People with severe mental illness are substantially affected by vocational and social exclusion (
1), with competitive employment rates typically less than half the rate of employment among people with physical disabilities (
2). Effective vocational rehabilitation approaches are crucial to addressing the low rates of employment among people with a psychiatric disability.
The dominant vocational rehabilitation model continues to be the “train-place” approach in which individuals are provided extended skills training or noncompetitive work experiences prior to seeking competitive employment. Despite the continued use of these approaches, less than 30% of people with severe mental illness in these programs obtain any competitive employment (
3). In contrast, supported employment, which is based on the alternative “place-train” approach, emphasizes a rapid search for competitive jobs followed by the provision of skills training and supports as needed to maintain jobs. Supported employment has a strong evidence base for helping people with severe mental illness obtain and keep competitive jobs (
4,
5).
To date, most of the controlled research on supported employment has focused on work outcomes, such as obtaining competitive employment, hours and weeks worked, and wages earned over follow-up periods of two years or shorter. Limited research has evaluated the effects of vocational programs or work on nonvocational outcomes, such as quality of life and hospitalizations. A recent review found that employment was associated with improvements in self-esteem and with reduced utilization of outpatient psychiatric services but was not consistently related to better outcomes in other areas, including reduced symptoms or hospitalizations, or to improved global well-being or life satisfaction (
6). Although this research suggests that working has some beneficial effects on nonvocational outcomes over a short term (two years), the longer-term impact of sustained employment remains unknown. The beneficial effects of working may be cumulative and grow over time, and, therefore, it is important to understand the impact of sustained work on other life domains beyond the traditional two-year follow-up periods of prior supported employment studies.
Understanding the causal pathways between vocational programs and various outcomes—for instance, employment and quality of life—has relevance from an economic point of view. For example, some research suggests that competitive work reduces the frequency and duration of hospitalizations. On the other hand, reduced frequency and duration of hospitalizations will reduce the overall treatment costs. There is a need for more research examining the interactions between supported employment and nonvocational outcomes. Some evidence suggests that the length of employment has a crucial impact on nonvocational outcomes (
6), underscoring the importance of evaluating the duration of competitive work rather than simply comparing people who worked (or are working) with those who did not work (
7,
8).
The aim of this study was to investigate the effects of sustained competitive employment on hospitalization and quality of life over a five-year follow-up period. Over the past ten years in Europe, partial hospitalization has become a frequently used method for reducing the time in inpatient treatment or as an alternative to inpatient care (
9–
13). Although the average duration of partial hospitalization (nine weeks) is usually longer than that of inpatient treatment (five weeks) (
14–
16), partial hospitalization is a cost-effective alternative that can ensure continuity of treatment and facilitate the ability of clients to reestablish a daily routine before discharge into the community. For this reason, we did not distinguish between receipt of these two types of more intensive treatment, which are both referred to as hospitalizations.
A previous randomized controlled trial (RCT) showed that supported employment resulted in higher rates and longer periods of competitive work over five years among persons with severe and persistent mental illness (
17). This study sought to evaluate how vocational rehabilitation influenced nonvocational outcomes, including whether sustained competitive work partially or fully mediated improvements in these outcomes.
Methods
The study was conducted at the University Hospital of Psychiatry in Bern, Switzerland, between 2002 and 2009. The study protocol was approved by the Canton of Bern Ethics Committee.
Study participants were randomly assigned to either traditional vocational rehabilitation (N=54) or supported employment (N=46). The traditional vocational rehabilitation program functions according to the “first train, then place” approach. Participants received training for six to 12 months in sheltered workshops before the transition into a real-world work environment. The supported employment program was based on the individual placement and support (IPS) model, with good program implementation scores on the IPS Fidelity Scale (66–68 points out of a possible score of 75 during the investigation period) (
18).
To be included in the study, persons were required to be between 18 and 64 years of age, to have a stabilized mental disorder in accordance with
ICD-10 criteria, to be eligible for vocational rehabilitation by Swiss disability insurance, to have expressed an interest in competitive employment, and to not be engaged in competitive work at the time of signing the consent form. Persons were excluded if they exhibited an intellectual disability (IQ <70), a primary substance use disorder, a physical or organic handicap that seriously impeded work, an unwillingness to attend regular outpatient therapy, or a work performance below 50% of normal work performance as determined during the assessment phase or if they had attended the traditional vocational rehabilitation program or the supported employment program for fewer than 15 hours per week (
19). [A CONSORT diagram showing the progress of participants through the stages of the RCT is available as an
online supplement to this article.] Routine assessments were conducted at baseline, one-year follow-up, two-year follow-up, and five-year follow-up.
