The emergency department (ED) is an important component of the mental health care system, acting as the gateway between outpatient and inpatient care in most settings (
1). In the United States and other high-income countries, mental illness and addictions are the primary presenting issues for up to one in 10 adult ED visits (
2). Whether individuals present voluntarily because of subjective distress or involuntarily (e.g., with police escort) because of acute risk, psychiatric ED visits suggest an urgent need for care. Most psychiatric ED visits do not result in hospital admission (
3), yet mental health–related crises cannot usually be managed in a single visit. Urgent outpatient mental health care is crucial for ongoing assessment and management and for preventing repeat visits to the ED and other negative outcomes.
Existing research on post-ED follow-up has been inconsistent across jurisdictions, and most research focuses only on certain diagnoses. A U.S. Medicaid study found that about 67% of individuals received follow-up care within 7 days after a psychiatric ED visit. There were similar follow-up rates for those with and without substance use disorders (
4). However, a U.S. health maintenance organization (HMO) study focused on substance use presentations found that only 13% received addictions care within 14 days of ED discharge (
5). Another U.S. Medicaid study found that 52% of patients presenting with self-harm received follow-up within 30 days after being discharged from the ED (
6). In contrast, a Canadian population-based study found that only 31% of similarly presenting individuals received follow-up within 30 days (
7).
This study aimed to measure the likelihood of outpatient follow-up with a physician for mental health care in the 14 days after discharge from the ED among all adults who visited an ED for a psychiatric reason in Ontario, Canada, from 2010 to 2012 and who were not hospitalized as a result of that visit. The study also compared the likelihood of follow-up across specific types of psychiatric ED presentations.
Methods
This cohort study used population-level data from Ontario, Canada’s most populated province (population approximately 14 million), between 2010 and 2012. Ontario’s government-funded health insurance covers both physician-delivered and hospital-based mental health care for all residents. We accessed de-identified Ontario health administrative data at ICES, an independent nonprofit health research institute. (A table showing data sources is available as Appendix A in the online supplement.) These data sets were linked by using unique encoded identifiers and analyzed at ICES.
The cohort comprised all Ontario residents ages 19 and over who presented to an ED with a primary psychiatric issue and who were not admitted to the hospital directly after the ED visit (April 1, 2010-March 31, 2012). Primary psychiatric issues constituted either a psychiatric diagnosis as the main diagnosis on the ED record (
ICD-10-
CA codes F00–F99) or intentional self-harm coded in any diagnostic field (X60–X84, Y10–Y19, Y28) (
8). To investigate specific presentation types, participants were classified based on their primary presentation into two groups: those with a substance use disorder and those with a mental disorder other than a substance use disorder, using the primary diagnosis at the index ED visit. From among individuals whose primary presentation was a mental disorder that was not related to substance use, we further identified those presenting with primary diagnoses of schizophrenia, bipolar disorder, and major depressive disorder. A person’s first ED visit during the study period was considered the index visit (individuals could contribute only one visit). Those with a repeat psychiatric ED visit, hospitalization, or death within 14 days of the index visit were excluded because there was insufficient time for follow-up to occur after the ED visit. Persons registered in community health centers (CHCs) were excluded because of incomplete outcome data (CHC physician care is not captured in the Ontario Health Insurance Plan database).
The primary outcome was any outpatient follow-up with a physician (primary care provider or psychiatrist) for mental health care within 14 days of the index ED visit. Fourteen days is a pragmatic time frame because it represents the typical follow-up timeline in urgent psychiatric care programs (
9). A validated algorithm was used to identify follow-up visits to a primary care provider for mental health care (
10). Specialist codes were used to identify psychiatrist visits. The variables used to describe the sample were age, sex, rural residence, neighborhood income quintile (derived from the postal code), medical comorbidity (Johns Hopkins adjusted clinical grouping count of major diagnostic groups; higher scores indicate greater comorbidity [
11]), primary care enrollment type, and previous health service utilization (outpatient care, psychiatric ED visits, and psychiatric admissions).
We measured the proportion of individuals with any follow-up visit, a follow-up visit to a primary care provider only, and follow-up care with a psychiatrist (with or without primary care). The proportion of individuals receiving follow-up care was then compared between those with and those without substance use disorders and across major mental illness categories by using chi-square tests of association. We did not adjust comparisons for covariates because the crude rates provide the key data for researchers, policymakers, and clinicians looking to improve post-ED follow-up. Analyses were conducted by using SAS software, version 9.4 and University Edition (SAS Institute, Cary, NC).
Data use was authorized under section 45 of Ontario’s Personal Health Information Protection Act and was exempt from research ethics board review.
