African Americans living in the rural South are more likely than other rural Americans to live in persistent poverty (
1) (with poverty rates of at least 20% since 1980) (
2) and to experience poor educational attainment, fewer economic opportunities, racism, and discrimination (
3–
5). Chronic exposure to such stressors can increase the likelihood of experiencing stress-related psychopathology, such as depression (
6–
10). A recent study found that up to 30% of rural African Americans sampled reported clinically significant depressive symptoms (
11), compared with estimates of 10%−19% in other community-based studies of African Americans (
12). Research on racial disparities in outcomes has shown that rural African Americans are more likely than their white counterparts to experience a higher burden of disability related to mental illness, such as an increased risk of hospitalization and greater impairment in occupational and social functioning (
13,
14). Taken together, these data suggest that rural African Americans may experience greater stress and an increased risk of mental illness, compared with their Caucasian counterparts (
10,
15–
17).
Rural African Americans are less likely to receive formal mental health treatment than members of other racial and ethnic groups living in the rural South (
15). Numerous structural barriers to timely and adequate mental health care for rural African Americans exist, including lack of insurance, fewer available services, services of substandard quality, and greater travel distances (
15,
16,
18–
20). Cultural barriers, such as mistrust and fear of treatment, may prove equally as obstructive, placing rural African Americans at risk of experiencing significant levels of functional impairment resulting from unmet psychiatric need (
19,
21,
22).
Most efforts to improve mental health care in rural areas focus on improving access to care (telemedicine) or improving quality of care (collaborative mental health services in primary care) (
23–
25). However, these approaches may not be as beneficial to those who may be unlikely to seek formal health care. Therefore, this study aimed to understand mental health, mental illness, and mental health treatment from the perspective of rural African-American residents and other stakeholders in order to develop culturally acceptable treatment approaches.
Methods
Community Partnership
This study resulted from a partnership between the University of Arkansas for Medical Sciences (UAMS) and Tri-County Rural Health Network (TCHRN). The UAMS team consisted of a multidisciplinary group of faculty (psychiatrist, clinical psychologist, doctoral-level nurse, medical sociologist, and medical anthropologist). TCHRN runs a successful program of community health workers (called community connectors) linking persons with chronic general medical illnesses to resources for home- and community-based health services. A ten-member Community Advisory Board (CAB) provided oversight of the project. The CAB consisted of community leaders, college students, mental health providers, community health workers, and persons living with mental illness.
Setting
This study was conducted in Jefferson County, located in the Arkansas Delta. African Americans living in the Arkansas Delta experience negative health outcomes and marked health disparities (
26). The mean income of African Americans in Jefferson County is $36,638, compared with the mean income of $41,983 among Caucasians. In Jefferson County, African-American households are more likely to be headed by a single mother, and 36% of African-American families with children under age 18 live below the poverty level. Jefferson County has a relatively strong health care infrastructure, including a mental health clinic and a federally qualified community health clinic.
Recruitment
Four key stakeholder groups relevant to rural African-American mental health were identified: primary care providers, faith community representatives, college students and administrators, and individuals living with mental illness. In choosing our stakeholder groups, we considered groups identified in the literature as being important to the African-American community in general (clergy), important in this particular location (colleges), important in the health care delivery system (providers), and important for the lived experience of mental illness (individuals with mental illness). We utilized a snowball recruitment technique in which we identified a key informant or a person connected to the stakeholder group, who then connected us with potential participants or suggested ways (such as flyers) to reach potential participants.
Interview Procedure and Protocol
Prior to developing the interview guide, the research team, community partners, and CAB worked to determine culturally acceptable language for discussing mental health. Given the stigma associated with the word “mental,” the CAB suggested that we use the term “emotional wellness.” The CAB defined emotional wellness as “a state of health in which an individual can cope with everyday stress and life circumstances.” Following consensus on terms to be used, the research team developed a semistructured interview guide. This interview guide included probes to encourage discussion about perceptions of emotional wellness and mental illness, current efforts to address mental illness, and preferences for both addressing mental illness and promoting emotional wellness. [The focus group guide is available as an online supplement to this article.]
We completed two focus groups with health care providers (N=16), one with clergy and parishioners (N=6), one with persons living with mental illness (N=10), and one with college students and administrators (N=9). After noting how the inclusion of college administrators stifled the voices of the students, we held an additional focus group with only college students (N=9). All focus groups were conducted between March and May 2013. Each group lasted approximately 90 minutes and was moderated by a member of the academic research team. Focus groups were held in local settings (local church, college office space, and medical clinic conference rooms). Participants received $50 to $100 compensation (depending on community or provider status) for participating in the study. Each focus group was audio recorded, and the recordings were transcribed.
