About 6.7% of children and adolescents (hereafter referred to as children) are diagnosed as having attention-deficit hyperactivity disorder (ADHD), and prevalence estimates have risen steadily over the years (
1). ADHD significantly affects academic, fine-motor, and socioadaptive skills, leading to emotional, behavioral, and learning problems among children. Thus it is crucial to appropriately diagnose, treat, and manage ADHD in this population.
During the past decade, primary care settings have become the first point of contact and the treatment site of choice for all children with mental disorders (
2,
3). Analysis of data from a nationally representative sample found that in 2012, one-third (34.8%) of children (ages two to 21) receiving outpatient care for mental health conditions saw primary care physicians (PCPs) only, and nearly a quarter (23.8%) saw both PCPs and specialists (
2). Consistent with the general trend in mental health care, the vast majority of patients with ADHD are now first identified and treated in the primary care setting. Data from physician office visits show that 64% to 75% of ADHD prescriptions written between 2000 and 2010 were written by PCPs (
4).
Despite the importance of PCPs in current ADHD care, they face barriers, such as lack of training, time constraints, and low reimbursement rates, which have led to concerns about the quality of care provided. Patients and caregivers are often concerned about short visits and difficulties associated with access to care, which have resulted in their perception of PCPs as not being as competent as child psychiatrists (
5–
9).
In contrast to PCPs, child psychiatrists are regarded as the group with extensive training in and knowledge of mental health care. A physician survey showed that 70% of child psychiatrists consider pediatricians to lack appropriate training in identifying mental problems among children (
5). However, with the severe shortage of mental health specialists in most counties in the United States, it is expected that PCPs will remain the mainstay for care of ADHD.
To improve the quality of care for children with ADHD, it is necessary to understand the differences between the practice of PCPs and child psychiatrists. However, little relevant information exists in the literature. Therefore, we compared the current practice of diagnosis, treatment, and monitoring of children with ADHD first identified by PCPs versus child psychiatrists.
Methods
Data Source
This study was conducted using data from the 1995–2010 General Electric (GE) Centricity electronic medical record (EMR) research database. GE Centricity EMR has 35,000 physician users from 2,500 practices throughout the United States, representing about 15% of the physicians in the country (
10). The database includes longitudinal ambulatory health records for around ten million individuals across 40 states. The data are representative of the U.S. population based on gender, age, most diagnoses, and geographic location (
11,
12). GE EMR data cover both the private and the public sectors and include information about patients visiting the practices that use the GE EMR system, regardless of the insurance type of the patient and the specialty of the physician.
To examine the validity of the data set, Crawford and colleagues (
13) compared the GE Centricity EMR data with data from the National Ambulatory Medical Care Survey (NAMCS) on the prevalence of major conditions in the United States and found that GE-EMR data were more sensitive than NAMCS data in capturing diagnoses, especially chronic diagnoses.
Sample Population
Individuals were eligible for inclusion in this study if they were ≤18 years of age, had ever been diagnosed as having ADHD (ICD-9-CM code 314.XX), and had received at least one prescription for ADHD medication (stimulants and atomoxetine). About 20% of patients had only one physician visit and then disappeared from the GE EMR system; these patients were excluded from the sample. They may have moved, changed physicians, or simply stopped using health services.
Study Design
This study used a retrospective cohort design in which every ADHD patient was followed for one year after the index visit. The index visit was defined as the visit during which the patient was diagnosed as having ADHD or received a prescription for ADHD medication after a minimum of 180 days free of both ADHD diagnosis and psychotropic prescription. The washout period was used to increase the likelihood that the ADHD cases identified were new. The study groups (PCPs or child psychiatrists) were defined on the basis of the type of physician who made the index ADHD diagnosis. In the sample, 21.6% of patients were given the ADHD diagnosis by a physician whose specialty was missing from the database; however, instead of excluding these patients, we created a group for unknown specialty. This group could reflect the involvement of trainee physicians or part-time physicians in the care of children with ADHD.
Outcome Measures
Comorbid psychiatric disorders.
Comorbid psychiatric disorders noted at the index visit were identified by using ICD-9-CM codes for depression, bipolar disorder, oppositional or conduct disorder, anxiety disorder, substance use disorder, or learning disability.
Time to first ADHD prescription.
How soon children were prescribed ADHD medication after their index ADHD diagnosis was examined. Treatment could either be immediate (medication was prescribed on the day of ADHD diagnosis) or delayed (medication was prescribed sometime after ADHD diagnosis).
