Effective surveillance systems are the cornerstone of public health because they inform the development of prevention strategies and evaluate their impact. Suicide is no exception. Enhancing surveillance of suicide mortality is widely recognized as a priority to help curb rising rates of suicide among veterans and other vulnerable populations (
1). Since implementing a national veteran suicide prevention program in 2007, the U.S. Department of Veterans Affairs (VA) has embraced this priority (
2,
3). Specifically, in 2010, VA researchers established the State Mortality Project and obtained death certificate records for all suicide decedents directly from participating states (
4). A complex validation process was used to identify veteran suicide decedents in this database (
4). In 2012, to ensure national surveillance coverage for both veterans and active duty military service members and to improve the timeliness, efficiency, and accuracy of such efforts, the VA and U.S. Department of Defense (DoD) collaborated to establish a joint data archive and information sharing mechanism known collectively as the VA-DoD Mortality Data Repository (MDR). With the establishment of the MDR, the State Mortality Project was discontinued. The MDR captures all-cause mortality data obtained from the National Death Index (NDI) (
5). Each year, the VA Office of Mental Health and Suicide Prevention and the DoD Defense Suicide Prevention Office jointly compile a search list that includes veterans, nonveteran Veterans Health Administration (VHA) users, and active duty military service members to submit to the Centers for Disease Control and Prevention’s NDI database. Using this comprehensive data source, the VA regularly publishes suicide data reports and state-specific figures (
6,
7).
Prior to full implementation of the MDR, data from 23 states participating in the State Mortality Project were used to estimate suicide rates (2000–2010) among all veterans as compared with suicide rates among U.S. adult nonveterans. Data were also used to compare suicide rates between male and female veterans and between veterans who did and did not use VHA services prior to death (
4). Previously, information on veteran suicide rates was primarily limited to VHA patient populations (
8), although some efforts had been made to indirectly identify and compare suicide rates among veterans who used VHA services and veterans who did not (
9). Findings from the 23-state analysis were striking: in 2010, the suicide rate among all veterans was estimated to be 60% higher than that observed for adult nonveterans, and the suicide rate among female veterans was estimated to be nearly six times higher than that of female nonveterans (
4). National VA reports using MDR NDI data have similarly found higher suicide rates among veterans than among nonveterans, but estimates differ from the State Mortality Project’s figures. According to MDR data, in 2014, veterans were approximately 22% more likely than nonveterans to die by suicide (
10). The national MDR analysis also found that the suicide rate among female veterans was approximately 2.5 times higher in 2014 than that for female nonveterans (
10). Given these pronounced differences, MDR data were used to directly replicate the State Mortality Project’s 23-state analysis (
4). This Brief Report investigates the reasons for the observed discrepancies and discusses findings in the broader context of enhancing veteran suicide surveillance.
Methods
In 2019, we replicated the statistical methods from Hoffmire et al. (
4), using NDI data from the MDR for the same 23 states and years of death (2000–2010) examined in the State Mortality Project analysis. The 23 states analyzed were Alabama, Alaska, Arkansas, Florida, Idaho, Iowa, Kansas, Louisiana, Michigan, Minnesota, Montana, Nebraska, New Jersey, New York, North Carolina, Oregon, Pennsylvania, Rhode Island, Tennessee, Texas, Utah, Washington, and West Virginia. Suicides were identified by using
ICD-10 codes X60–X84 and Y87.0. Crude and direct age-adjusted suicide rates (per 100,000 population members) were computed for veterans and nonveterans overall, by gender, and by VHA service utilization history. VHA users were defined as veterans who had used health care services provided or paid for by the VA in the year prior to death. Standardized mortality ratios (SMRs) were computed to compare veterans with nonveterans overall and by gender and to compare veterans who did and did not use VHA services (
11). Findings were compared with those from the State Mortality Project. Inquiries were made to assess for systematic errors in the State Mortality Project veteran validation process that could explain discrepancies observed between the two data sources. This work was conducted as an operational analysis for the VA Office of Mental Health and Suicide Prevention.