Results
There were 143,662 individuals with an index psychiatric ED visit, including 31,592 (22.0%) presenting with substance use disorders and 112,070 (78.0%) whose primary presentation was not a substance use disorder. (A figure outlining the cohort and groups is available as Appendix B in the online supplement). The latter group included 4,765 (3.3%) with schizophrenia, 2,222 (1.5%) with bipolar disorder, and 17,643 (12.3%) with major depressive disorder. (A table displaying the characteristics of the overall sample and for each group is available as Appendix C in the online supplement.)
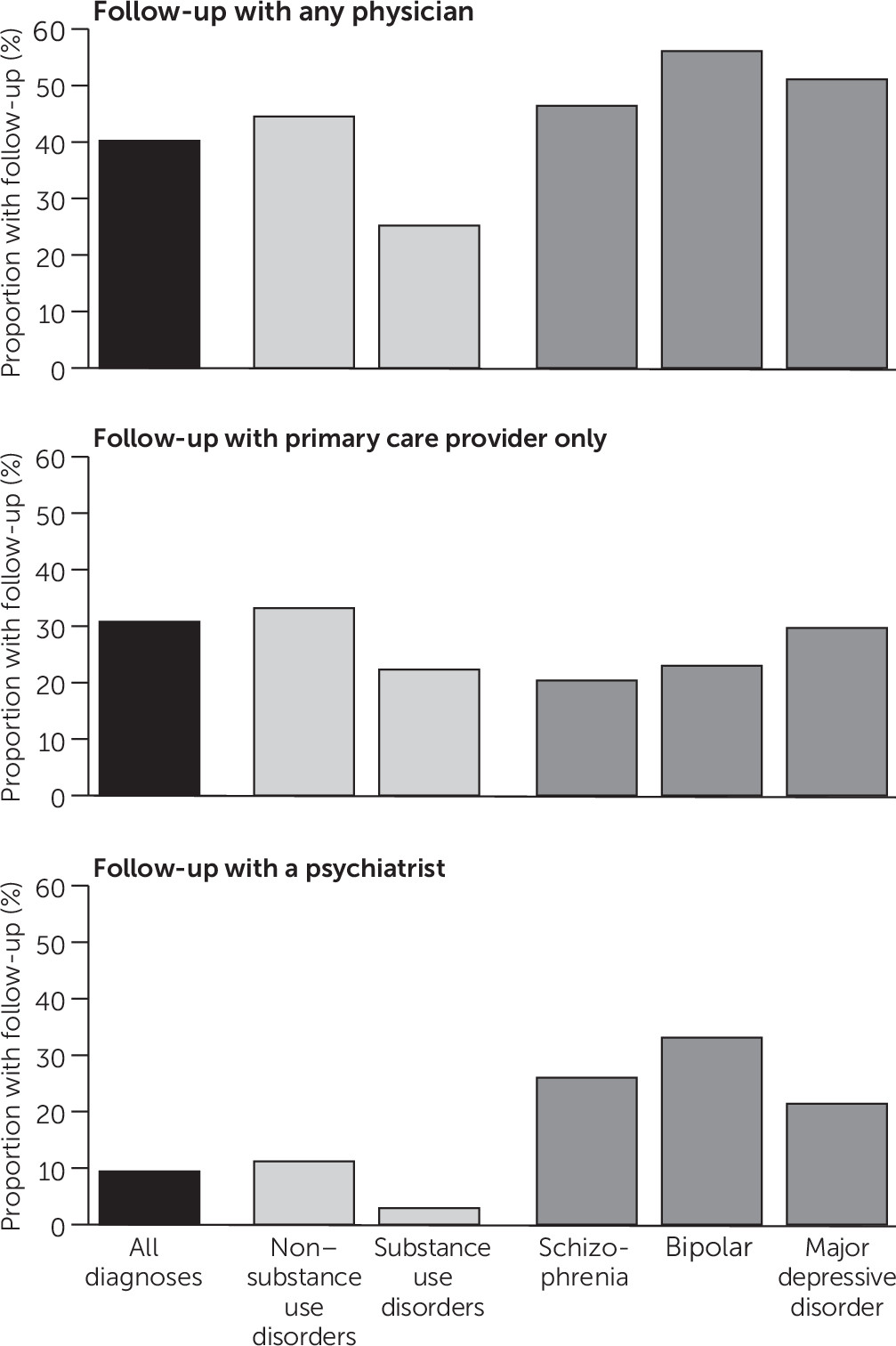
About 40.2% (N=57,797) of the cohort had a follow-up visit with any physician for mental health care within 14 days of ED discharge (
Figure 1). Those presenting with substance use disorders (N=7,974, 25.2%) were much less likely to have a follow-up visit than those who did not present with substance use disorders (N=49,823, 44.5%) (χ
2=3,784.7, df=1, p<0.001). The likelihood of follow-up differed significantly across the three major psychiatric diagnosis types: schizophrenia (N=2,212, 46.4%), bipolar disorder (N=1,246, 56.1%), and major depressive disorder (N=9,017, 51.1%) (χ
2=61.7, df=2, p<0.001).
