Each year, roughly 14% to 20% of children and adolescents experience a behavioral health issue (
1), ranging from attention-deficit hyperactivity disorder to severe depression and suicidal or homicidal ideation. Because of shortages of psychiatrists (
2) and other pediatric mental health professionals, local emergency department (ED) and urgent care providers are often the only available behavioral health resources (
3). As a result, decisions about treatment are made by ED and urgent care providers or generalists directing care from hospital settings. The mismatch of care and need is associated with avoidable inpatient admissions, long wait times, or costly and potentially traumatic emergency medical service ambulance transfers (
4) to locations providing specialized services. Because community behavioral care resources interact with overburdened emergency care systems (
5), they are central to efforts to redesign policy and practice related to child mental health services (
6–
10).
Videoconference-based, synchronous psychiatric consultations (“telepsychiatry”) have emerged as one solution for distant providers to access behavioral health expertise (
11). The use of telepsychiatry to provide timely access to care has been well documented (
11–
13). Telehealth broadly has been identified as an avenue for increasing access to care, although whether it produces subsequent medical cost savings is unknown (
14,
15). Although community telepsychiatry for children and adolescents has been studied, the use of telepsychiatry emergency services for children has not been studied (
16), and associated clinical and fiscal outcomes are unknown (
13,
16,
17). This study compared process outcomes in a cross-sectional pre-post design at five pediatric ED and urgent care facilities sites before and after systemwide implementation of telepsychiatry consultation in 2015. Because economic evaluations often include multiple perspectives (
13,
18–
22), telepsychiatry-associated financial charges and time efficiency were evaluated from the hospital system perspective and satisfaction was evaluated from the provider and parent or guardian perspectives.
Methods
Setting
Children’s Hospital Colorado (CHCO) consists of a central academic medical center (hereafter, CHCO Main) at the University of Colorado’s Anschutz Medical Campus and a network of care comprising five pediatric ED and urgent care facilities (hereafter, network ED) in the greater Denver metropolitan area. Network ED locations are located between eight and 33 miles from CHCO Main, with average estimated travel times of 22 to 36 minutes. [A map of the area with estimated driving times between CHCO Main and the network ED locations is available as an online supplement to this article.] CHCO Main houses an ED with psychiatric emergency services provided 24/7 by a consultative team of behavioral health specialists, including pediatric psychiatrists and clinical social workers. Network ED sites do not staff in-house psychiatric consultants.
Operational data from network EDs indicate that behavioral health emergencies constituted almost 5% of all visits in 2013, more than twice the national average (
23). In 2014, 92% of patients presenting to a network ED site with a mental health problem required emergency medical (ambulance) transfer to CHCO Main for in-person psychiatric emergency service evaluation; more than one-half of these patients were subsequently discharged home with outpatient behavioral health resources; wait times between admission to the network ED, transport to and discharge from CHCO Main were typically long, exceeding 12 hours for roughly one-third of these patients.
Population
Inclusion criteria for telepsychiatric consultation at a network ED were broad: age under 18 years and presentation with a behavioral health complaint that was not immediately life threatening. Exclusion criteria were significant behavioral dyscontrol or complex medical comorbidities, including suicide attempts that required immediate medical treatment. Excluded patients were transferred to CHCO Main for usual care.
Usual Care for Psychiatric Emergencies
Pediatric patients presenting with a behavioral health emergency at a network ED were evaluated by a physician, nurse practitioner, or physician assistant. If the ED provider determined a need for a psychiatric crisis evaluation, the patient was then transferred by ambulance to the central campus for evaluation by the CHCO Main psychiatric emergency service and subsequent disposition: admission to CHCO Main, admission to another psychiatric inpatient facility on the basis of bed availability and insurance authorization, or discharge home.
Telepsychiatric Intervention for Psychiatric Emergencies
With the goal of reducing unnecessary patient transfers to CHCO Main, a synchronous telepsychiatry consultation model was implemented, linking patients at network EDs in real time with the centralized psychiatric emergency service staff instead of transporting them to CHCO Main for in-person consultation. The telepsychiatry intervention was progressively deployed during calendar year 2015 to one new network ED every four to six weeks from January to June.
