insurance status, and marital status. The model for mental health service utilization also included a continuous K6 score for level of psychological distress and a measure of perceived need derived from the survey question, “During the past 12 months, was there any time when you needed mental health treatment or counseling for yourself but didn't get it?” Response options were yes and no.
Finally, because of the timing of our data, we derived a measure of recession duration for each individual sampled, calculated as the time between the interview date and the beginning of the state’s recession. We defined the beginning of each state’s recession as the first month in a period of three or more consecutive months during which the state experienced a cumulative decline in its SCI of .5% or more.
Data Analyses
Our analyses examined the associations between the three macroeconomic variables—SCI, serious mortgage delinquency rate, and county unemployment rate—and our measures of substance use disorders, serious psychological distress, and mental health service utilization among adults experiencing serious psychological distress.
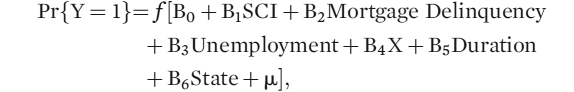
We used multiple regressions to examine associations between the outcomes and macroeconomic variables, holding constant selected demographic and individual-level socioeconomic variables. Because the dependent variables for these models are dichotomous, we used logistic regression (with weights) as indicated below.
In this equation, Y is the discrete behavioral health outcome at the individual level, equal to 1 if the condition existed. SCI is a categorical measure of the past-year average of the SCI for the state in which the individual resided. Mortgage Delinquency is a categorical measure of the past-year average serious mortgage delinquency rate for the state in which the individual resided. Unemployment is a categorical measure of the past-year average unemployment rate for the county where the individual resided. X is a vector that represents various demographic and individual-level socioeconomic characteristics. Duration is the length of an individual’s exposure to recession at the time of interview (in months), which is included as a within-state linear time trend. State is a vector of time-invariant, state-level fixed effects that control for unobserved state characteristics that may be associated with Y.
Analyses used SAS-callable SUDAAN software to account for the complex sample design and sampling weights of the NSDUH. Because we included several economic measures in our models, we performed variance inflation factor analysis to test for the presence of multicollinearity, which was not detected for most variables. Multicollinearity between SCI and some state fixed effects was detected. To determine its impact, we ran a similar model with continuous measures of the macroeconomic variables and without state fixed effects, and we found no statistically significant relationship between SCI and the behavioral health outcomes. For ease of interpretation and to best control for state-specific unobserved effects, we present the findings from the fuller model that included categorical macroeconomic variables and state-level fixed effects.
We should note that accounting for the complex sample design limited our modeling choices. At the time of the study, we were unaware of an appropriate method that would have allowed us to simultaneously use multilevel modeling to adjust for clustering and address the specific survey complexity of the NSDUH (
43). Unlike multilevel modeling, our model accounted for the survey design and used a fixed-effects specification to control for clustering and correct for potential point estimate bias. Our specification included individual-level variables, such as demographic variables, employment status, and family income as a percentage of FPL; macroeconomic variables, such as SCI, serious mortgage delinquency rate, county unemployment rate, and recession duration; and fixed-effects time variables (quarterly indicators of when a state entered the recession).
Results
Table 1 presents prevalence estimates of study outcomes by each covariate. In this population, 9.6% had serious psychological distress, and 8.9% had a substance use disorder. Among those with serious psychological distress, 44.6% reported receipt of mental health services in the past year. The study population was almost evenly divided between males and females, and most were ages 26–64 and non-Hispanic white. Most individuals had some college education, were married, were employed full-time, and had family incomes ≥200% of FPL. For the most part, prevalence of serious psychological distress, substance use disorders, and mental health service utilization was similar across the quartiles for SCI, serious mortgage delinquency rate, and county unemployment rate. An exception was mental health utilization in counties with the lowest unemployment rates (quartile 1); in those counties, the percentage of individuals who used mental health services was approximately 16 to 19 percentage points higher compared with counties with higher unemployment rates.