Data Analysis
Principles of grounded theory, including theme identification, constant comparison, and model building grounded in narrative text, were used to analyze the data (
27). The transcribed content of each focus group was imported into MAXQDA, a qualitative data analysis program (
28). MAXQDA facilitates organizing, managing, and analyzing text-based data. Analysts developed codes based on the interview guide and used MAXQDA to apply codes and to tag related text segments. Analysts then used open coding to identify emergent themes. A codebook, including thematic code definitions and exemplar quotes, was developed, and analysts independently applied the coding schema to the same text to assess intercoder agreement (
29). The qualitative analysts reconciled disagreement and revised the codes until an intercoder reliability of .80 was reached (
30). Analysts then applied the codes to all transcripts. Constant comparison was used to compare and contrast themes within and across focus groups. Themes were reported to the CAB, and CAB members assisted with data interpretation.
Results
As shown in
Table 1, most participants were female (58%), African American (88%), and currently employed (63%). Thirty-three percent were married, and 33% had completed some college. A total of 22 (47%) were either currently in mental health treatment themselves or knew of someone who had received formal mental health treatment.
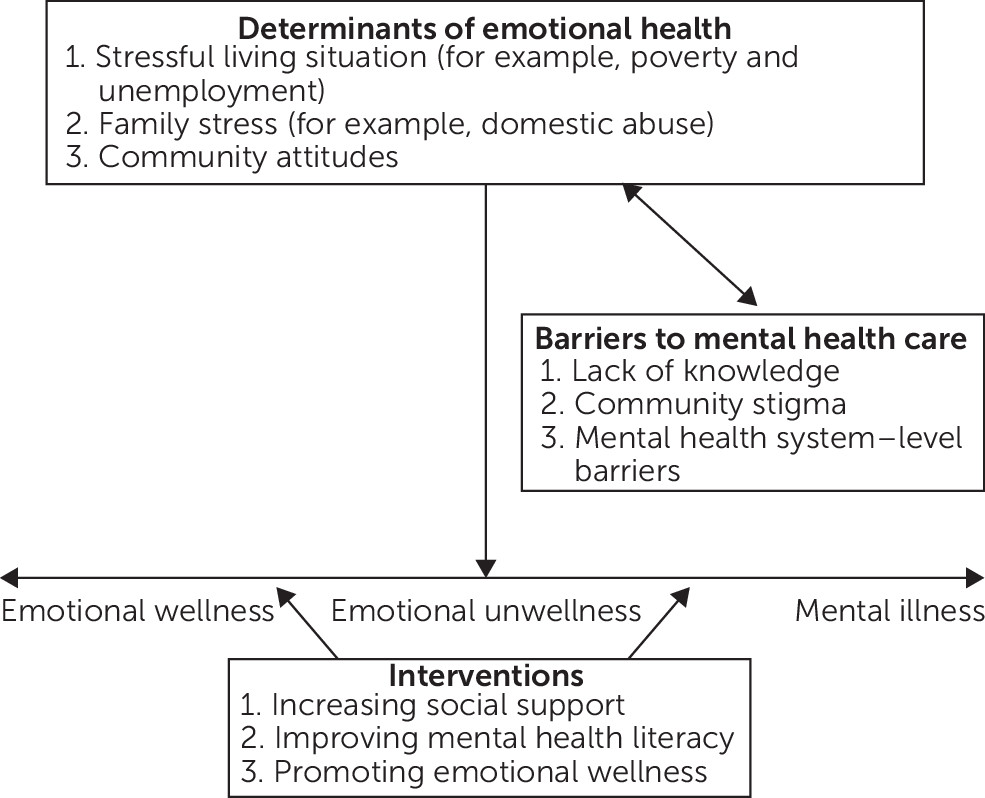
Analysts generated a conceptual model that was grounded in the transcribed recordings and that provided a comprehensive overview of the relationships between themes (
27,
31).
Figure 1 delineates how determinants of emotional health influenced participants’ conceptualization of mental health and their perceptions of barriers to the use of mental health services. Such barriers often serve to reinforce determinants of emotional wellness, such as community-held beliefs. Participants identified community-level strategies to address mental illness and promote emotional wellness in rural African-American communities. Below we explicate the relationships delineated in
Figure 1 by using participants’ narratives.
What Is Emotional Wellness?
When defining mental health, participants tended to think of a spectrum running from emotional wellness (ability to cope with stress) to emotional unwellness (emotional distress)—and at the far end, a diagnosable psychiatric illness.
