An orientation in mental health services toward supporting recovery is recommended internationally (
1) and is central to national policy in many countries (
2–
5). Interventions involving collaborations between mental health professionals and peer providers are particularly effective at increasing recovery, hope, and empowerment (
6). Recovery colleges have been described as a “radical” embodiment of recovery-oriented services (
7). Recovery colleges involve supporting people living with mental health problems through adult education rather than through treatment (
8). The concept of “recovery education”—supporting recovery in relation to mental health problems through education—was developed in Boston and Phoenix in the 1990s.
In the past decade, a model of recovery colleges has emerged in the United Kingdom, with a greater emphasis on coproduction and colearning. The first recovery college opened in London in 2009, and there are now more than 80 in the United Kingdom (
9), even though recovery colleges were first mentioned in national policy only in 2017 (
10). This rollout has been supported by the national recovery transformation program in England called Implementing Recovery through Organizational Change (ImROC), which identified recovery education centers as central to the development of a recovery orientation (
11).
The recovery college model developed in England has been widely replicated internationally. Sometimes called “discovery centers” or “empowerment colleges” or “recovery academies,” recovery colleges are now open in Australia, Bulgaria, Canada, Hong Kong, Ireland, Italy, Japan, the Netherlands, Norway, Poland, and Uganda, among other countries (
12), and an international community of practice has been established (
13). Reasons why this model of recovery college has not gained traction in the United States have not been investigated. Most colleges are funded by health services, although there is an increasing movement toward a wider range of funding, including from employment and education departments of national government, international sources (for example, the European Union Regional Development Fund), and nongovernmental organizations.
Recovery colleges are based on pedagogical principles from adult education rather than clinical or therapeutic models (
8). Defining features of recovery colleges are that they are collaborative, strengths based, person centered, inclusive, and community focused (
14). Individuals who use mental health services and attend recovery colleges are known as students instead of patients or service users. Others, including family members and mental health professionals, also attend as students. After registration, students attend self-selected courses codelivered by peer trainers (individuals with personal experience of mental ill health and recovery) and nonpeer trainers (for example, clinicians or topic experts).
A key feature of recovery colleges is the emphasis on coproduction—that is, individuals with lived experience coproduce all aspects of the college, including curriculum development, quality assurance, and course delivery, alongside a trainer with professional or topic-specific expertise. Recovery colleges typically directly employ a small team of peer and mental health practitioners, with a larger group of peer trainers and practitioner trainers from mental health services and community agencies who are used on a sessional basis. Courses vary from brief, one-hour, introductory sessions to ten-week courses with classes held one day per week (
12). Because they are locally coproduced, curricula vary from college to college, but courses offered typically cover the following: understanding various mental health issues and treatment options; rebuilding life with mental health challenges; developing life skills and confidence to either rebuild life outside services or get the most out of services; capacity building and developing the peer workforce; and helping people provide support for family members and friends who experience mental health challenges. Recovery colleges are emerging internationally as a central feature of system transformation toward a recovery orientation (
15).
There is preliminary evidence that recovery colleges are popular, support goal achievement, improve well-being, and reduce service use (
12,
16–
19). However, almost no robust evaluative research has addressed how they work and what outcomes they produce for students. The lack of empirical evidence for an approach that is being implemented at scale in many countries is an important gap in scientific knowledge.
The aim of this study was to develop a testable change model for recovery colleges, characterizing the mechanisms of action and the outcomes for mental health service users who attend recovery colleges.
Methods
This research was undertaken from February to November 2017 as part of the Recovery Colleges Characterisation and Testing (RECOLLECT) study (researchintorecovery.com/recollect). The University of Nottingham Ethical Committee approved the study (Nottingham REC 1, 18.1.17, 16/EM/0484). All participants provided informed consent.
Design and Setting
We conducted a systematized review involving collaborative analysis of included papers, followed by qualitative interviews with stakeholders. To reduce bias in the characterization of mechanisms and outcomes that may have arisen from the research team members’ clinical priorities, we formed a Lived Experience Advisory Panel (LEAP) of recovery college students who were mental health service users, service users who were not students, and family members (N=9) from the three study sites—recovery colleges in Leicestershire, London, and Sussex in England. LEAP members were involved as coresearchers throughout the study; they provided primary data, undertook collaborative data analysis to produce the theoretical framework, coproduced the change model, and coauthored this report.
