Certified peer support specialists (CPSSs) are individuals who draw on their lived experiences of recovery from mental illness, substance use disorders, or both to promote recovery among others sharing similar experiences (
1). Prior research has documented common CPSS professional activities and wages (
2–
4). As this workforce matures, their roles evolve, leading to gaps in knowledge about their professional life (
5) and their financial well-being (
3). Research is needed to characterize CPSSs’ diverse professional activities and economic experiences, so that peer training can target their most effective roles (
6) and so that employers can better understand the extent to which their workers are economically vulnerable.
The current project used community-engaged methods (
7) to develop a statewide survey on CPSS roles, activities, self-rated skills, and economic well-being. Prior surveys suggested that the scope of CPSS practice is quite broad (
2), that their wages differ based on their gender and employer (
3), and that peer work benefits their own recovery (
4). Our study complements existing survey data by focusing on a new region and by controlling the survey’s distribution to enable a response rate calculation. A peer community advisory board identified the following research questions: What are CPSSs’ most common professional activities, and how strongly do they rate their skill in each activity? Does CPSS job satisfaction vary between different demographic and regional groups? and How do CPSSs describe their economic well-being?
Methods
The University of Michigan institutional review board designated the project as exempt human subjects research. The project team, which initially consisted of a university investigator [AL], a CPSS [MO], and a government administrator [PW], recruited a community advisory board (CAB) to design the survey. The CAB members consisted of five CPSSs from both rural and urban areas who represented diverse work settings, including community mental health, U.S. Department of Veterans Affairs (VA) facilities, and consumer-run centers. The CAB led survey development over four meetings and additional conference calls. The investigators used Qualtrics survey software (
8) for survey distribution. Two CPSSs piloted the survey for time to completion, which was approximately 15 minutes.
Final survey items represented four categories: demographic characteristics, professional activities, professional satisfaction, and wages and finances.
We asked respondents to state their age, race, work setting (for example, community mental health), and geographical service region. Although most regions yielded a large number of respondents, four had small numbers, which could have compromised anonymity. Therefore, on two occasions, we combined adjacent and demographically similar regions.
The CAB used the Michigan Medicaid provider manual to select CPSS tasks and enhanced this list with other activities related to recovery-oriented care (for example, facilitating self-determination). The final list of professional activities included benefits assistance, community visits, crisis support, developing or leading groups, financial education, health and wellness support, housing assistance, intake work, integrating physical and mental health care, person-centered planning, self-determination work, sharing recovery stories, vocational assistance, and welcoming and ambassador work. We asked respondents to state how often they engaged in each activity. When respondents indicated they engaged in an activity at least sometimes, survey display logic prompted them to rate the strength of their skill in that activity (1, not at all strong; 2, slightly strong; 3, moderately strong; and 4, very strong).
To assess job satisfaction, we asked questions on a 5-point scale (1, strongly disagree; 5, strongly agree) about the following areas: flexibility of hours, physical safety, promotion opportunities, job security, stress level, supervisor supportiveness, nonpeer staff supportiveness, and overall supportiveness. To assess satisfaction related to the broader professional climate, we adapted 10 items from the
Pillars of Peer Support, a document describing 25 factors that facilitate high-quality peer services (
9), into questions on a 5-point scale (1, strongly disagree; 5, strongly agree).
We asked respondents to report their current hourly wage. We also asked a single question used by economists as a metric of “financial fragility”: whether the respondent had the capacity to generate $2,000 in 30 days. This metric represents the cost of common financial shocks, such as a car repair or home maintenance (
10).
The government administrator who served on the CAB facilitated access to a database containing contact information for all Michigan CPSSs. The survey was password-protected. We used a gift-card lottery incentive to optimize the response rate.
We sent the survey invitation and Qualtrics link to each e-mail address in the database. Twenty-four e-mails were undeliverable, resulting in 1,128 valid invitations. We closed the survey after 24 days. Twenty-two surveys were removed because of incompleteness (for example, the survey was mostly blank) or duplication. The final sample consisted of 394 ostensibly unique respondents, for a response rate of 35% of all known CPSSs in Michigan.
We excluded 75 respondents from the analysis because they reported not currently working as a CPSS. The 319 respondents in the analyses reported that they worked in paid positions (N=271), volunteer positions (N=17), or both (N=31); when respondents indicated both, they were directed to answer questions based on paid positions. We grouped work settings into three categories for comparisons: community mental health (N=202), clubhouse or drop-in center (N=52), and other (N=61), which consisted of VA (N=25) and low-frequency settings, such as forensic settings and health plans (N=36).
