Emerging from an era of high operational tempo and rotating deployments, military personnel are experiencing high levels of psychological concerns, including posttraumatic stress, anxiety, depression, and substance abuse (
1–
4). In 2017, mental health complaints were the leading reason for hospitalization and the third leading reason for outpatient visits among active duty personnel (
5,
6). Mental health issues can affect service members’ long-term health, quality of life, job performance, and career trajectories (
7,
8); thus it is essential to connect service members with high-quality mental health services. One critical step in making that connection is to increase service members’ willingness to seek mental health care before a crisis occurs.
Despite having access to mental health care, many service members do not seek behavioral health treatment (
2,
9,
10). Stigma surrounding the use of mental health services, along with myths associated with mental health treatment, discourages people from seeking care (
2,
11). In particular, negative attitudes toward mental health treatment in the military are associated with decreased intentions to seek help, as well as more negative perceptions of mental health care utilization (
10,
12,
13). Additionally, a recent review of qualitative literature further elucidates reasons for treatment avoidance among service members (14), including refusal to acknowledge symptoms because of concerns over stigma or disclosure, internalized social stigma, and military system factors, such as how leaders may support or detract from help seeking.
Research suggests that interventions that familiarize service members with behavioral health treatment and address mental health–related beliefs may be effective in reducing stigma and promoting health care seeking (
15,
16). Specifically, interventions that increase service members’ contact with peers who have experienced mental health issues or with mental health care providers—either in person or indirectly—have yielded positive results (
17–
19). For instance, a training program for Marine Corps leaders sought to demystify mental health care by increasing contact with providers and peers with a mental health condition via in-person training. The training, which consisted of a stigma reduction toolkit and an educational video, was shown to improve leaders’ perception of the efficacy of mental health treatment and reduce their perception of negative consequences of treatment seeking on future deployability (
20). Although the results of the study showed promise, the study did not evaluate the components of the training (i.e., toolkit and video) individually or examine the effect of in-person contact with a provider.
This research extends the previous work by evaluating whether the video alone—without the corresponding toolkit or the more time-intensive, instructor-led training—decreases social stigma toward mental illness and treatment. The study hypotheses were that service members who viewed the video (both with and without provider-led discussion) would report decreased social stigma toward mental illness and treatment, increased willingness to seek help, and increased personal desire for mental health care compared with a control group. Additionally, it was hypothesized that the addition of pre- and postviewing discussion would increase the effectiveness of the video in reducing social stigma, increasing willingness to seek help, and increasing personal desire for mental health care.
Methods
Participants and Procedures
Study participants were recruited from three overseas U.S. Marine Corps bases. A repeated-measures, randomized control group design was used to evaluate the video. After providing consent, participants were randomly assigned to one of three study groups: intervention video only, intervention video plus discussion, or control condition. The control group watched a video on nutrition that was unrelated to mental health issues. Participants completed paper-and-pen questionnaires in a group setting (approximately 30 participants per group) at baseline (i.e., pretest) and posttest (i.e., immediately after completion of training) and a Web-based questionnaire 6 weeks later. The study protocol, including all procedures for this study, was approved by the Naval Health Research Center Institutional Review Board in compliance with all applicable federal regulations governing the protection of human subjects.
Intervention
The 35-minute intervention video was previously developed as part of an antistigma toolkit for Marine Corps personnel (
20). The video includes 11 segments that address issues related to mental health treatment previously identified as being poorly understood by service members (
21). Specifically, the video shows three mental health practitioners with military backgrounds discussing topics such as types of providers, common concerns about and barriers to seeking help, and treatment options primarily related to posttraumatic stress. Participants in the video-plus-discussion condition participated in a 10-minute group discussion led by a clinical psychologist both before and after the video to highlight key content.
Measures
The questionnaires assessed demographic and service characteristics, social stigma for mental health care, willingness to seek help, and personal desire for mental health care.
Demographic and Service Characteristics
Participants reported their age, sex, education, race-ethnicity, military rank, and deployment history at pretest.