Procedures
A systematized literature review (
20) was conducted. Inclusion criteria were as follows: related primarily to recovery colleges, online publication date 2016 or earlier, available in electronic form, and published in English. The review excluded any document that was a college prospectus—that is, a course list for a specific college. Publications were collated from five sources: a repository of published, peer-reviewed academic publications (researchintorecovery.com/rcrg); expert consultation with the ImROC national transformation program director and consultants (N=5), international experts (N=7), and the Recovery College International Community of Practice (N=54); conference abstracts (Refocus on Recovery conferences in 2010, 2012, 2014, and 2017; European Network for Mental Health Service Evaluation conferences in 2011, 2013, and 2015) with author contact; publications citing included articles (using Web of Science); and reference lists of included publications. All included papers were reviewed, and a subset was identified by the research team as of relevance to the research question.
The LEAP met to identify candidate mechanisms of action and outcomes from their own experiences. Four research team analysts independently used inductive coding of key publications, incorporating LEAP data as a priori codes, to identify themes related to mechanisms of action and outcomes. Themes were refined in collaboration with two expert qualitative researchers to develop an initial coding framework. The LEAP then met to undertake collaborative data analysis (
21). LEAP members offered alternative perspectives to challenge researcher assumptions, commented on the content and language of the initial coding framework, and addressed ambiguities and differences of interpretation identified by the research team. Such issues were explored and where possible reconciled. After the meeting, minutes, flipchart outputs, photographs of visual representations, and researcher field notes were used by the research team to finalize the theoretical framework for the change model, which was sent to LEAP coresearchers for review.
Remaining publications from the systematized review were deductively coded by the research team by using superordinate categories from the theoretical framework. Coding involved identification and allocation of text related to the theoretical framework, enabling related text to be grouped and compared and allowing identification of themes occurring within and across sources; regular discussions between analysts explored how mechanisms of action and outcomes were expressed and related to each other, which allowed lower-order themes to be recognized (
22). This process developed candidate components for inclusion in the change model. The LEAP met to develop a preliminary change model from these components. Using a change model related to peer worker interventions as a template (
23), LEAP members organized the components into a diagram characterizing the preliminary change model.
Stakeholders from the three study sites were identified: individuals directly involved with recovery colleges (students, peer trainers with lived experience, trainers with professional or topic-specific expertise, and recovery college managers); community-based and mental health service–based partners; and commissioners. Semistructured interviews were conducted to obtain proposed refinements to the theoretical framework and the preliminary change model, with a topic guide that employed open questions and probing. Because the focus was on refinement, a proportionate-analysis approach was used. Recordings and field notes were reviewed by the research team to identify refinements, producing the final theoretical framework and model of change.
Results
Forty-four publications related to recovery colleges were identified. [A table listing these publications and their key features is included in an
online supplement to this article.] Included publications comprised nondata opinion pieces (N=12) and mixed-methods (N=14), qualitative (N=10), and quantitative (N=8) studies. Most (N=36) were from the United Kingdom, followed by Australia (N=5). Studies reporting data were mainly single site, and all involved nonexperimental designs with either cross-sectional or pre-post designs. Positive claims were made both frequently and without robust empirical justification—for example, “It was personal narratives that impacted on the room with such potency. Images of possibilities, evidence of human achievement” (
24).
Ten publications were identified as key papers of high relevance, spanning theory, development, evaluation, and best practice [see first 10 listed papers in the online supplement]. The LEAP identified 10 mechanisms of action (for example, learning from others, learning together, making social connections, participating in a group or an activity rather than receiving a transactional service, and inclusion) and seven outcomes (for example, self-confidence, empowerment, meaning, and purpose). Inductive analysis by researchers of key publications developed an initial theoretical framework comprising four mechanisms of action (increased agency, transformed relationships, identity development, and personal growth) and two outcomes (change in the student and change in the student’s life) [see initial framework in online supplement].