Results
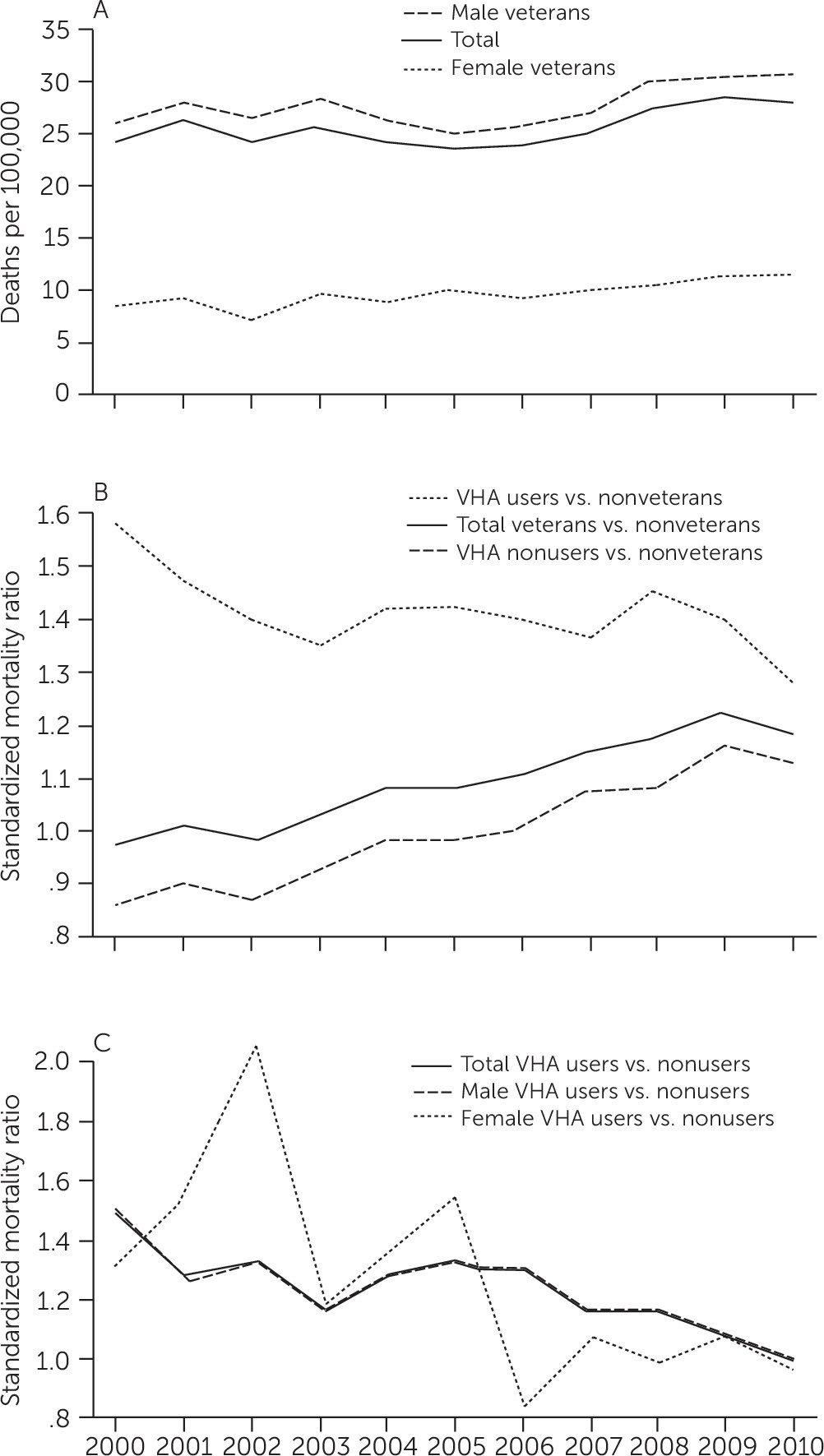
Data on 32,516 suicides among veterans (31,623 males, 893 females) captured in the MDR from 2000 through 2010 were analyzed. The crude suicide rate for all veterans increased from 21.6 deaths per 100,000 veterans in 2000 to 27.4 deaths per 100,000 veterans in 2010. These rates were lower than analogous figures observed in the State Mortality Project analysis (28.6 deaths and 35.9 deaths per 100,000 veterans, respectively) (
4). Differences were more pronounced for female veterans: for 2010, a suicide rate of 12.4 deaths per 100,000 female veterans was estimated in the current MDR analysis (
Figure 1A), compared with a rate of 34.6 deaths per 100,000 estimated by using the State Mortality Project database (
4).
Figure 1 presents trends in direct age-adjusted suicide rates for veterans throughout the study period as well as SMRs for veterans compared with nonveterans and for veterans who used VHA services compared with veterans who did not. Differences in suicide rates and SMRs from the two data sources can be seen by comparing this figure with Figure 1 and Figure 2 reported by Hoffmire et al. (
4). Notably, in 2000, the suicide rate among VHA users was nearly 60% higher than that of adult nonveterans, whereas the suicide rate among VHA nonusers was approximately 15% lower than that of adult nonveterans (
Figure 1B). However, opposite SMR trends experienced by VHA users and nonusers resulted in converging SMR estimates for the two groups; by 2010, suicide rates were 30% and 15% higher than the rate for adult nonveterans among VHA users and nonusers, respectively.