Social Stigma
Public stigma toward mental illness is the reaction of the general public toward people with mental illness (
22), a definition that has been used by researchers in a review of stigma toward mental health problems in the military (
19). Building on that, social stigma is defined in this study as the tendency to endorse values and behaviors of public stigma, such as discrimination, marginalization, stereotyping, and increased social distance. At pretest, posttest, and follow-up, social stigma was measured with a 23-item scale adapted from previous stigma assessment efforts (
2,
23–
25). (Scale items are listed in an
online supplement.) Participants indicated the extent to which various factors would affect their decision to receive mental health services, from 1 (strongly disagree) to 5 (strongly agree). Higher scores indicate greater social stigma. Item responses were averaged to compute a total scale score (α=.85).
Willingness to Seek Help
A 10-item scale developed by the investigators assessed willingness to seek help at all time points. Participants were asked how willing they would be to seek help for stress or an emotional problem (if they ever had such a concern) from a variety of resources or providers (e.g., mental health professional attached to a unit, military chaplain). Response options ranged from 1 (very unwilling) to 5 (very willing); item scores were averaged to compute a total scale score (α=.91).
Personal Desire for Mental Health Care
Marines reported their personal desire for mental health care at pretest and at the 6-week follow-up. At each assessment, participants chose one of the following response options: never wanted help, wanted but did not seek help, wanted and sought help but have not received any yet, and wanted and received help. At pretest, the time frame was since joining the military; at follow-up, it was in the past 6 weeks. Responses were dichotomized to reflect whether participants wanted (1) or did not want (0) help for a stress-related or psychological problem.
Analysis
Descriptive statistics and chi-square tests were conducted to determine the distribution of all variables within groups and whether there were differences between groups in the distribution of variables, respectively. Mixed-model ANOVAs with condition (video only, video plus discussion, and control) as a between-subjects factor and time of measurement (pretest or posttest) as a within-subjects factor were used to examine the hypothesis that service members who viewed the video (both with and without discussion) would report decreased social stigma and increased willingness to seek help at posttest compared with a control group. These analyses were repeated by excluding the control condition to test the hypothesis that the pre- and postviewing discussion (vs. video only) would increase the effectiveness of the video in reducing social stigma and increasing willingness to seek help at posttest. Similar analyses of social stigma and willingness to seek help were also conducted at follow-up. Differences between the intervention and control groups in personal desire for mental health care at follow-up were analyzed by using logistic regression, controlling for baseline personal desire for mental health care. All analyses initially controlled for demographic and service characteristics; because inclusion of these covariates did not alter results, unadjusted results are reported for parsimony and to maximize power. IBM SPSS Statistics software (version 23) was used to analyze the data.
A power analysis for a repeated-measures ANOVA test was performed with 3 measurement time points by using a conservative estimated Cohen’s d effect size of .10 for the primary outcomes, 80% power, and 5% significance. This analysis indicated that a total of 282 participants would be needed to detect a significant group × time interaction.
Results
Of the 294 active duty U.S. Marines enrolled in the study, 291 (99%) completed both the pretest and posttest.
Table 1 provides participant characteristics. Of the initial sample, 131 Marines (45%) completed the 6-week follow-up assessment. Attrition was not associated with sex or race-ethnicity, but compared with follow-up completers, noncompleters were significantly younger (p=.001) and had a lower rank (p=.02), less education (p=.01), and fewer combat deployments (p=.01).