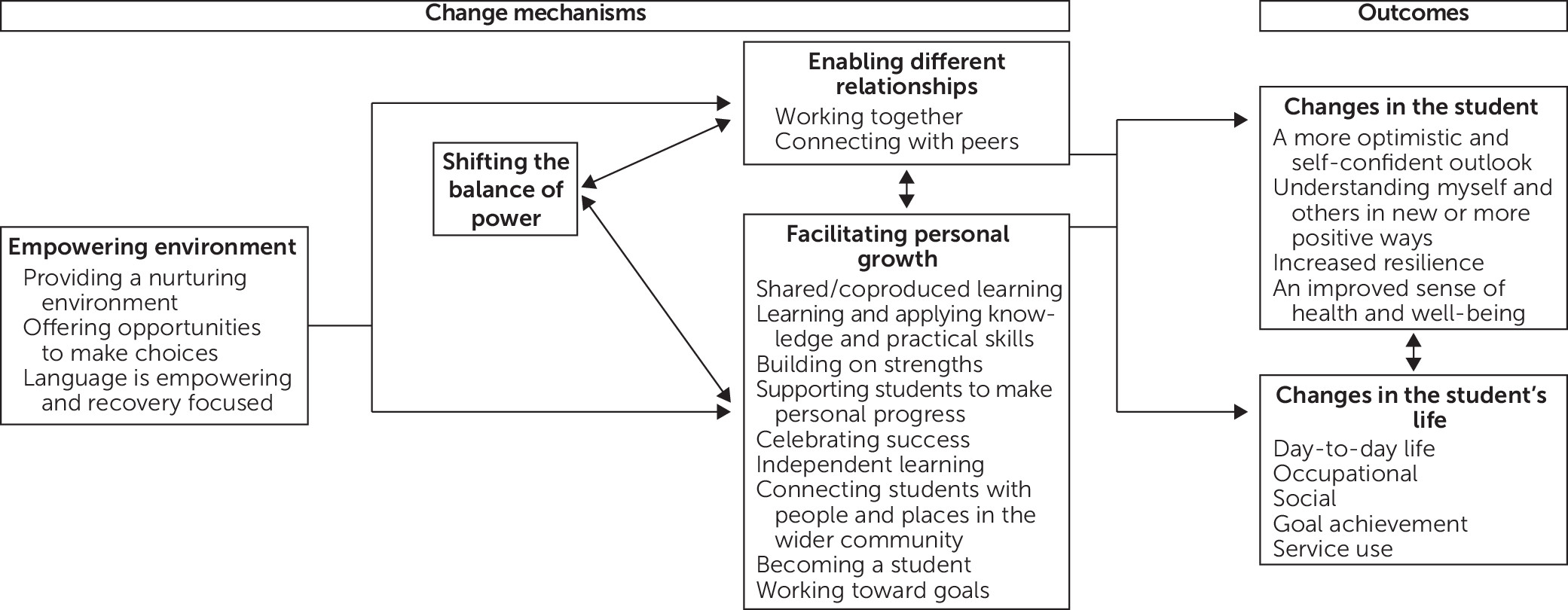
The collaborative data analysis workshop identified refinements, including recommended deletion of the superordinate category identity development, because it implied having an inferior or defective identity prior to joining a recovery college. The resulting codeveloped theoretical framework comprised three mechanisms of action (empowering environment, enabling different relationships, and facilitating personal growth) and two outcomes (change in the student and change in the student’s life) [see online supplement].
The deductive coding of the remaining 34 publications identified new codes for mechanisms (for example, language and community links) and outcomes (for example, leisure and service use) [see online supplement for definitions and exemplar text]. All mechanisms and outcomes were identified as positive contributors, and no harms from recovery colleges were reported. The five superordinate categories were all coded in at least 21 (range 21–27) of the 34 publications, indicating coding framework validity. The LEAP developed a formative model of change, hypothesizing causal relationships between mechanisms and outcomes.
Stakeholders interviewed were students who also used secondary care mental health services (N=12), peer trainers (N=4), clinician trainers (N=3), recovery college managers (N=3), mental health commissioners (N=1), NHS Trust clinicians (N=2) and managers (N=1), and local community partners (N=7). Only minor refinements to wording and order were made to produce the final theoretical framework for mechanisms of action and outcomes (see box on next page) and the final coproduced change model (
Figure 1).