Results for nonveterans were relatively consistent between the two databases (data not shown). As such, the lower suicide rates for veterans estimated by using MDR data (
Figure 1A) resulted in reduced SMR estimates comparing veterans with nonveterans (Figure 1B). Using 2010 data from the MDR, we estimated that veterans had a suicide rate approximately 20% higher than that of their nonveteran peers, compared with the 60% higher rate observed with the State Mortality Project database (
4). Differences were also observed between the two databases when comparing female veterans who used VHA services and female veterans who did not (
Figure 1C). Prior results from the State Mortality Project indicated that in 2000, female veterans who used VHA services had lower suicide rates (SMR=0.2) than female veterans who did not (
4). Conversely, data from the MDR showed that in 2000, similar to male veterans, female veterans who used VHA services were at elevated risk for suicide (SMR=1.3) compared with female veterans who did not. By 2010, however, analysis using data from the MDR did not result in significant differences in suicide rates on the basis of VHA utilization for either males or females.
Review of these findings prompted a reassessment of the processes used to identify veterans in the State Mortality Project database. Of note, the increased number of veteran suicide decedents identified in the State Mortality Project database was primarily limited to suicide decedents without a history of VHA use in the year prior to death. Most veterans who did not use VHA services in the State Mortality Project database were identified by using the VA-DoD Identity Repository (VADIR) or, for older veterans, by relying on death certificates to ascertain whether an individual served in the military. Thus, the State Mortality Project database was resubmitted to VADIR to confirm the veteran status of those identified. Upon resubmission, some decedents initially identified as veterans were reclassified as nonveterans. Although it is unknown why those individuals were initially classified as veterans in the VADIR system, they were likely dependents (e.g., a spouse) of a veteran who received VA benefits or were eligible for an entitlement from the VA. This finding confirmed that the data linkage and resulting process used to identify veterans in the State Mortality Project misclassified veteran status for some suicide decedents and overestimated suicide rates among veterans, specifically among those without a history of VHA service use.
Discussion
Suicide rates computed from NDI data contained in the VA-DoD MDR differed from those previously estimated with death certificate data obtained directly from states participating in the VA’s State Mortality Project (
4). The MDR findings, which used data from the same 23 states, were in line with national MDR estimates (
6,
10). The State Mortality Project database and the MDR are two related but distinct data sources. To increase the number of older veterans identified and included in the database, the State Mortality Project used death certificates to ascertain whether an individual served in the military (
4). However, greater inclusion of older veterans did not explain differences in findings between the data sources. The State Mortality Project did not achieve national coverage and relied on a complex validation process to identify veteran suicide decedents. This validation process resulted in misclassification of veteran status, with some nonveterans identified as having a history of military service. Most of these individuals were likely nonveteran dependents of veterans or of active duty service members. This misclassification disproportionally affected females and may explain much of the difference observed between data sources.
In 2012, Miller et al. (
12) published “A Call to Link Data to Answer Pressing Questions About Suicide Risk Among Veterans,” which discussed the difficulty of tracking veteran suicide rates using the National Violent Death Reporting System (NVDRS) (
13). The article claimed that the system, which combines participating states’ death certificate records with other data sources, was unable to accurately identify veterans from state records without linkage to DoD records. The State Mortality Project aimed to improve identification of veteran suicide decedents from state death certificate records but faced challenges in validating veteran status, particularly among older adults. Questions about the reliability of veteran identifiers in the NVDRS remain. The MDR, however, has substantially improved the VA’s ability to accurately identify suicide decedents and track suicide rates for the veteran population as a whole and within key high-risk subpopulations.
Findings from this comparative analysis highlight the importance of accurately identifying veteran status to track suicide rates within smaller high-risk populations (i.e., female veterans) because the rates for such populations are greatly affected by small differences in suicide counts. The lessons learned from this analysis can be generalized beyond veteran suicide surveillance, however. More broadly, this study provides a pertinent example of how conditions with low base rates (i.e., “rare events”) can be major public health problems; how minor misclassification can have a large impact on the success of surveillance, prevention efforts, and the validity of study findings; and how challenging disease or mortality surveillance can be when attempting to track events across hard-to-define or transient populations. Maternal suicide is a similar, relevant example. Inconsistencies in documentation, definitions, and methods to identify the “maternal” population (i.e., pregnant or postpartum women) pose a significant challenge to accurate suicide surveillance in this population as well. Recent enhancements to maternal mortality surveillance include state-based maternal mortality review committees, which, similar to the enhanced veteran mortality surveillance efforts described in this study, aim in part to improve accuracy and timeliness of maternal suicide surveillance.
Conclusions
Continued efforts to maintain and improve the VA-DoD MDR will be paramount to ensuring the VA’s suicide prevention program is successful. Accordingly, the recently released report “National Strategy for Preventing Veteran Suicide” (
1) emphasizes a public health approach to suicide prevention and sets a goal to “increase the timeliness and usefulness of national surveillance systems relevant to preventing veteran suicide and improve the ability to collect, analyze, and use this information for action.” The MDR can and should continue to be enhanced to help meet this goal. For example, linking MDR data to other national data sources such as the NVDRS can further refine veteran suicide surveillance efforts by enhancing knowledge on clinical and circumstantial factors that may increase risk for suicide among U.S. veterans not using VHA services. Such findings can help to tailor veteran suicide prevention programs and target subpopulations at greatest risk.