Follow-up care.
Follow-up visits were defined as per the
Follow-Up Care for Children Prescribed ADHD Medication, a publication of the National Committee for Quality Assurance (NCQA) (
14). Follow-up visits were measured as the percentage of individuals on ADHD medication who had one follow-up visit during the 30 days (initiation phase) after the initiation of ADHD medication and the percentage who remained on the medication for at least 210 days and who, in addition to the visit in the initiation phase, had at least two follow-up visits within 270 days (continuation and maintenance phase) after the initiation phase.
Use of psychotropic medication monotherapy and polytherapy.
The proportion of children with ADHD who were prescribed ADHD medication and the proportion prescribed other psychotropic prescriptions in addition to ADHD medication were estimated by physician type.
Collaborative care between PCPs and child psychiatrists.
Children given an ADHD diagnosis by a PCP were followed to observe whether they were ever referred to a child psychiatrist and whether their referral was ever completed (that is, whether they visited a child psychiatrist).
Statistical Analysis
Multivariate logistic regression analysis was conducted to further clarify the association between physician type and each of the three outcome measures, including identification of comorbid psychiatric disorders (defined as comorbidity diagnosed or no comorbidity), time to treatment (defined as either immediate or delayed), and use of psychotropic polytherapy (defined as received or not received).
The primary independent variable was the type of physician who made the ADHD diagnosis at the index visit. The covariates included were patients’ demographic characteristics, including age, race-ethnicity, gender, geographic region (Midwest, Northeast, South, or West), and type of insurance (commercial insurance, Medicaid, self-pay, or unknown); psychosocial and behavioral interventions prior to prescription of ADHD medication; and any medications prescribed prior to the prescription of ADHD medication. For the analysis of psychotropic polytherapy, we also controlled for comorbid psychiatric disorders to clarify whether child psychiatrists were prescribing more intensive pharmacotherapy than PCPs solely because of the comorbid conditions that they identified.
All the analyses were carried out with Statistical Analysis Software 9.3. The University of Houston Institutional Review Board approved the study.
Results
Demographic Characteristics
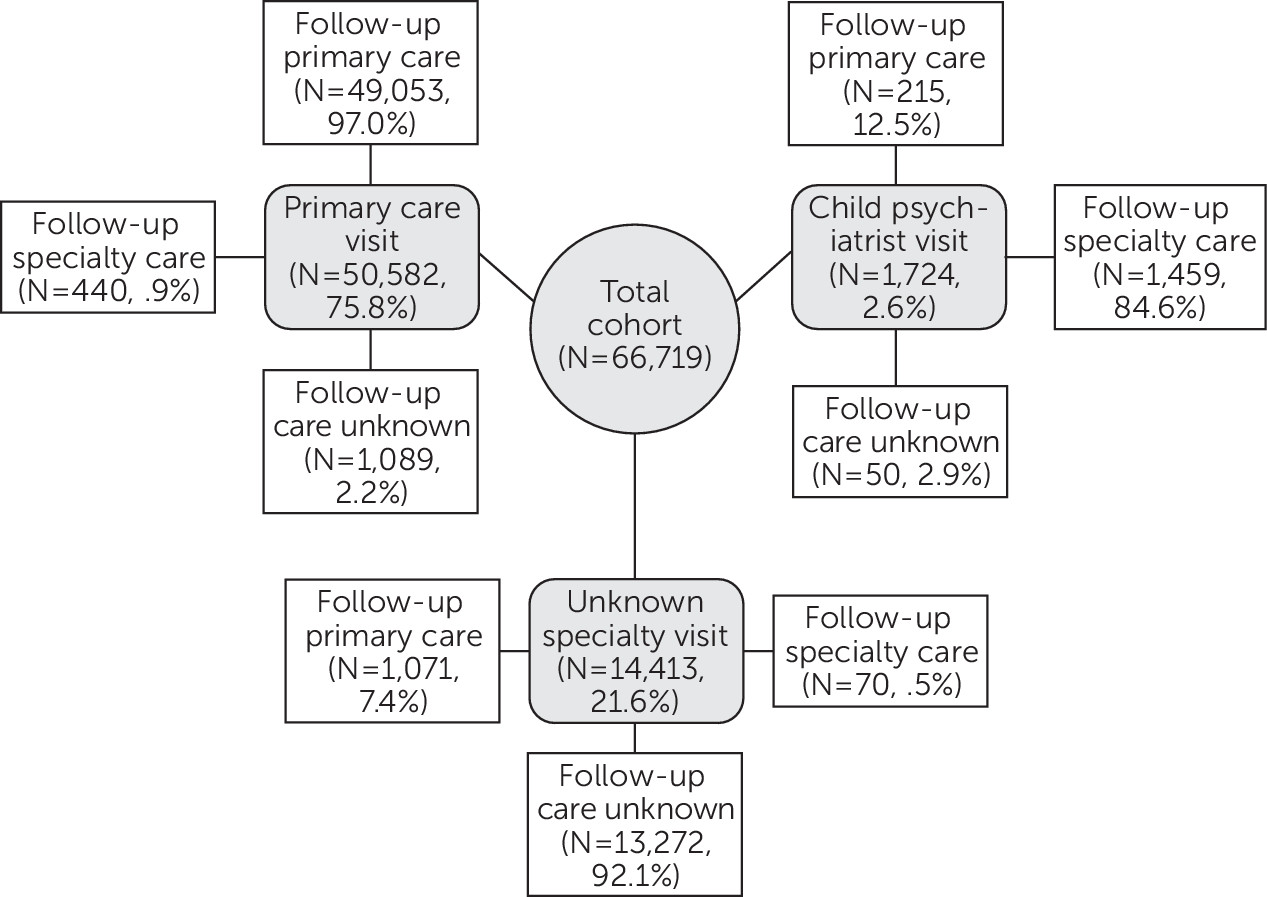