Telepsychiatry implementation began with educational sessions that connected network ED staff to the CHCO Main psychiatric emergency service behavioral health team. Despite historical use of the usual care process, each network site had a unique work flow that was not coordinated with CHCO Main psychiatric emergency services. Work flows at each site were synchronized to create a new, comprehensive, and consistent algorithm that addressed equipment training, initiating consultations, diagnoses or presentations, troubleshooting, and potential consultation outcomes. A final systemwide work flow, described in the following sentences, was adopted. When eligible patients present to network EDs, the ED provider contacts the CHCO Main psychiatric emergency service behavioral health care team by phone to request a synchronous telepsychiatry consultation. The psychiatric emergency service team then secures a private consultation room at CHCO Main and sends a virtual meeting request via encrypted e-mail to the network location by using the hospital’s software-based, HIPAA-compliant telehealth platform. At the network ED, the nursing staff secures a room for the patient, assesses vital signs, and ensures patient and staff safety before connecting the patient with the psychiatric emergency service team. At this point, a video-enabled cart is rolled into the patient room to begin the live, virtual encounter. The interaction includes the CHCO Main psychiatric emergency services provider (typically a licensed clinical social worker), the child or adolescent patient, a parent or guardian, and the network ED attending physician or advanced practice provider.
During the virtual consultation, the psychiatric emergency service team member performs a standard clinical interview consistent with the CHCO Main usual care, in-person protocol and consults with the team at CHCO Main to make a disposition decision. After the joint consultation is completed, each parent or guardian is asked (not required) to complete a satisfaction survey for program evaluation. [A flowchart illustrating the steps in the telehealth evaluation is available in the online supplement.]
Data Collection
Patient encounter data were obtained from multiple sources. Each patient’s electronic medical record was linked with an anonymous study unduplicated identifier to a case report form on a secure, encrypted, password-protected research database (RedCap). The psychiatric emergency service staff also abstracted specific text fields from encounter records into a de-identified version of the RedCap database. Billing data for facility charges came from the hospital finance office, and data for provider fees came from the faculty practice plan. Satisfaction data were obtained by using the point-of-care surveys completed by parents or guardians and providers at CHCO Main and at ED network sites. This study was approved by the Colorado Multiple Institutional Review Board.
Dependent Variables
ED/urgent care length of stay (LOS).
ED LOS was defined as the length of time from initial admission at a network ED to discharge disposition. This time was measured by using a time stamp in the electronic medical record and reported in hours as a median and an interquartile range (IQR).
Discharge disposition.
Dispositions were measured by a mutually exclusive categorical variable with three possible pathways: path 1, admission to CHCO Main hospital; path 2, admission to another non-CHCO psychiatric facility when no beds were available at CHCO Main; and path 3, discharge home with referral for outpatient follow-up. Paths 1 and 2 were combined in analytic models into one disposition, inpatient admission, for comparison with path 3, discharge home.
Costs, charges, and expenses.
Costs of emergency care were measured from the hospital system perspective. Because the true costs of production were unknown, they were approximated by using billed charges for any facility and provider services during the network ED–initiated encounter. Average patient transfer cost for ground ambulance transportation was obtained from ambulance provider charges to CHCO Main. Telepsychiatry consultation costs were approximated as a proportion of the operational expenses to the CHCO health care system for the behavioral health team and the technological telehealth infrastructure. Telepsychiatry operational cost included both fixed and variable costs for the year: fixed costs included capital expenditures incurred for the purchase of the equipment (including operational software and technology infrastructure), annualized for the equipment’s applicable lifetime (
13,
20). Because the videoconference equipment was used for numerous other specialty care initiatives, psychiatric emergency service consultation expenses were prorated to the proportion of visits for psychiatric emergency service consultations as a ratio of all videoconference consultations. Variable costs included a prorated allocation of expenses for equipment maintenance, technicians, training, personnel wages, administrative support, and supplies (
20). The 2015 operational cost for telepsychiatry was estimated at $222,800.
Satisfaction with telepsychiatry.