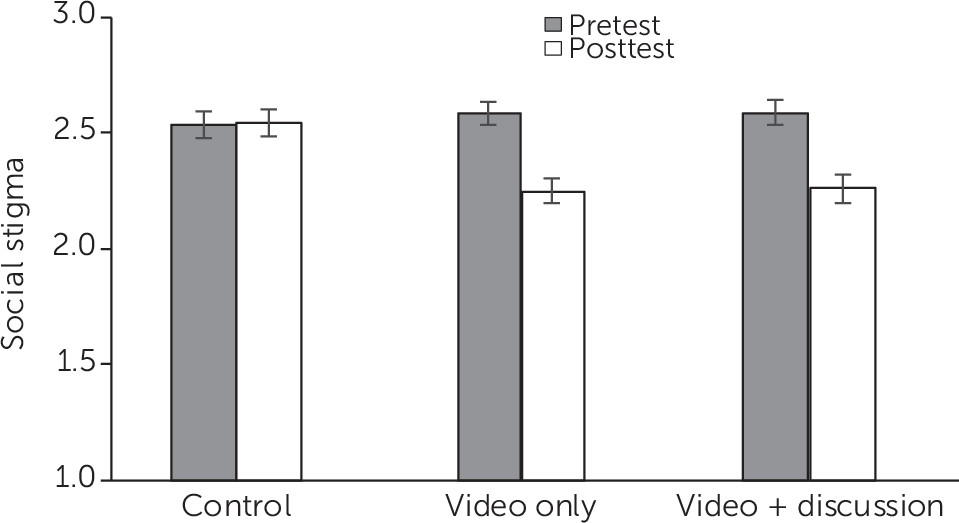
Social Stigma
Although there was no overall effect of condition, perceptions of social stigma decreased from pretest to posttest (mean±SD scores of 2.57±.51 and 2.35±.58, respectively; F=82.23, df=2 and 277, p<.001, η
2=.23). However, the degree of reduction in social stigma differed by condition (F=21.72, df=2 and 277, p<.001, η
2=.14) (
Figure 1). The significant condition × time interaction provides support for the hypothesis that service members who viewed the video would report decreased social stigma compared with a control group. Participants in the control condition showed no change in perceptions of social stigma from pretest to posttest (2.53±.54 and 2.54±.54, respectively). In contrast, perceptions of social stigma decreased significantly among both participants in the video-only condition (2.59±.49 and 2.25±.55; F=46.93, df=1 and 94, p<.001, η
2=.33) and the video-plus-discussion condition (2.59±.49 and 2.26±.61; F=51.77, df=1 and 93, p<.001, η
2=.36).
A comparison that focused only on the video-only and the video-plus-discussion intervention groups revealed no significant difference between the groups in reduction of social stigma; the significant effect of time was replicated (F=98.27, df=1 and 187, p<.001, η2=.34), whereas the interaction of condition and time was not significant, indicating a lack of support for the hypothesis that the addition of a pre- and postviewing discussion would increase the effectiveness of the video in reducing social stigma. A mixed-model ANOVA including data at follow-up showed that improvements in social stigma among the video-only and the video-plus-discussion groups did not persist at follow-up.
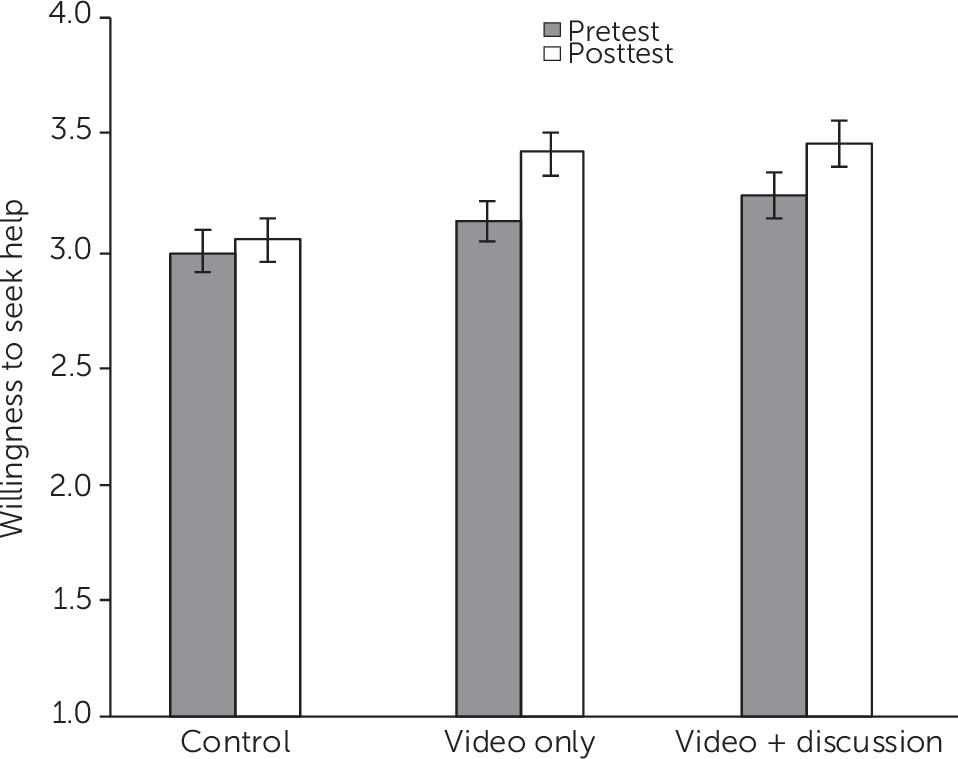
Willingness to Seek Help
Mean scores for willingness to seek help increased from pretest (3.11±.90) to posttest (3.30±.94) (F=28.30, df=1 and 277, p<.001, η
2=.09). Additionally, there was a significant effect of condition, such that participants in the control condition (3.01±.86) reported the lowest willingness to seek help, followed by the video-only condition (3.26±.80) and the video-plus-discussion condition (3.34±.91) (F=3.64, df=2 and 277, p=.03, η
2=.03). These main effects were qualified by the significant interaction of time and condition, the result of most interest (F=3.90, df=2 and 277, p=.02, η
2=.03) (
Figure 2). In the control condition, willingness to seek help did not differ from pretest (2.98±.90) to posttest (3.04±.89). In contrast, Marines in both the video-only and video-plus-discussion conditions were more willing to seek help at posttest than at pretest (3.41±.89 versus 3.11±.84, F=11.33, df=1 and 93, p=.001, η
2=.11 [video only]; 3.45±1.00 versus 3.23±.94, F=19.71, df=1 and 94, p<.001, η