We identified 3,920,793 children in the GE Centricity EMR database treated between 1995 and 2010, of which about 5.0% (N=197,075) were ever diagnosed as having ADHD. Among those with an ADHD diagnosis, 51.5% (N=101,516) had been prescribed ADHD medication (either stimulants or atomoxetine). Among these treated patients, 19.4% (N=19,658) did not have a documented activity after the index prescription. Among patients with no documented follow-up, 74.3% (N=14,606) received a prescription for ADHD medication from a PCP, 3.1% (N=609) from a child psychiatrist, and the rest (22.6%, N=4,443) from a provider with an unknown specialty. The distribution of prescribing providers was similar to the distribution for individuals with documented follow-up activities. Individuals without a documented follow-up activity and those without sufficient data in the GE EMR system to capture the care history 180 days before the first ADHD diagnosis or prescription (15%, N=15,139) were excluded. Thus the final cohort consisted of 66,719 children with ADHD prescribed ADHD medication. [A flowchart in an online supplement to this article provides details about sample selection.] Of the 66,719 children, 75.8% (N=50,582) were given the ADHD diagnosis by PCPs, 2.6% (N=1,724) by child psychiatrists, and 21.6% by physicians whose specialty was unknown.
Comorbid Psychiatric Disorders
The most common comorbid conditions diagnosed along with ADHD at the index visit were conduct or oppositional disorder (2.4%) and depression (2.3%). Compared with patients diagnosed with ADHD by PCPs, those diagnosed by child psychiatrists had higher rates of comorbid depression (3.5% versus 2.2%, p=.002), conduct or oppositional disorder (4.4% versus 2.5%, p<.001), anxiety disorder (3.7% versus 1.8%, p<.001), and learning disability (2.1% versus 1.4%, p=.027) (
Table 1).
Time to Initial ADHD Medication Prescription
Of the 66,719 patients, 59.0% (N=39,343) were prescribed ADHD medication at the visit when ADHD was diagnosed. Among the 41.0% (N=27,376) who received delayed medication treatment, 34.7% (N=9,491) received medication treatment within three months, 17.3% (N=4,740) within six months, 11.8% (N=3,225) within nine months, and 9.4% (N=2,576) within 12 months; the rest (26.8%, N=7,344) received medication treatment 12 months after the initial ADHD diagnosis. The median time to initial ADHD medication prescription was 37 days. Among the 50,582 children diagnosed by a PCP, 59% (N=29,889) were given a prescription for ADHD medication immediately, compared with 43% (N=746) of the 1,724 children who were diagnosed by a child psychiatrist (p<.001).