Measures
Information about the duration of hospital treatment over the five-year follow-up period was collected retrospectively one year, two years, and five years after entering the program.
To assess overall level of functioning, the Global Assessment of Functioning (GAF) (
20) was used. Participants’ quality of life was assessed by the global rating scale of the Wisconsin Quality of Life Index for Mental Health, Self-Administered (W-QLI-MH-s), which encompasses eight semi-independent domains (life satisfaction, occupational activities, psychological well-being, physical health, social relations, economics, activities of daily life, and symptoms). Goal attainment is included as a ninth domain, with its own scoring method. Each domain is assessed by self-report. The global rating scale of the W-QLI-MH-s records how the participants feel about their quality of life during the past four weeks. Lowest quality means things are as bad as they could be. Highest quality means things are the best they could be. Because similar results were found across the various domains, we report only the global rating scale of the W-QLI-MH-s. This multidimensional instrument has been shown to be valid and reliable among persons with severe mental illness (
21).
The Strauss-Carpenter Scale, modified from five to three levels, was used to assess the level of employment as the dependent outcome measure (
22,
23). The three levels distinguished among being unemployed, working in a sheltered workshop, and having competitive employment with a minimum wage. Participants who had been competitively employed for at least 50% of the study duration were defined as “steady workers” (
7). Sustained competitive employment was used as both an outcome and a process variable.
Statistical Analyses
A mediation analysis was conducted to evaluate whether the effects of supported employment on nonvocational outcomes were direct or indirect and if indirect, whether they were mediated by sustained competitive work (
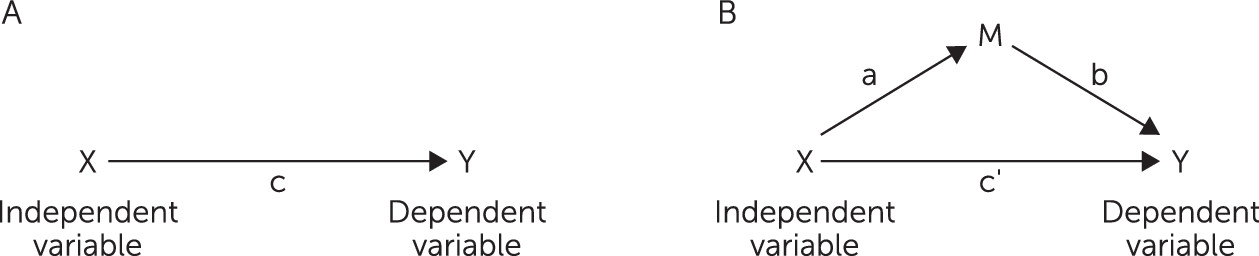
24). A mediation analysis evaluates whether the associations between study condition and an outcome of interest can be better explained by taking into account the effects of treatment on a third variable, which subsequently influences the outcome of interest (
25) (
Figure 1). In this study, the mediation analysis evaluated whether the associations between assignment to study condition (traditional vocational rehabilitation or supported employment) and hospitalization could be better explained by taking into account the effects of treatment on sustained employment. The test of the simple mediation model (model B in
Figure 1) was conducted by performing four steps of regression analyses, with the significance of the coefficients examined at each step. Full mediation is supported if the independent variable, or “X,” (in this case, vocational services) is no longer significant after the analyses have statistically controlled for the mediator, or “M” (in this case, sustained competitive employment). To estimate the explained variance in mediation of hospitalization and quality of life, a coefficient of determination (adjusted r
2 [r
2adj]) is reported. Effect sizes were specified according to Cohen as follows: small, r
2adj>.01; medium, r
2adj>.09; and large, r
2adj>.25 (
26).
A further model calculation was performed by using multiple regression analysis. All data analyses were performed by using JMP Pro 11.1.
Results
Study Participants
Data records for 85 of the 100 patients in the Bernese Job Coach Project study were included in the analysis; data records for 15 patients (15%) were incomplete with regard to the outcome criteria or because the participants were lost over the five-year follow-up period, and four participants died. At the five-year follow-up, an average of 11 years had elapsed since the onset of the patients’ psychiatric disorder. Participants had an average GAF score of 50, indicating moderate to serious impairment in their functioning. The sample is described in detail in
Table 1.