A survey to assess the experience of telepsychiatry consultation from the perspectives of the provider and of the parent or guardian was administered immediately following the network ED encounter with items rated on a Likert scale of agreement, with 5 indicating strongly agree and 1 indicating strongly disagree. Respondents included the pediatric patient’s guardian, the network ED attending provider, and the CHCO Main–based psychiatric emergency services consultation provider. Surveys contained 14 questions from a previously validated telehealth satisfaction survey instrument (
24). The surveys contained no identifiers (other than type of respondent [provider or parent/guardian]), and were administered on paper at the point of care, collected by hospital staff, and provided to study staff through the institutionwide e-mail system. Surveys were administered at each interaction and voluntarily completed. No incentives were provided to respondents for survey completion.
Independent Variables
Demographic variables included age in years at date of ED admission, gender, race-ethnicity (Caucasian or non-Caucasian), and insurance type (public [Medicaid, State Children’s Health Insurance Program, or Tricare], private [commercial], or uninsured [self-pay]). Clinical severity was defined as the chief complaint with the highest severity at admission to the network ED, with suicidal intent with plan considered the most severe, followed by harm to self without plan, harm to others, major depression/anxiety, hallucination/delusions, or other complaint not otherwise specified.
Data Analysis
Descriptive bivariate and categorical variables for telepsychiatry and usual care were compared by using chi-square and Wilcoxon two-sample tests. ED LOS and charges were reported as medians with IQRs because of skewness. The likelihood of disposition to inpatient care compared with discharge home was modeled as a multivariable logistic regression adjusted for patient variables. Cost-efficiency estimated the difference in charges plotted against the difference in time saved for each path, using median values of usual care and telepsychiatry cases for comparison. Statistical analyses were conducted with SAS software, version 9.4.
Results
Table 1 describes the 494 pediatric patients who presented in 2015 at a network ED with a primary presenting complaint of an acute behavioral health condition. In early 2015 before implementation, usual care was received by 268 patients (54%), and after implementation telepsychiatry consultation was received by 226 patients (46%). Patients in the two groups did not differ statistically by age, gender, insurance type, or severity of chief complaint at network ED admission; however, there was a significant preponderance of Caucasian patients who received telepsychiatry compared with the proportion of Caucasians who received usual care before telepsychiatry was available (77% versus 69%, p=.036).