Follow-Up Care
The children in the study cohort had a mean of 6.57 follow-up visits within ten months of initial medication prescription (the follow-up duration was defined on the basis of NCQA HEDIS criteria [
15]). Children given an ADHD diagnosis by a PCP had a slightly lower mean number of visits compared with those given a diagnosis by a child psychiatrist (6.56 versus 7.26, p<.001); the median number of follow-up visits was six for both groups (
Table 1). Of the 66,719 children, 38.1% (N=25,390) had a follow-up visit within the initiation phase, and 33.7% (N=22,476) met both the initiation phase and the continuation-maintenance phase criteria of the HEDIS follow-up care measure for children prescribed ADHD medication. Among these children, the proportion meeting the criteria was slightly higher among those diagnosed by a child psychiatrist (N=654 of 1,724, 37.9%) compared with those diagnosed by a PCP (N=16,797 of 50,582, 33.2%) (p=.013).
Collaborative Care Between PCPs and Specialists
Of the 64,995 children diagnosed by a PCP or by a physician with an unknown specialty, 6.4% (N=4,180) were ever referred to a mental health specialist, and 32.4% (N=1,354) of these patients were documented as having a completed referral (the patient completed a visit with the specialist); referrals for the other patients were recorded as “on hold” or “under process” (the referral was either incomplete or the system had lost track of the referral). Moreover, the referral from a PCP to a mental health specialist did not usually happen immediately after the case identification. As presented in
Figure 1, only a small proportion of children diagnosed by PCP (.9%) or by unknown specialty (.5%) had their first follow-up visit (visit immediately after the index visit) with a child psychiatrist, whereas among the 1,724 patients (2.6%) diagnosed by a child psychiatrist, 84.6% had the first follow-up visit with a specialist and 12.5% had the first follow-up visit with a PCP.
Monotherapy and Polytherapy
Of the 66,719 children, the percentage prescribed stimulants ranged from 86.9% to 90.1% (mean 89.5%) depending on the provider type; 9.2% to 12.1% (mean 9.8%) were prescribed atomoxetine and .7% to 1% (mean .7%) were prescribed a combination of the two (
Table 1).
Among the 66,719 children, the most commonly prescribed non-ADHD psychotropic medications were antidepressants (5.9%) followed by second-generation antipsychotics (2.4%). Overall, a greater proportion of children given an ADHD diagnosis by a child psychiatrist received non-ADHD psychotropic medications, compared with those given an ADHD diagnosis by a PCP (antidepressants, 15.3% versus 5.4%; second-generation antipsychotics, 8.8% versus 2.4%, and mood stabilizers, 3.7% versus 1.0%; p<.001) (
Table 1).
Unknown Physician Specialty
Of the 66,719 children, 21.6% (N=14,413) were given an ADHD diagnosis by a physician whose specialty was not reported in the database. Compared with patients diagnosed by a PCP, these patients had similar rates of receiving an immediate prescription for ADHD medication (PCPs, 59% [N=29,889]; unknown specialty, 60% [N=8,628]) and similar rates of being prescribed stimulants (PCPs, 89.4% [N=45,241]; unknown specialty, 90.1% [N=12,988]) and atomoxetine (PCPs, 9.9% [N=4,993]; unknown specialty, 9.2% [N=1,331]). However, patients given an ADHD diagnosis by a physician of unknown specialty had longer times to first follow-up visit, compared with those diagnosed by PCPs (54.53 versus 49.29 days) (
Table 1).
Multivariate Analysis
After control for all demographic and baseline characteristics, multivariate analysis indicated that at the index visit child psychiatrists were more likely than PCPs to identify psychiatric disorders comorbid with ADHD (odds ratio [OR]=1.20) (
Table 2). Child psychiatrists were much less likely than PCPs to prescribe ADHD medication at the index visit (OR=.53). Use of non-ADHD psychotropic medications was positively associated with having certain comorbid psychiatric disorders (for example, bipolar disorder) and with increasing patient age. However, even after controlling for these predictors, the analysis indicated that child psychiatrists were more likely than PCPs to prescribe a non-ADHD medication in addition to medication for ADHD (OR=1.52).
We also conducted a subanalysis with data for the elementary school–age children in our sample, which represented a much newer (incident cases) cohort with fewer comorbid conditions. The findings showed trends similar to those in the main analysis (
Table 3).
Discussion
Consistent with previous research (
15,
16), this analysis of data from the GE Centricity EMR database found that 5.0% of children had ever been diagnosed as having ADHD and that half of these patients (51.5%) were prescribed ADHD medications. Of the 66,719 children with ADHD prescribed ADHD medication in the study cohort, 75.8% were given a diagnosis by a PCP, 2.6% by a child psychiatrist, and 21.6% by a physician whose specialty was unknown. The small proportion of children diagnosed by child psychiatrists might be attributable to the fact that the GE EMR database is mainly used by PCPs—roughly two-thirds of all users are PCPs. However, because of the large sample size, the absolute number of patients diagnosed by child psychiatrists was large enough (N=1,724) to permit analyses of child psychiatrists’ practice patterns.