An analysis of variance showed no statistically significant differences between those who dropped out and those who did not drop out by study condition, age, or sex.
Employment Level and Hospitalizations After Five Years
At the five-year follow-up, 32% of participants had achieved sustained competitive employment, with an average duration of employment of 41 months, or nearly 70% of the total follow-up time. Seventy percent of them (19 out of 27) were steady workers, having been competitively employed for at least 50% of the study duration. Forty-nine percent did not achieve competitive employment during the follow-up period (never competitively employed), and 19% achieved competitive employment but lost it and had not regained a job by the five-year follow-up (nonsustained competitive employment) (
Table 1). The participants who did not achieve sustained competitive employment by the five-year-follow-up were either unemployed (N=29) or were working at sheltered workshops (N=29). Those who had obtained competitive jobs during the follow-up period had worked at the jobs briefly before losing them or quitting (
Table 2).
No statistically significant differences were found in days of hospitalization or quality of life between the group with nonsustained competitive employment and the group that never achieved competitive employment. Furthermore, there were no statistically significant differences in time spent working, or income earned from working between the group with nonsustained competitive employment and the group that never achieved competitive employment. Persons who were unemployed did not differ significantly in number of hospitalizations or in quality of life compared with those who were employed in sheltered workshops. For this reason, these two groups were combined into one group of participants with nonsustained competitive employment. This group is compared in the following analyses with the group that achieved sustained competitive employment.
Mediation Analysis
The four steps of mediation analysis were followed to evaluate the effects of vocational program on hospitalizations and quality of life and whether any effects were mediated by sustained competitive employment (
Table 3). First, there was a trend for the vocational program to have a statistically significant effect on hospitalization (p<.1). (This step is shown as path c in model A in
Figure 1). Second, there was a statistically significant relationship between vocational program and sustained competitive employment (path a in model B). Third, there was also a statistically significant relationship between sustained competitive employment and hospitalizations (path b in model B). Fourth, after including the mediator variable (sustained competitive employment) as a covariate in the regression model, the relationship between vocational program and hospitalization became nonsignificant, indicating that the effect of program on hospitalization was fully mediated through the program’s impact on sustained competitive employment (path c′ in model B). The explained variance (r
2adj>.07) indicated a small effect size.
Also shown in
Table 3, the second mediation analysis indicated that the effect of vocational program on quality of life was fully mediated by sustained competitive employment. The explained variance (r
2adj>.09) in this model was 10%, corresponding to a medium effect size.
Discussion
This study investigated whether sustained competitive employment mediated the effects of supported employment versus traditional vocational programs on reduced psychiatric hospitalizations and improved quality of life among persons with severe mental illness who were enrolled in a five-year RCT comparing the two vocational approaches. Participants who were randomly assigned to supported employment were much more likely to achieve sustained competitive employment compared with participants in a traditional vocational program, and they also tended to have fewer hospitalizations and higher quality of life. Furthermore, the mediation analyses indicated that the impact of supported employment on hospitalizations and quality of life was fully mediated by the program’s greater effects on sustained competitive employment. The results are consistent with the interpretation that to the extent that supported employment led to greater reductions in hospitalization and better quality of life than traditional services, these causal effects were mediated by the program’s impact on increased sustained employment (
27,
28).
This mediation analysis provides valuable insight about the role of sustained competitive employment as a potential mechanism underlying the effects of supported employment on nonvocational outcomes (
29,
30). Unemployment is an established psychosocial stressor in the general population (
31). Work is one of the most important recovery goals espoused by people with severe mental illness. Meeting patient-rated unmet needs is associated with higher quality of life (
32). In line with these results, competitive employment has been shown to be associated with improved mental health and quality of life in this population (
33–
35), including among persons receiving supported employment (
36,
37). Bush and others (
38) showed that among individuals with severe mental illness, use of outpatient psychiatric services, in hours, by those who had worked steadily for three years was equal to one-third to one-half of the services used by individuals who had engaged in a minimum amount of work. The number of days hospitalized among those who worked steadily decreased by about three-quarters.
Vocational rehabilitation programs that are based on the IPS model (
39) are much more effective than other vocational programs at helping people with psychiatric disabilities obtain and keep jobs on the open labor market (
40). This study contributes to the body of research on supported employment by documenting its superiority over other vocational models on sustained employment over a five-year follow-up period, the longest of any controlled study of vocational rehabilitation with this population. The mediation analysis further suggests that clinical and quality-of-life benefits may accrue from sustained employment, a finding that is not readily apparent in studies with briefer follow-up periods, for example, one to two years.