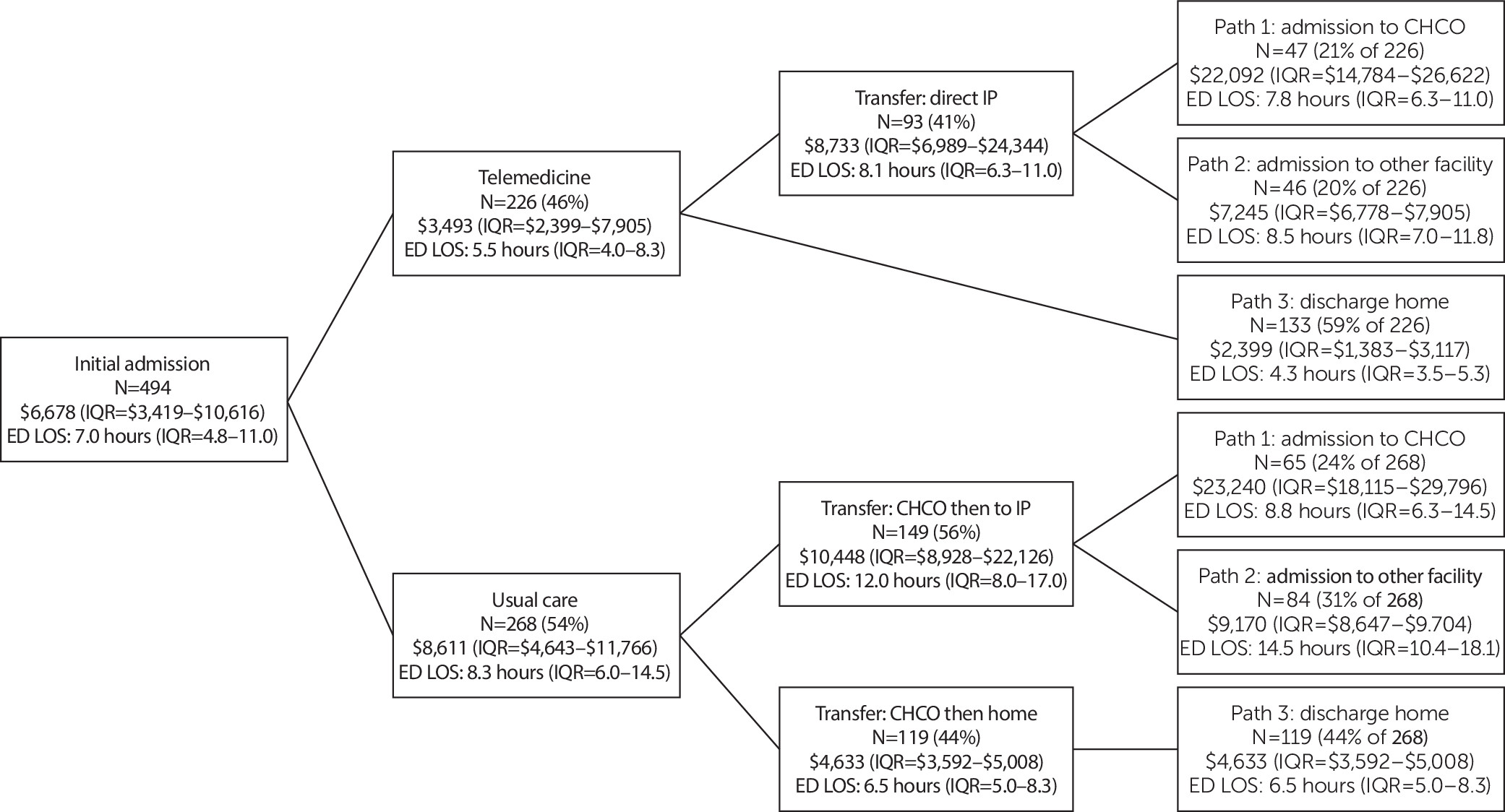
A decision tree illustrates the distribution of patients who received telepsychiatry or usual care (
Figure 1). For each care type, the figure reports the subsequent disposition of patients in any one of three pathways: path 1, admission to the CHCO Main inpatient psychiatric facility; path 2, admission to another inpatient facility if either a bed was unavailable at CHCO Main or the patient’s insurance preferred admission to another inpatient facility; or path 3, discharge home with outpatient follow-up. Each node displays median and IQR charges to the hospital system and also median and IQR ED LOS.
Median charges for telepsychiatry patients were $3,493 per patient (IQR=$2,399–$7,905), significantly lower than the median charge for usual care, which was $8,611 (IQR=$4,643–$11,766) (p<.001). Charges associated with inpatient pathways (admission to CHCO Main [path 1] or other facility [path 2]) did not differ statistically between telepsychiatry and usual care, with median charges of $22,092 per patient for telepsychiatry and $23,240 for usual care in path 1. Paths 1 and 2 terminal nodes included an ambulance transfer prior to inpatient admission and involved the most acutely ill patients. However, charges for path 3 differed significantly between telepsychiatry (median=$2,399, IQR $1,383–$3,117) and treatment as usual (median=$4,633, IQR=$3,592–$5,008) (p<.001), which included a transfer via ambulance.
The decision tree also describes LOS at network EDs in hours from time of network ED admission to time of final disposition. Overall LOS in the ED was significantly shorter for patients who received telepsychiatry (median=5.5 hours) compared with patients who received usual care (8.3 hours) (p<.001). LOS in the ED was significantly shorter among patients who were discharged home after telepsychiatry (4.3 hours) compared with patients who were discharged home after usual care (6.5 hours) (p<.001). Nearly 30% of telepsychiatry patients had ED LOS fewer than 4 hours compared with only 12% of patients who received usual care (p<.001) (data not reported). In terms of likelihood of disposition pathway, 42% of patients who received telepsychiatry were admitted directly as inpatients (21% to CHCO Main and 20% to another inpatient facility) compared with 56% of patients who received usual care (24% to CHCO and 31% to another facility), a significant difference (p<.001). In a multivariate framework, a logistic model found that after accounting for age group, race, clinical severity, gender, and insurance type, the likelihood of inpatient admission was significantly lower among patients who received telepsychiatry versus usual care (odds ratio=.59, 95% confidence interval=.40–.86, p<.001) [see online supplement].