The change model hypothesizes that an empowering environment provides the context for a student’s experience and involves the creation of a physical place, emotional space, and workforce that is friendly and welcoming. The emphasis on personal growth arises from the use of adult learning approaches: “College is knowledge” as one peer trainer put it. The relationships that arise from this educational approach are different from those that result from traditional clinical interactions, both because peers engage in more active interactions with each other and because they are relating in new ways to clinicians (as trainers and as students) in the recovery college: “the ‘Us and Them’ culture is being questioned in the recovery college classroom” (
24). Relationships and personal growth are mediated both by the environment and by power balances. The emphasis on shifting the balance of power arises from the coproductive culture of recovery colleges, which “emphasises reciprocal relationships where users of public services are recognised as active agents with positive capabilities rather than passive beneficiaries” (
14). Relationships, growth, and power interact, with more empowered students relating differently to others and having higher expectations about self-efficacy.
These processes lead to changes in the student’s inner world and to self-initiated changes in their interactions with the outside world. A LEAP member noted, “Recovery is about transformation,” which happens within the student. Changes in identity are proposed, including improved self-esteem, self-knowledge, and well-being. Along with gaining increased confidence, skills, and resilience, students become more optimistic and confident about dealing with the challenges of living well. A LEAP member also noted, “Wellness is about living, not about being symptom-free,” and changes in students’ attitudes led to, and were reinforced by, observable changes in their lives. Key domains of change were in lifestyle choices and social and occupational engagement. An impact on service use was identified, either in the direction of less use through increasing independence or more use through increasing engagement with services.
Discussion
A theoretical framework and testable change model for recovery colleges were coproduced by academic researchers and a panel of persons with lived experience of mental illness and family members. The four identified mechanisms (environment, power, relationships, and growth orientation) were contrasts from traditional mental health services. The two categories of outcome—change in the student and change in the student’s life—were located as mutually reinforcing processes of reconnection with self and reengagement in life in new ways. Additional research by the authors will add to the understanding of this process by identifying the key components of recovery colleges (unpublished data, Toney R, Knight J, Hamill K, et al., 2018).
The emphasis on an empowering environment reflects the importance placed on context. In part, this aligns with existing clinical recommendations regarding experiences of individuals who use services, such as engaging people in a “warm . . . respectful and professional manner” on arrival (
25). However, the recovery college environment was framed as an active part of the support, with an emphasis on hospitality and the built environment. The emphasis on choice was consistent with the importance attached to shared decision making in mental health services (
26) but went further in focusing on providing opportunities for choice at every interaction, such as through registration by self-referral (most recovery colleges do not allow referral by clinicians) and course choice (students choose their own courses). This approach is consistent with empirical studies showing optimal outcomes from active rather than shared decision making (
27). It also accords with the move away from “nonadherence” (
28) toward community engagement (
29).
Power is a difficult issue to discuss in mental health systems. Evidence is emerging of the incompatibility between ratified human rights legislation and compulsion-related practice (
30). Thus there is a credible case for reexamining current power arrangements. Recovery colleges provide a context in which support is given with no compulsion, and active efforts are made to reduce power differentials—for example, by having peer and clinician trainers codeliver courses. This modeling of interactions between individuals with service use experience and clinical expertise as a relationship of equals is a key feature of recovery colleges.
Relationships are recognized as central in mental health services (
31), because a “better therapeutic relationship predicts better outcomes” (
32). However, this instrumental focus differs from the recovery college emphasis on mutuality—the idea that both parties in a dyadic relationship will be changed (
33). Both peer and nonpeer recovery college workers are expected to be open to personal change and growth. Further blurring of the roles occurs through an organizational culture supporting “disclosure comfort” (
34) of personal experiences by workers and provision of active support for existing students to take on responsibility (for example, as a course tutor or a mentor for new students), all of which reduce distinctions between students and workers in a recovery college.
Finally, the focus on growth builds on the coproduction and adult education–pedagogical approaches that are central to recovery colleges. This is informed by a number of resource-oriented approaches in mental health (
35). Areas of emphasis in recovery colleges include celebrating success, such as graduation ceremonies after course completion; independent learning, including through book libraries and online access to learning materials; and active support for students to move on to mainstream education and occupation.
Outcome categories in the framework are changes in the student and changes in the student’s life. The coproduced change model indicates an interaction between these two outcome categories, which is consistent with findings from psychological therapy that neither cognitive nor behavioral changes are individually sufficient for sustained transformation. These two outcome categories align with the CHIME framework (Connectedness, Hope, Identity, Meaning, Empowerment) of recovery processes (
36–
38), although with a stronger emphasis on increasing self-knowledge and self-confidence, which perhaps differs from traditional services. Evaluations of peer support interventions in randomized controlled trials have tended to use primary outcomes related to intrapsychic processes (
39), and our study highlights the need for evidence of recovery-supporting interventions for social and occupational outcomes.