Participation in work is an essential part of the recovery process (
41). The biopsychosocial model of mental health and the concept of functional health in psychiatry have helped to sharpen the focus on working as a desirable outcome in the recovery process (
42–
44). Clinical concerns that competitive employment worsens the course of mental illness have been repeatedly refuted (
6). However, this study suggests that sustained work actually has protective effects against rehospitalization, findings that are consistent with some recent RCTs of supported employment (
30,
45,
46). Our results are in line with those of a recent study supporting the notion that better employment status enhances subjective quality of life among patients with schizophrenia (
47).
Study Limitations
This study had a number of limitations. Mental health systems differ across countries, meaning that the nature of services provided for inpatient psychiatric treatment, as well as access to and duration of such treatment, vary by country. Thus caution is required regarding the generalizability of these findings, which are from Switzerland, to other countries and mental health systems. Another limitation was that data on inpatient and partial hospitalization were not collected separately. However, it has been reported that employment has had similar effects on reducing the likelihood of hospitalization in other countries, suggesting that competitive work may have protective effects against hospitalization among people with severe mental illness across a range of mental health systems (
30,
48).
The relatively small sample size, as well as a lack of longitudinal data on symptoms and other dimensions of social participation, such as social contacts, were also limitations of the study. The fact that the quality-of-life outcomes were all self-reported may also be a limitation. On the other hand, subjective quality of life is becoming a standard health outcome measure, especially for people with severe and functional illness (
32,
49,
50). Another limitation, which is inherent to all mediation analyses, was that one or more potentially unmeasured variables other than sustained employment could be responsible for the reduced hospitalization rate and improved quality of life associated with supported employment. One final limitation was that persons with comorbid substance use disorders were excluded. Although some prior research has indicated that supported employment is more effective than alternative vocational programs for persons with co-occurring disorders (
51), the effects on sustained employment in this group remain unexamined.
Future Directions
Additional research is needed to better understand the interactions between sustained competitive employment and mental health–related outcomes. Supported employment has demonstrated its superiority to traditional vocational rehabilitation in improving employment rates, to the extent that employment is defined as working for at least one day. More long-term studies are needed to identify factors that are associated with maintaining sustained competitive employment among participants in supported employment programs—even after acute mental illness or job loss.
In this study, only 19 of the 38 (50%) IPS participants reached sustained employment, an outcome that leaves considerable room for supported employment services to improve.
Competitive employment and education are common treatment goals among people with severe mental illness, in particular people with early psychosis, but individuals often struggle with ambivalence in taking concrete action to achieve these goals (
52–
54). Coping with reluctance to pursue goals—in particular, fear of failure, social anxiety, and stigmatization—is not a key element of supported employment. Motivational interviewing is a collaborative, person‐centered form of guiding to elicit and strengthen motivation for change, and it focuses on exploring and resolving ambivalence. Only a few studies have investigated the implementation of motivational interviewing in IPS (
54–
56), and the effects of this approach in supported employment programs are understudied to date. Another promising approach to improve the effectiveness of supported employment is cognitive remediation (
57,
58).
A recently published research report by the Organization for Economic Cooperation and Development (OECD) addresses practical issues related to employment and mental health. The report postulates that “Only treatment and employment support combined improve work outcomes” (
59). This principle could also have been derived from the results of this study. In other words, scientific evidence is required to promote practical implementation and application in service planning, including evidence related to early vocational interventions, the combination of clinical treatment and medical and vocational rehabilitation, and long-term job support. In the context of long hospitalizations, it could be useful to install psychosocial rehabilitation programs to enhance functional health as an alternative to long-term hospital treatment (
60). Another relevant issue is the implementation of nationwide supported employment services to improve mental health, recovery, and quality of life among people with severe and persistent mental illness (
61). Finally, our results indicate that mediation analysis is a promising methodological approach to illustrate the mechanisms through which vocational programs and nonvocational outcomes are related.
Conclusions
Sustained competitive employment significantly reduced the need for psychiatric hospitalization over the long term. People with severe and persistent mental illness who were sustainably competitively employed assessed their quality of life as significantly better compared with those who did not maintain competitive employment. Supported employment significantly increased competitive employment and indirectly promoted improved mental health and quality of life by improving the likelihood of achieving sustained employment.