2=.17 [video plus discussion]), providing support for the hypothesis that those who viewed the video would report increased willingness to seek help compared with the control group.
In a direct comparison of the two intervention groups, the significant effect of time on willingness to seek help was replicated (F=30.57, df=1 and 187, p<.001, η2=.14). The interaction of condition and time of measurement, however, was not replicated, indicating there were no significant differences between the interventions in the effect on willingness to seek help. Mixed-model ANOVAs of willingness to seek help at follow-up showed that improvements did not persist over time and that there was an unexpected increase in willingness to seek help among participants in the control condition (p=.01).
Personal Desire for Mental Health Care
At baseline, 33% (N=93) of all participants reported a personal desire for mental health care. To determine whether the intervention would significantly increase Marines’ personal desire for mental health care, two logistic regression analyses examined the effects of study condition on the proportion of Marines who reported wanting help for mental health issues at the 6-week follow-up, controlling for baseline personal desire for mental health care. Results of the first analysis showed that after the analyses controlled for baseline personal desire for mental health care, those in the intervention conditions (combined) were 2.56 times more likely than those in the control condition to report a personal desire for mental health care at follow-up (45% versus 24%, B=.94, 95% confidence interval [CI]=.00 to 1.88, χ2=3.83, df=1, p=.05). A second analysis tested the hypothesis that the addition of a pre- and postviewing discussion would increase personal desire for mental health care, while controlling for baseline desire for mental health care. No significant difference between the two intervention conditions was found.
Discussion
This study evaluated the effects of a video developed to reduce social stigma among active duty Marines by demystifying the treatment process and options available to service members. The study expands upon previous research regarding the effectiveness of a stigma-reduction toolkit (
20) by evaluating use of the toolkit’s video as an independent component and with an in-person discussion led by a mental health professional. Results indicated that both intervention conditions improved social stigma and willingness to seek help at posttest, but findings at follow-up were less clear. Nevertheless, the intervention was successful in increasing personal desire for mental health care at the 6-week follow-up. There were no statistically significant differences between the video-only and video-plus-discussion conditions on outcomes.