We used SAS 9.4 for the analyses. We used analysis of variance to examine differences in wages, skill self-ratings, and satisfaction between regions and between categories of work settings. We examined boxplots, and the assumption of homoscedasticity was verified. T-tests were used to evaluate the differences between the race categories of Caucasian and non-Caucasian. We used correlations to examine relationships between age, skill self-ratings, and wages.
Results
Most respondents were female (208 of 303 respondents, 70%), between the ages of 40 and 59 years (187 of 301 respondents, 62%), and Caucasian (255 of 396 “check all that apply” responses, 64%). Most of the respondents had attended at least some college (272 of 303 respondents, 90%). [A table showing demographic information is available in an online supplement to this report.]
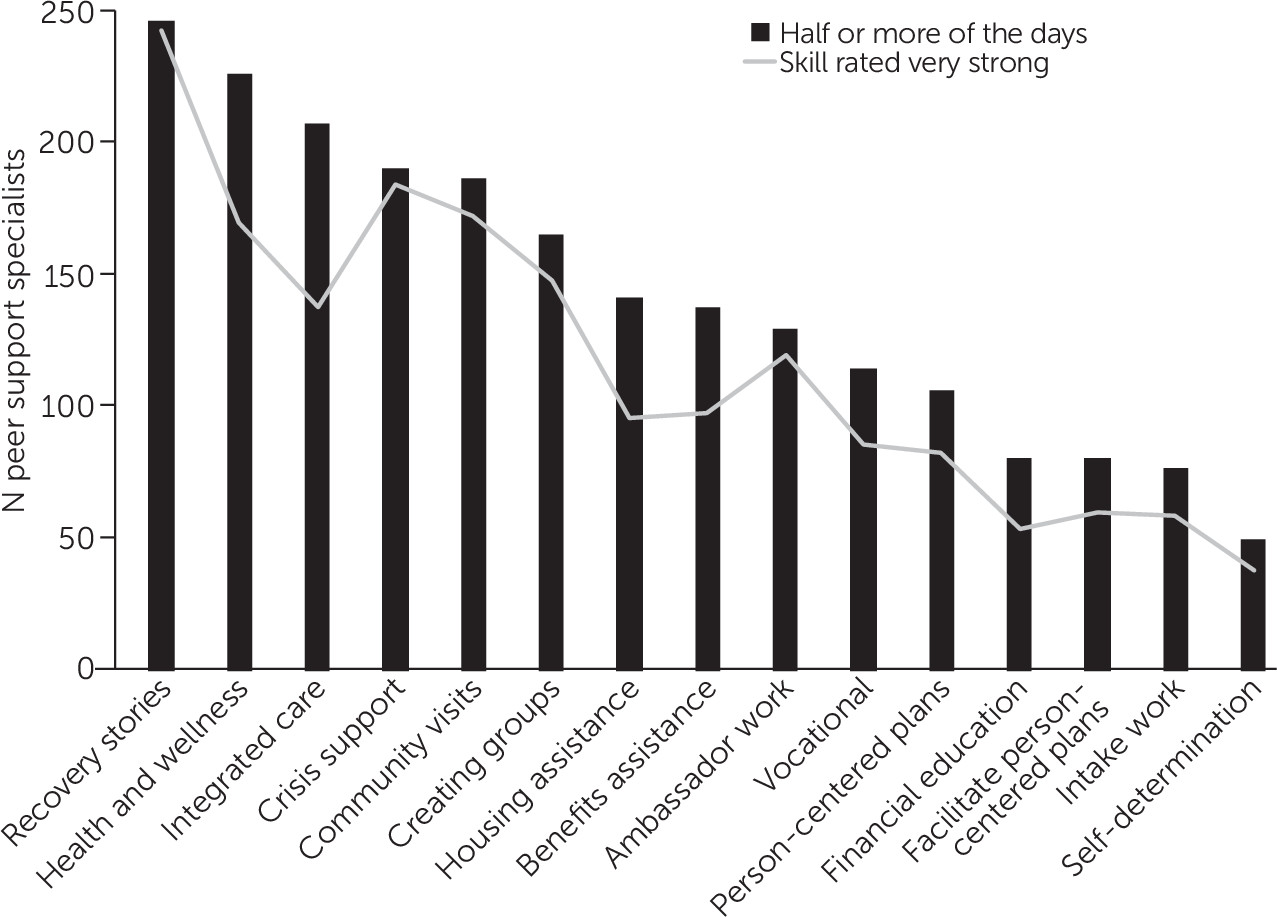
The most common professional activities were sharing recovery stories and health- and wellness-related tasks; the least common were self-determination work and intake work. The highest self-rated skills were sharing recovery stories and community visits; the lowest were financial education and vocational support.