Primary care was the only form of mental health follow-up with a physician for 30.8% of the cohort (N=44,306) (
Figure 1). The primary care follow-up rate was lower among those presenting with versus without substance use disorders (N=23,618, 22.3%, versus N=62,247, 33.2%) (χ
2=1,380.8, df=1, p<0.001). About 29.7% of those with major depressive disorder had primary care follow-up only (N=5,243), with lower rates among those with bipolar disorder (N=511, 23.0%) and schizophrenia (N=974, 20.4%) (χ
2=185.6, df=2, p<0.001).
Only 9.4% (N=1,341) had a follow-up with a psychiatrist within 14 days (
Figure 1), with a substantially lower likelihood of follow-up by those with versus without substance use disorders (2.9% versus 11.2%) (χ
2=1,987.9, df=1, p<0.001). Psychiatrist visits occurred for 33.1% (N=735) of those with bipolar disorder, a higher rate than that for individuals with schizophrenia (N=1,239, 26.0%) and major depressive disorder (N=3,774, 21.4%) (χ
2=173.2, df=2, p<0.001).
Discussion
In a population-based cohort of 143,662 adults with psychiatric ED visits, fewer than half had a physician follow-up visit within 14 days of the ED visit for outpatient mental health care. Fewer than one in 10 had a psychiatrist follow-up visit. ED visits related to substance use represented more than one fifth of the total ED presentations (22%), and only one in four received any follow-up care in the 14-day follow-up period (and only approximately 3% received follow-up care from a psychiatrist). Rates of follow-up with a psychiatrist were also low among those with the serious mental disorders of schizophrenia and bipolar disorder, where about one in four and one in three received follow-up, respectively. These rates are concerning, given the high levels of distress and (often) risks associated with psychiatric ED visits and the importance of care continuity for this population.
To our knowledge, this is the first study to examine post-ED follow-up in a population-based study across a range of diagnoses and capture mental health follow-up by all physicians (not just from certain hospitals or insurance plans). For those with substance use disorders in our sample, only 25.2% had physician follow-up within 14 days. These rates are higher than in U.S. HMO data (13% within 14 days) but much lower than those reported in U.S. Medicaid populations (66.6% within 7 days), although the latter included mental health follow-up with all “providers,” presumably also including nonphysician professionals (
4,
5). Our study’s rates for substance use disorders are consistent with research on frequent ED visitors in Ontario, where substance use presentations are associated with remarkably low physician follow-up rates (
12). For those presenting with a disorder other than a substance use disorder, 44.5% had follow-up within 14 days. This rate, although lower than that in the Medicaid data mentioned earlier, is generally aligned with data from other U.S. and Canadian studies of 30-day follow-ups after ED presentations for self-harm (52.4% and 31.4%, respectively) (
4,
6,
7).
In a single-payer system such as Canada’s, where physician visits are publicly funded, low follow-up rates are unlikely because of individual-level differences in insurance status or out-of-pocket costs. Instead, system-level factors likely limit access to timely and appropriate follow-up care. In Ontario, ambulatory mental health services are delivered by a range of independently operating clinics, providers, and hospitals with no single point of accountability. Although there is a limited supply of psychiatrists in certain rural areas, urban psychiatrists tend to see a lower number of patients than their rurally practicing counterparts and see their patients more frequently and for longer durations, leading to low availability for new patients (
13).
Although our data capture service use for the entire jurisdiction, there are some limitations to this report. The data sets do not include nonphysician mental health care, and relevant follow-up may have occurred with other providers. Because physician follow-up is key to many aspects of mental health and addictions care, including risk assessment and pharmacological management, we believe that it is reasonable to ensure that individuals presenting in crisis to an ED have physician follow-up, even if they are also seeing other health care professionals. We did not have the acuity level of the ED visit and, therefore, were unable to determine whether follow-up rates differed by acuity level. However, the cohort included only those well enough to be discharged from the ED. Finally, the data for this study were collected between 2010 and 2012; however, as there have been no major changes to the Ontario mental health care system since that time, our results are likely representative of current mental health care utilization.
Conclusions
The gaps that we observed in mental health care continuity in Ontario highlight the need for systemwide and coordinated solutions to successfully transition patients to from the ED to outpatient care. Ultimately, physicians alone are unlikely to be able to adequately care for patients with these acute and complex conditions without coordinated and well-resourced interprofessional teams with case management support (
14). In particular, for those presenting with substance use disorders, for whom there may only be a short window of motivation to seek care and a similarly short window before rapid deterioration occurs, provider- and system-level barriers to addictions care (e.g., difficult-to-navigate referral pathways [
15]) warrant careful attention.
Acknowledgments
The authors thank Rick Glazier, who provided valuable input to the design of the cohort.