Emotional wellness.
Participants defined emotional wellness as the “positive management of emotions” when faced with stressful situations. Participants also identified self-esteem as an important characteristic of emotional wellness. One participant stated, “If I’m emotionally well, I feel good about myself. I feel good about where I’m at, and I feel good about the way I work—and I have a real good stepping stone.” Participants identified factors that promote emotional wellness; they identified having social support (that is, having someone available to listen and offer help or advice) and positive outlets (that is, recreational activities or hobbies) as being particularly important for emotional wellness.
Emotional unwellness.
Probing questions encouraged discussion about perceptions only of emotional wellness and mental illness. However, participants spontaneously introduced another term: emotional unwellness. Participants considered emotional unwellness as being “distressed” or “emotionally strained,” with symptoms not yet as severe as those of mental illness. Rather, emotional unwellness was seen as a risk factor for the development of mental illness.
Mental illness.
Most participants perceived mental illness as a serious issue characterized by being “unkempt” or “isolated.” Participants mentioned clinical diagnoses, such as depression and schizophrenia; however, when they were asked to describe mental illness, most—with the exception of providers—were unable to identify the signs and symptoms associated with these labels.
Determinants of Emotional Wellness
Stressful living environment.
Participants readily acknowledged that living in poverty leads to a host of additional stressors, such as unstable housing, inability to pay for utilities, and food insecurity, that negatively affect emotional health. One participant stated, “You see a lot of people now that are homeless or either one check away from being homeless. And that increases the stress level, which increases anxiety levels, which may lead to other forms of mental health issues, because you just think you’re on the verge of—you don’t know whether or not you’re going to have a roof over your head tomorrow. Or you’re working but you know that check is not stretching the way it needs to stretch week to week.”
Family stress.
In addition to the impact of community stressors, participants noted that adverse experiences within the family, such as abuse and neglect, also affect emotional health. One participant stated, “Well, if you got a husband that’s got mental health issues and he may be drinking and in turn he may get abusive with his wife, that may cause her to have issues and it’s just a cycle. Maybe cause her to have depression and everything.”
Community attitudes: feelings of hopelessness.
Many participants described how the stress of living in poverty leads to a sense of hopelessness that can have a negative impact on emotional health. One participant stated, “I think the mentality in our community is very bad. I think we've gotten away—because things are bad and things are worse in areas of poverty—our mentality and our morale has dropped.”
Barriers to Mental Health Treatment
Participants identified mental health treatment as an important and necessary option for addressing mental illness. Untreated mental illness was thought to be associated with increased isolation, criminal activity, and self-medication with drugs and alcohol. Despite the importance of treating mental illness, many participants indicated that significant barriers impeded access to and use of mental health services.
Limited knowledge about mental health.
Participants indicated that there is a general lack of awareness about mental illness. Participants felt that most people don’t know what mental illness looks like, how to recognize it, or how to identify warning signs of crises. For instance, one participant said, “Yeah, it’s pretty easy to recognize you’re having a heart attack if your chest hurts and you’re short of breath, but if you’ve got some mental illness, like I said, they’re a little tricky. It’s not like you have these set number of symptoms.”
Community stigma.
Stigma remains one of the most important barriers to formal treatment and informal help seeking within this community. One participant stated, “It’s sad to say that in the African-American community that we act as if it [mental illness] doesn’t exist, but it does.” Many participants discussed reluctance to seek help for mental health issues because of concerns about a lack of anonymity and fears of being labeled crazy or dangerous. In fact, some participants described a reluctance to discuss mental illness with medical providers. “If you’re a diabetic you may go to your physician and say, ‘Well, diabetes runs in my family,’ but if you have a mental illness, ‘Well, mental illness runs in my . . .’—you’re not likely to say that to the doctor.”
Mental health system–level barriers.
Most participants perceived that services are available. However, they agreed that the mental health care system is more complicated than the general medical care system. Participants identified several improvements that could be made to the service system, such as better mental health screening in primary care, more mental health care provided in primary care, and better quality mental health specialty care.
Addressing Mental Health Needs and Promoting Emotional Wellness
Participants identified three broad types of interventions in addressing mental health needs: providing social support, improving mental health literacy, and promoting emotional wellness.
Social support.
Participants highlighted the importance of providing emotional support (that is, nonjudgmental listening). Specifically, participants suggested implementing mentorship programs and support groups for family members of those living with mental illness as the primary ways to increase social support in rural African-American communities.
Mental health literacy.