This study developed the first theoretically grounded change model for recovery colleges. Several approaches were used to reduce bias, including the triangulation of data sources (LEAP, publications, and interviews), the use of multiple analysts and collaborative data analysis to develop the coding framework, coproduction of the change model with advisors with lived experience, and involvement of multiple stakeholder perspectives in the change model validation.
Three limitations can be identified. First, a nonsystematic search strategy was used to identify publications. The rationale was that the existing online repository of academic publications is likely to be complete because “recovery college” is the term used most commonly for these services. However, other related approaches are emerging, such as recovery education centers, discovery colleges, and empowerment colleges. A second limitation is the use of field notes rather than formal transcript analysis. The aim of the interviews was to refine an existing model rather than develop new theoretical understanding, but more detailed analysis may have captured additional information about suggested refinements. A final limitation is the use of only three recovery colleges as study sites, all of which were informed by ImROC in their development, which limits their diversity.
Conclusions
This study’s findings have three implications. First, they can inform clinician judgment about which individuals from their caseload to particularly encourage to attend a recovery college. The change model characterizes how recovery colleges may provide transitional support toward increased community participation and development of a more layered identity beyond being a person with mental health problems. Indeed, an explicit principle of recovery colleges is that they are “open to all” (
12). From this perspective, anyone using mental health services may benefit from attending a recovery college. Therefore, general encouragement to all service users to consider enrolling as a student is indicated. However, on the basis of the identified mechanisms of action and outcomes, clinicians may particularly want to encourage four specific subgroups of mental health service users to register as recovery college students. First, service users who are early in their recovery journey and not yet confident in making choices about their life may benefit from an enabling environment in which choice is supported and positive growth is expected. Second, individuals with whom mental health services struggle to engage may benefit from a nurturing and safe environment in which different relationships are possible and where there is an emphasis on shifting the balance of power. Third, service users who have high self-stigma or do not believe recovery is possible for them may benefit from exposure to peer trainers and other students who are “credible role models of recovery” (
40). Finally, service users whose lives lack social capital and who live in a “virtual institution” (
41), where their social environment (social network, place of living, and how time is spent) is primarily or exclusively indexed on mental ill health may benefit from the social connectedness and wider community connections offered in recovery colleges. Establishing the validity of these recommendations and determining whether there are subgroups for whom recovery colleges may be less beneficial are important future research goals.
Second, the identified mechanisms of action have implications for organizational culture within mainstream mental health services. There may be lessons to learn from a more established prorecovery innovation—the introduction of peer support workers into the workforce. A recent review identified a number of implementation barriers related to peer support workers, including the lack of credibility of peer support worker roles, professionals’ negative attitudes, tensions with service users, struggles with identity construction, cultural impediments, poor organizational arrangements, and inadequate overarching social and mental health policies (
42). It is feasible to anticipate that similar challenges may arise as recovery colleges become more established. The extent to which the culture of mental health systems is compatible with mechanisms such as empowerment through active decision making, mutuality, support of student-directed learning, and community participation is unclear, not least because of the ongoing conceptual debates about the core purpose of mental health systems and social care systems (
43). This suggests that sustained implementation of recovery colleges may have an impact on, and be affected by, organizational culture within health and social care systems.
Finally, current evidence suggests that recovery colleges are popular with students and produce a range of positive outcomes (
12,
16,
44). However, the evidence base is not yet scientifically robust. Evaluations of recovery colleges with randomized and nonrandomized controlled trials should be a priority of research funders, both to investigate the effectiveness and experience of using recovery colleges and to establish likely return on investment. The development of a testable change model will support formal evaluation of whether, and how, recovery colleges support recovery.
Acknowledgments
The authors gratefully acknowledge the support of the recovery college managers (Lucy Locks, Sussex; Kate Hamill and Marie McGranaghan, Leicestershire; and Gabrielle Richards and Kirsty Giles, SLaM) and all the recovery college students and staff, NHS clinicians, and further education college staff who took part in this study. The work of Jane McGregor, who passed away before publication, directly informed this research.