This research adds to the literature regarding the comparative efficacy of video-based interventions, which is both somewhat mixed and somewhat limited in military populations (
26–
28). The finding that social stigma was reduced for only a short period after the video was shown is consistent with findings from prior interventions, including those that used videos (
29,
30). Contrary to our hypotheses, adding a discussion period did not improve social stigma or willingness to seek help beyond merely watching the video. However, additional study results indicated that service members in the video-plus-discussion group were more likely than those in the video-only condition to share what they learned with other service members, which may help reduce social stigma (
31). Thus there may be a benefit to including a discussion along with the video, but more research is needed. Nonetheless, this type of video may be effective as an initial stand-alone social stigma reduction intervention. For example, military units could use the video in small group discussions about mental health, video segments could be aired on basewide television broadcasts, and the video could be played in primary care or pharmacy waiting rooms in medical treatment facilities.
Although study results showed immediate improvements in intervention participants’ social stigma and willingness to seek help, these effects did not persist over time. The lack of sustained effects on social stigma, which is consistent with previous research (
29,
30), suggests that one-time stigma-reduction interventions may be insufficient to inspire long-term changes in attitudes. Participants may benefit from repeated exposure to intervention material or booster sessions over time to reinforce content. Furthermore, we saw an unexpected significant increase at follow-up in willingness to seek help among participants in the control condition, which may have occurred because of unknown external circumstances or as a result of contamination across study groups.
Notably, while the changes in social stigma and willingness to seek help did not persist at follow-up, the increase in the personal desire for mental health care among the two intervention groups was significant at the 6-week follow-up. Although personal desire for mental health care is not a substitute for actually seeking help, it is possible that by participating in the intervention, participants became more aware of the symptoms of mental disorders and more willing to consider seeking help. Although more research is needed to improve and sustain treatment-seeking behavior, this finding may highlight a change in participants’ cognizance of their own mental health needs.
Though promising, the results of this study must be interpreted with caution because of several limitations. First, although self-reports are an effective manner to measure intentions and attitudes regarding mental health care in this setting, common biases in self-reporting, such as social desirability, must be considered (
32). Second, increases in willingness to seek care and personal desire for mental health care may not translate to changes in help-seeking behavior. Nonetheless, we believe that help-seeking behavior does not occur without intention, and thus any improvements in willingness or intention to seek care are meaningful. Third, attrition neared 50%, which may have caused the study to be underpowered for detecting changes at follow-up and reduced generalizability of the results. Fourth, the video was originally designed to highlight treatment for posttraumatic stress among infantry Marines and thus may have been perceived as less relevant for other groups. Future research could broaden the applicability of the video to other groups (e.g., female Marines, noninfantry units), and psychological issues (e.g., depression, anxiety).
Conclusions
This study tested a novel approach to reducing social stigma toward mental health treatment among Marines. The results showed that a stigma-reduction video in which mental health care providers explain the mental health care treatment process can decrease social stigma, affect willingness to seek help for mental health concerns, and increase personal desire for mental health care. The results are particularly promising given that the video had an immediate impact regardless of whether it was accompanied by a live discussion. Future research is needed to assess how this shift can be maintained over time and how personal desire for mental health care can be converted to help-seeking behavior. In addition, future studies should develop and assess an updated video that emphasizes other mental health conditions common for this population, including anxiety, depression, and substance abuse, and that focuses on a more diverse target population, including female Marines, noninfantry Marines, those who have not deployed, and leadership. Nonetheless, the intervention video is useful as a starting point in the battle against social stigma toward mental illness among service members.
Acknowledgments
The authors express their sincere appreciation to all of the Marines who took the time to participate in this study. They also express their gratitude to Isabel V. Altarejos, Renee G. Dell’Acqua, and Anne Hickey for their invaluable assistance in this study.