Participants identified a lack of understanding of the symptoms of mental illness and a lack of awareness of treatment options as major barriers to help seeking. Many suggested that increasing awareness through education may be an important first step. Education efforts could target everyone in the community, but they could specifically target family members, primary care physicians, and ministers. One participant said, “I also think educating the community on just being mentally healthy, just educating and letting them know it’s not a weakness but it’s about a chemical imbalance and some things you can’t help. Try to help them with coping skills and educate them.”
Promoting emotional wellness.
Participants indicated that it may be helpful to implement interventions aimed at promoting emotional wellness and preventing mental illness. Programs could include providing recreational outlets for individuals, such as community centers offering daily activities. Many also mentioned that updating or cleaning up the parks might be a good start to promoting emotional wellness. Participants also discussed the importance of helping individuals cope with common stressors, such as managing finances, preparing résumés for job searching, and learning to manage other chronic health issues. These efforts may improve an individual’s ability to cope and thereby improve his or her overall emotional wellness. Spirituality, including an intrinsic belief in God and prayer, was thought to be beneficial to maintaining emotional wellness because it gives individuals a sense of hope and optimism in the face of stress. Although participants discussed spirituality as important, they also noted that some aspects of organized religion may not always be useful in promoting emotional wellness and in some cases may even be detrimental. A participant stated, “You have to be careful . . . so we [don’t] look at mental illnesses as demons.”
Discussion
In this study, rural African Americans correctly recognized how social inequities, including racism, unemployment, and poverty, increase the risk of experiencing mental illness. Implementing interventions that promote mental health and that build individuals’ abilities to cope with stressful situations (that is, teaching strategies for coping with racism and poverty) (
32) in communities riddled with persistent poverty may be a first step to mediating the negative impacts of poverty-related stress on emotional health. Attempts to improve emotional wellness in this population may be more effective if emotional unwellness is conceptualized as a normal reaction to living under inequitable conditions. Therefore, interventions using sociocultural conceptualizations of mental health that emphasize the role that stress related to one’s minority status plays in the development of mental illness may be more culturally acceptable.
The most powerful barriers to seeking help cited by participants were mental health stigma and low mental health literacy. The ability to identify symptoms of mental illness is the first step to seeking timely and appropriate help (
33), and a lack of awareness has serious implications for service use. Except in the most extreme cases, it is challenging for community members to recognize that treatment is needed. Even after a need is recognized, stigma may continue to impede treatment seeking. Participants’ recommendations to improve treatment use, such as providing services in nonclinical settings such as community centers, were in many ways shaped by stigma and concerns about preserving anonymity. Providing care in community settings also offers an opportunity to implement peer-led mental health interventions. Peer-led interventions for depression and trauma have been found to be effective (
34,
35) and culturally acceptable. Peer-led interventions may also provide opportunities to increase social support, a strategy that was suggested by participants to improve emotional wellness.
Participants also suggested educating the public about mental illness. Mental health education programs, such as Mental Health First Aid (MHFA) (
36), have been shown to have a positive impact on mental health literacy and stigmatizing attitudes and may be an effective tool in rural African-American communities (
37–
40). However, literature suggests that providing both education and contact with a person who has experienced mental illness produces larger and more long-standing impacts on stigmatizing attitudes (
39). Thus adapting MHFA to include contact with individuals living with mental illness may more effectively address both mental health literacy and stigma in this population.
Participants emphasized the usefulness of prayer and other spiritual practices in promoting emotional wellness, which may partly explain noted preferences for pastoral counseling among African Americans (
41). However, participants also expressed concerns that traditional religious leaders might view mental illness as a spiritual failure rather than as a medical illness, which may serve to impede use of formal mental health services. Clinicians working with African-American clients should be aware that some clients may feel their own spiritual inadequacy has either caused or contributed to their illness. It could be useful for clinicians to know which local pastors accept a medical model of mental illness in order to enlist their assistance when appropriate to support treatment (
42).
Some limitations should be noted. Although our findings provide a rich understanding of how rural African Americans view mental health and mental health treatment, participants in this study tended to be younger and more educated than the larger rural African-American population, which is likely a function of the preselected stakeholder groups (that is, college students and administrators and providers) sampled in this study. In addition, the study was conducted in the rural South, and the results may not be generalizable to other rural African-American subgroups.
Conclusions
Mental health is an important concern among rural African Americans. These results provide important recommendations for developing culturally relevant strategies for improving mental health in rural African-American communities.
Acknowledgments
The authors thank Alice Deibel, Ph.D., Paul Koegel, Ph.D., Nancy Shoenberg, Ph.D., and Gery Ryan, Ph.D., for advice and guidance on this project.