To assess any safety signals for each type of care, cases of readmission to the network ED within 72 hours of discharge were measured. Among patients who received telepsychiatry emergency consultation, 85% had no return visit in the medical record in any interval compared with 90% of patients who received usual care, which was not a statistically significant difference [see online supplement]. No telepsychiatry patients, and only one usual care patient, returned to the network ED within 72 hours of discharge from the incident psychiatric emergency visit.
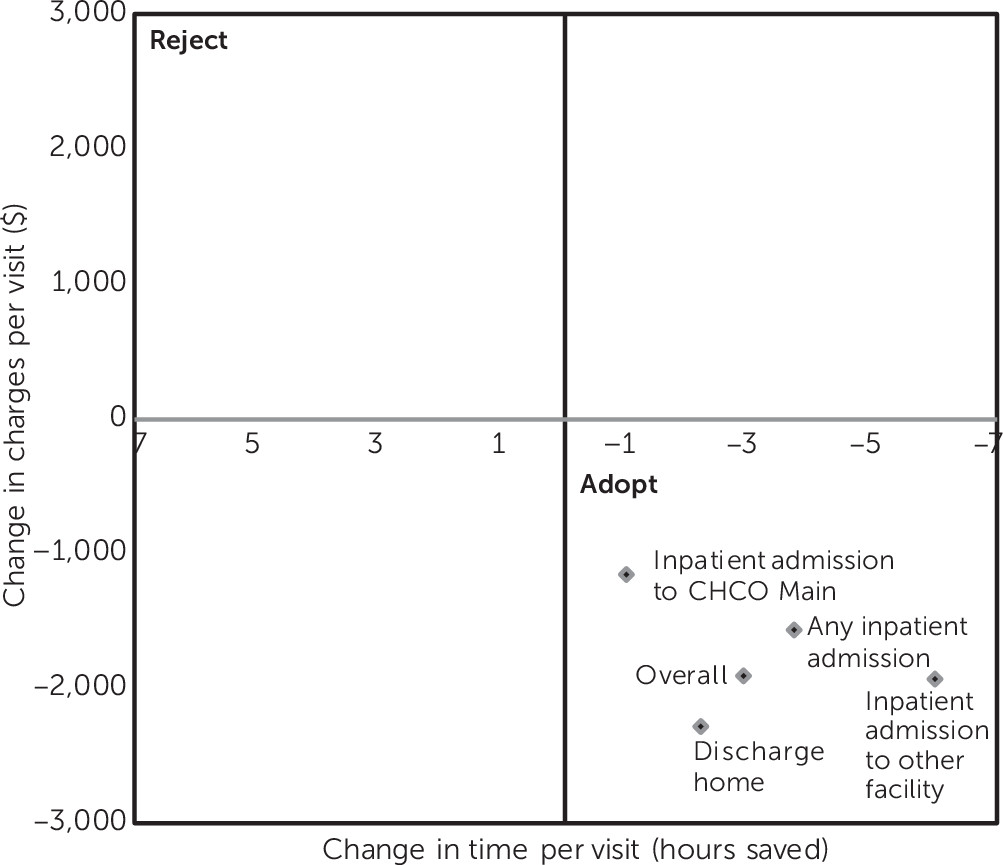
Figure 2 is a cost-efficiency plane (
25) that illustrates the relationship between the incremental gains for telepsychiatry over usual care in terms of median charges and the absolute value efficiency (time in hours) in ED LOS. A plotted value on the positive vertical axis would indicate that telepsychiatry was more expensive than usual care, and a value on the positive horizontal axis would indicate that telepsychiatry saved more time (fewer hours) than usual care. Current usual care charges and efficiency are represented at the origin; therefore, savings to the hospital system for telepsychiatry relative to usual care are plotted on the vertical axis below the origin. Efficiency in ED LOS is plotted on the horizontal axis; improved efficiency of telepsychiatry over usual care is plotted to the right of the origin. For each pathway on the decision tree
(Figure 1), telepsychiatry resulted in lower charges and shorter ED LOS; therefore incremental median change in each terminal node (paths 1–3, paths 1 and 2 [inpatient admission], and overall) is plotted in the lower right quadrant.