One of the most prominent differences in care delivered by child psychiatrists was that they were more likely than PCPs to identify comorbid psychiatric conditions. Child psychiatrists may be better trained than PCPs in identifying conditions comorbid with ADHD. A previous study showed that PCPs failed to recognize 30% to 50% of depressed patients who had a comorbid mental illness (
17). Correct diagnosis is the first and most important step in disease management. Given the increasingly important role of PCPs as gatekeepers for ADHD identification and treatment among children, it is critical to develop collaborative approaches that involve PCPs and specialists in the diagnostic process. However, our findings suggest that current collaboration between PCPs and child psychiatrists in ADHD care is limited. Of the patients diagnosed with ADHD by PCPs, only 6.3% were ever referred to mental health specialists, and only 32.4% of those referred were documented as having a completed referral. To improve access, collaboration, and coordination in pediatric mental health care, it is necessary to address the administrative and financial barriers that PCPs and mental health professionals face in providing behavioral health services to children and adolescents (
18).
Another important finding was that child psychiatrists were less likely than PCPs to initiate treatment immediately following the diagnosis of ADHD. However, once the treatment started, they were more likely than PCPs to prescribe additional psychotropic medications. Even after the analysis controlled for the difference in identified comorbid conditions, psychiatrists were still more likely than PCPs to prescribe other psychotropic medications (OR=1.52). These seemingly paradoxical differences in practice between PCPs and child psychiatrists reflect the ongoing challenges faced by PCPs in managing pediatric behavioral disorders, including ADHD, and the increasingly important role of pharmacotherapy in disease management. On average, a PCP has a patient panel of 1,500 to 2,000 patients and sees 20 to 30 patients per day. PCPs likely do not have enough time and training to conduct a comprehensive evaluation of patients’ mental health status. However, patients typically expect some action to be taken immediately and may pressure PCPs to write a prescription (
19). The delayed treatment observed among patients cared for by child psychiatrists may imply that child psychiatrists are more effective than PCPs in persuading parents to go through a period of watchful waiting before the initiation of pharmacotherapy, which allows psychiatrists to ascertain the duration and severity of the behavioral symptoms. However, once treatment is initiated, many psychiatrists place a greater emphasis on specific symptom reduction than on the disorder itself, which may lead to lack of concern about the number of medications prescribed (
20–
22).
Regarding ADHD follow-up care, only 38.1% of the patients in our study had a follow-up visit in the initiation phase and 33.7% met both the initiation phase and the continuation-maintenance phase criteria of the HEDIS follow-up care measure for children prescribed ADHD medications. Patients diagnosed by PCPs had a slightly lower number of follow-up visits and a shorter time to the first follow-up visit compared with patients diagnosed by child psychiatrists. Systematic titration of stimulant medications is necessary because of the marked individual variability among children in the dose-response relationship. Upward titration every one to three weeks is recommended, and the parent and teacher ratings of symptoms and side effects should be obtained after the child has been observed on a particular dose for at least one week. On the basis of these recommendations, the NCQA developed the ADHD quality-of-care HEDIS measures. Meeting the HEDIS performance measures is expected to have a positive impact on medication adherence and on monitoring of side effects, which are a common reason for medication discontinuation early in treatment. The low rates of follow-up visits and nonconcordance with the HEDIS criteria observed in our study, although consistent with national rates reported by NCQA in 2014 (
14), suggest a strong need for policy change to ensure that quality-of-care standards are met (
23,
24).
The study had limitations. First, the data used did not reflect patient visits to care practitioners outside the GE Centricity network. Complete treatment and care coordination data may not have been captured. Second, because the children were not randomly assigned to PCPs or psychiatrists, the comparison between the two types of providers was subject to selection bias on unobservable factors, such as severity. To minimize the impact of unobserved confounders, we restricted the cohort to patients with newly diagnosed ADHD first identified by a PCP or by a specialist, and we also conducted a subanalysis with data for the elementary school–age children.
Conclusions
This study found variations between primary care physicians and child psychiatrists in the treatment of children with ADHD. Additional studies are needed to understand the clinical consequences of these differences and the implications for care coordination across provider specialties.