Table 2 presents results of multiple regression analyses of associations between the outcomes and macroeconomic and individual-level sociodemographic variables. We found no statistically significant association between the macroeconomic variables and serious psychological distress. On the other hand, several individual-level sociodemographic variables were found to be highly statistically significant predictors of the likelihood of experiencing serious psychological distress. Most notably, being younger, female, and unemployed and living below the poverty line were positively associated with serious psychological distress. Results for substance use disorders were similar; however, being male, rather than female, was positively associated with having a substance use disorder.
A statistically significant negative association was found between use of mental health services and county unemployment rate and serious mortgage delinquency rate. Individuals who resided in counties with higher unemployment rates (quartiles 2–4) were less likely to use mental health services compared with individuals who resided in counties with the lowest unemployment rates (quartile 1). Similarly, individuals who resided in states with higher rates of serious mortgage delinquency (quartiles 2–4) were less likely to use mental health services compared with individuals who resided in states with the lowest rates of serious mortgage delinquency (quartile 1). Among individual-level economic variables, health insurance was found to be statistically significant. Individuals who did not have health insurance were less likely to use mental health services compared with individuals who had health insurance. Age, gender, race, and education level were also found to be statically significant predictors of mental health service utilization. (The prevalence of mental health service utilization is reported as relative risks because, with the model being conditional on individuals’ having experienced serious psychological distress, this prevalence was sufficiently high, and odds ratios may have overestimated the risks [
44].)
Discussion
In this study, we used data from the 2008–2010 NSDUH to examine the relationship between economic conditions and past-year measures of serious psychological distress, substance use disorders, and mental health service utilization. This study is especially relevant to health care policy because we simultaneously examined multiple economic variables at the individual level (employment status and household income as a percentage of FPL) and macroeconomic level (index of states’ overall economic well-being, county-level unemployment, and serious mortgage delinquency rate) to better capture the complex relationship between the economy and behavioral health outcomes.
We found that selected macroeconomic indicators were not significantly associated with the likelihood of serious psychological disorder and substance use disorders. Rather, similar to other studies, this study found that experiencing serious psychological distress or having a substance use disorder was significantly associated with individual-level variables, such as unemployment or living below the poverty level.
On the other hand, macroeconomic variables were found to be important predictors of mental health service utilization, even after the analyses controlled for individual-level economic variables. We found that serious mortgage delinquency rates and county-level unemployment rates were associated with use of mental health services; specifically, poorer economic conditions (represented by higher rates on both variables) were associated with lower utilization of mental health services. Most individual-level economic variables were not statistically significant predictors of mental health service utilization, with the exception of health insurance, which was found to be highly statistically significant.
These results suggest that access to and availability of mental health services among individuals experiencing serious psychological distress may be greater challenges for those who do not have health insurance or who reside in states with higher rates of mortgage foreclosures or counties with higher rates of unemployment. Our findings suggest that availability and affordability are key factors in determining whether individuals experiencing serious psychological distress receive mental health care. Poor economic conditions may affect a community’s ability to provide behavioral health services, and even if services are available, they may be unaffordable for individuals who lack health insurance.
This study had a few limitations. First, NSDUH collects self-reported data, which are subject to recall and reporting bias. Second, NSDUH is a cross-sectional survey and does not measure changes in socioeconomic status over time. Thus this study cannot infer any causal relationships. Third, this study may have underestimated the behavioral health needs of community-dwelling adults, given that the NSDUH does not cover homeless adults who do not live in a shelter.
Conclusions
Despite its limitations, this study contributes to a better understanding of the relationship between economic indicators and key behavioral health outcomes among U.S. adults. Results indicate that among community-dwelling adults, individual socioeconomic characteristics are the main predictors associated with likelihood of experiencing serious psychological distress or having a substance use disorder. However, use of mental health services among individuals experiencing serious psychological distress was strongly associated with macroeconomic conditions as well as with individual-level characteristics.
Economically vulnerable populations may be at greater risk of behavioral health problems, and personal financial hardships (including lack of health insurance coverage) and shrinking federal and state budgets may limit access to mental health services for persons in need. There is reason to hope that the reforms introduced recently by the Affordable Care Act in the provision and financing of health care will be especially helpful to vulnerable individuals. Although shrinking fiscal budgets and poor economic conditions can challenge a state’s or a community’s ability to provide mental health services, limiting such services—especially during periods of poor economic conditions—may have a sizable impact on people’s behavioral health.