Table 2 reports mean satisfaction ratings for the 226 telepsychiatry consultations by parents or guardians (N=156, 69% response rate), network ED providers (N=160, 71% response rate), and CHCO Main psychiatric emergency service consultation providers (N=148, 65% response rate). The survey questions asked respondents to rate their agreement with statements about the telepsychiatry consultation in terms of overall acceptability, effectiveness, and efficiency and also allowed an open-ended write-in statement. With a 5-point rating scale (5, strong agreement; 4, somewhat agree; 3, neither agree nor disagree; 2, somewhat disagree; and 1, strong disagreement), average ratings by caregivers were above 4 (median=4.21–4.46), including reducing “inconvenience and unnecessary travel,” “technology easy to use,” and “would recommend it to others.” In write-in statements, parents and guardians expressed appreciation for not having to travel to CHCO Main, and ED network providers frequently commented that telepsychiatry “saved this family a transfer by ambulance.”
Discussion
This study used a natural experiment in clinical redesign to study the impact of a telepsychiatry consultation model for pediatric psychiatric emergencies implemented by a large academic children’s hospital and its geographically dispersed network sites. Over the year surrounding implementation, all signs indicated a successful clinical program: charges to patients were reduced, time (and therefore resources) was saved, caregivers and providers rated satisfaction high, and there were no safety signals based on readmission. Existing studies indicate that telepsychiatry can reduce travel, wait, and consultation time (
26), which is especially salient for patients with behavioral health complaints, who often use disproportionate amounts of resources and wait, on average, much longer than patients with nonbehavioral health complaints (
27).
Despite growing evidence of positive process outcomes associated with telemedicine, it is unknown how telepsychiatry affects patient-physician relationships (
28,
29) or how to price a telemedicine implementation. The few controlled telehealth trials (
30–
32) demonstrate either substantially reduced costs or dramatically improved outcomes. This implementation showed that subsequent hospital system resource savings (lower charges) associated with telepsychiatry were large enough to offset the original capital investment after approximately 120 patients had used the service. Other sites that consider implementation would have different costs based on their existing infrastructure and operational capabilities and, therefore, a different “break even” volume.
Telepsychiatry synchronous video consultation reduced unnecessary transfers, saved time for patients and families, and reduced stress associated with ambulance transfer. Patients, parents or guardians, and network ED providers all rated the services high on satisfaction. This finding is similar to other studies in that patients rarely report a less satisfactory interaction by videoconferencing than in-person (
24). Satisfaction scores for the behavioral health providers were more modest than those of the network ED providers, likely because they performed new additional telepsychiatry consultations in real time in addition to managing their standard workload and did so without additional staff resources. Point-of-care surveys showed that provider satisfaction was somewhat lower than patient satisfaction, consistent with existing research (
24). In postprocess review interviews with members of the CHCO Main psychiatric emergency services team, it was clear that the work flow of the team was affected by this model of telepsychiatry perhaps more than any network ED process. The team members’ biggest concern was that a telepsychiatry-enabled clinical interview could limit their ability to build a patient-provider relationship or decrease their ability to make an accurate clinical judgment. Since the 2015 implementation, the number of telepsychiatry visits have doubled without objection, suggesting that with greater experience using telepsychiatry, providers have become more accepting of the technology and, perhaps, gained some reassurance about its effectiveness as well as its efficiency.
This study had limitations and strengths. One limitation was the short follow-up and single site, nonexperimental design: we observed care for one year in one health care system by using a nonrandomized intervention. Nevertheless, the observed implementation created a quasi-experimental design that allowed us to measure the effect of telepsychiatry by using time and intervention. Also, once a site had implemented telepsychiatry, there were nearly no exclusions governing its use, and therefore confounding by indication was minimized. Primary variables were utilization and charges, rather than clinical outcomes and true costs of care; however, outcomes were all positive and no safety concerns were indicated. A study strength was the use of multiple perspectives, including those of parents and guardians, ED providers, specialty psychiatric emergency services behavioral health providers, and the hospital system.