Figure 1 shows both the frequency of activities (as bars) and the number of respondents who indicated their skill level as strong. We did not observe statistically significant differences in self-rated skill across work settings, regions, and demographic categories.
Work satisfaction questions were asked of respondents in paid positions, not volunteer-only positions. More than 75% agreed they were somewhat or strongly satisfied with physical safety at work (261 of 303 respondents), work hours (266 of 306 respondents), and supervisor supportiveness (237 of 305 respondents). Fewer agreed they were somewhat or strongly satisfied with their job security (205 of 304 respondents, 67%), stress level (157 of 304 respondents, 52%), and chances for promotion (124 of 302 respondents, 41%). On items adapted from Pillars of Peer Support, more than 80% somewhat or strongly agreed that their job description is clear (265 of 303 respondents), their competencies relate to their job description (280 of 304 respondents), they have knowledge of the impact of trauma (280 of 303 respondents), they have access to continuing education (246 of 301 respondents), and they are aware of the peer code of ethics (294 of 305 respondents). However, only half (152 of 294 respondents) somewhat or strongly agreed that they have opportunities for professional advancement, and less than half (126 of 299 respondents) somewhat or strongly agreed that nonpeer staff are trained about the peer role. There were no significant differences in satisfaction on items adapted from Pillars across work settings, regions, and demographic categories.
Respondents reported an hourly wage ranging from $8.50 to $20.00 or more per hour, with a mean of $14.90. [A figure showing respondents’ reported wages is available in the online supplement to this article.] Twenty-three of 297 respondents (approximately 8%) reported that they made more than $20 per hour. Because of censored wage data, in order to analyze wages by region, “more than $20” was set to $23. We did not observe statistically significant differences in hourly wage across work settings or demographic categories. We observed significant group differences in hourly wage between regions (F=7.60, df=7 and 245, p<.001). On the financial fragility assessment, 115 of 301 respondents (38%) were “certain” they could not generate $2,000 in 30 days if an unexpected need arose, and another 83 (28%) stated they were “probably” unable to do so, resulting in a financial fragility rate of 66%.
Discussion and Conclusions
Our community-engaged study provides information about CPSSs’ self-reported professional activities, skills, job satisfaction, and financial situation. The project complements prior CPSS surveys by having had access to all known CPSSs in one state and by using novel methods to determine the survey response rate. Thirty-five percent of known CPSSs in the state of Michigan took our survey.
Solomon’s 2004 analysis of processes underlying peer services included the process by which clients can discover new ways of coping through learning about a peer’s experiences (
1). Our sample described activities consistent with this analysis, because sharing recovery stories was their most frequent professional activity and strongest self-rated skill. Davidson et al. (
6) noted the importance of assigning peers to jobs in which they use skills acquired through life experiences and training. Our survey suggests specific training needs, as it documents variations in skill self-ratings. We observed that skill self-ratings, while high across the board, are comparatively lower for financial education, housing support, and vocational support. Peer trainers could focus their efforts on these specific areas to help align CPSS practice with self-reported skill.
Our results also indicate that CPSSs in Michigan often experience financial fragility. CPSS wages are low relative to those of other health professionals. The average wage for our respondents was $14.90 per hour, fairly consistent with a national survey of peer support specialists that found an average of $15.42 per hour (
3).
The results of this study should be considered in the context of some limitations. Findings may not be generalizable to other states. We cannot be certain whether ineligible respondents or repeat surveys made it into the data set, although we took precautions to decrease this possibility (for example, sending the Qualtrics link only by direct e-mail and having a password-protected survey). The study was descriptive and did not test hypotheses. Despite these limitations, our study allowed a large proportion of CPSSs in a single state to share their voices, and helped foster a robust community-university partnership that continues to collaborate on new projects to this day.
A majority of respondents were satisfied with most aspects of their jobs. However, there was relatively less satisfaction with promotion opportunities. These findings are consistent with scholarship suggesting that both advancement and lateral moves often require leaving the CPSS profession (
5). Conduits for advancement within the CPSS profession, rather than outside of it, could improve job satisfaction, particularly if such opportunities result in a pathway toward better economic well-being.