It has been estimated that 2%−3% of hospitalized patients fall in the United States each year, increasing their likelihood of fall-related injuries, such as hip fractures (
1). For health care systems, fall-related injuries can lead to longer hospital stays, additional care needs, increased health care costs, and reduced reimbursement (
2–
4). For patients and families, falls can impair quality of life through anxiety and distress, fear of falling, and restricted mobility (
5,
6). Studies (
1,
7) have shown that fall rates in countries such as the United States and United Kingdom range from three to five falls per 1,000 patient-days; however, certain unit types, such as psychiatric units, may have higher rates because of differing patient risk factors (
7–
13).
Adult patients in psychiatric care may be at increased risk for falling and sustaining a fall-related injury compared with other inpatients. Psychiatric conditions, such as depression, psychosis, and schizophrenia, can increase fall risk (
14–
24). Similarly, psychotropic medications may increase fall risk (e.g., because of balance problems, confusion, and vision changes) (
17,
25–
33). The impact of medication on falls may be amplified when a patient’s medication regimen is changed or includes multiple medications (
28,
34,
35). Other clinical conditions, including neurological disorders and gait, balance, and visual deficits, have been shown (
14,
34,
36–
38) to be associated with fall risk among inpatients receiving psychiatric care. Despite the risk factors for falls among psychiatric inpatients, few studies have estimated how many falls occur in psychiatric care settings.
Most studies (
39–
42) that have estimated in-hospital fall rates have focused on general acute care rather than on psychiatric units. The few studies that have examined falls in psychiatric units have focused on geriatric patients. In the United Kingdom (
7), the median fall rate for adults older than age 65 in psychiatric care in 2012 was 13.9 falls per 1,000 patient-days, compared with 6.8 per 1,000 for similar aged patients in acute care hospitals. Estimates of falls in geriatric psychiatric units from other countries (
10–
12) have varied considerably (e.g., 1.25 falls per 1,000 patient-days in Australia in 2012). Few studies have estimated the rate of injurious falls. The U.K.-based study (
7) reported that the median injurious fall rate was 5.5 per 1,000 patient-days in psychiatric care units, compared with 2.5 per 1,000 patient-days in acute care units. Many of the other studies (
9,
13,
37,
43) estimating fall rates in psychiatric care settings, including U.S.-based studies, are more than a decade old.
In addition to the lack of recent estimates, few studies (
40,
44) of inpatient falls have distinguished between falls that occur when a staff member intervenes to slow the patient’s descent (i.e., assisted) and those that occur without such assistance (i.e., unassisted). Studies (
40,
44) have shown that unassisted falls result in a higher rate of injury. Unassisted falls have also been associated with certain processes of care. For example, falls are more likely to be unassisted when a fall prevention protocol has not been put in place (
40,
44). Therefore, unassisted falls should be included in estimates of falls and fall-related injuries to provide a signal of whether additional fall prevention interventions may be needed. To our knowledge, there have been no studies estimating how many falls occur with assistance in psychiatric care settings.
To address this research gap, we aimed to estimate the incidence of falls (total, injurious, and assisted) in U.S. psychiatric care settings and to examine whether the rate of assisted falls was associated with injurious falls. Additionally, we examined trends in total and injurious fall rates for psychiatric care settings across a 6-year period (April 2013–March 2019). By addressing this research gap, our goal was to help provide evidence on the extent to which hospital falls are a problem in psychiatric care, which can inform decisions about whether interventions need to be developed to address falls among patients on psychiatric care units.
Methods
Data
The National Database of Nursing Quality Indicators (NDNQI) began collecting falls data from inpatient units in 1998 and expanded falls data collection to psychiatric units in 2013 (
45). Roughly 2,000 hospitals participate in the NDNQI by collecting and submitting data on quality and/or safety measures for units of their choosing. Hospitals report monthly falls data to the NDNQI for each participating psychiatric unit.
These data include the unit’s total patient-days for the month, the total number of patient falls, and the injury level for each fall. Injury levels—none, minor, moderate, major, and death—are assigned by nursing staff on the basis of NDNQI definitions. Bruises and abrasions are examples of minor injuries. Joint and/or muscle strain and injuries requiring skin glue or sutures are classified as moderate. Major injuries include fractures and injuries requiring surgery, traction, or consultation for neurological or internal injury.
In addition, hospitals report whether each fall qualifies as an assisted fall, defined as a fall where a staff member tried to slow the patient’s descent and thereby lessen the fall’s impact. The NDNQI fall definition excludes intentional fall events, which hospitals have the option of tracking and reporting separately (
45). Because data on falls are considered a limited data set, as defined by Health Insurance Portability and Accountability Act (HIPAA) guidelines, the NDNQI collects only limited patient-level data on patients experiencing a fall. General medical data (e.g., diagnosis, medications, comorbidities) are not collected. The institutional review board at the University of Kansas Medical Center, whose School of Nursing coordinates research involving NDNQI data, ruled that our secondary analyses of NDNQI data did not constitute human subjects research.
Sample
We studied NDNQI fall data from inpatient psychiatric units for the 6 years from April 2013 through March 2019. We limited analysis to adult and geriatric psychiatric units in general, acute care hospitals, and psychiatric hospitals located in the United States. The final sample included 1,159 units in 720 hospitals.
Analyses
We calculated the total number of falls, injurious falls, and falls at each level of injury reported by sample units during the 6 years of the study. We computed study-wide rates of falls by dividing fall counts by the total number of patient-days reported and then multiplying the result by 1,000 to yield the rate of falls per 1,000 patient-days. We computed fall counts and rates for each of the four types of units: adult psychiatric units in general hospitals, adult units in psychiatric hospitals, geriatric psychiatric units in general hospitals, and geriatric units in psychiatric hospitals. We also computed the percentage of assisted falls by unit type.
In further analyses, we computed quarterly fall rates for each unit by aggregating each unit’s monthly data. We calculated each unit’s total fall rate for each quarter by dividing its total falls during the quarter by its total number of patient-days for the quarter and multiplying by 1,000. We computed quarterly rates of injurious falls per 1,000 patient-days in the same way.
The median and interquartile range (IQR) of the quarterly fall rates were computed for each of the four types of units. In addition, to test for differences between unit types in average quarterly fall rates, we modeled fall rates as a function of unit type in generalized linear mixed models. The dependent variable in each model was the quarterly unit fall count (total or injurious), which was assumed to have a negative binomial distribution; fall rates were effectively modeled by specifying the log-transformed quarterly unit count of patient-days as an offset. We controlled for hospital characteristics by including hospital teaching status, bed size, ownership, and metropolitan location as additional explanatory variables. Quarter (1, 2, 3, or 4) was included to control for seasonality. To adjust for clustering of quarterly fall rates within units, we specified a first-order autoregressive structure. We performed the modeling in SAS by using the GLIMMIX procedure.
We also examined trends in quarterly total and injurious fall rates across the study period for adult psychiatric units in general hospitals, adult units in psychiatric hospitals, and geriatric psychiatric units in general hospitals. Because there were only 15 geriatric units in psychiatric hospitals in the data set, and even fewer reporting data for specific quarters, we did not examine trends in their quarterly fall rates. In addition to plotting fall rates for each study quarter, we fitted two generalized linear mixed models, one for total falls and one for injurious falls, to estimate time trends. These models were identical to the generalized linear mixed models described above, except that they included a time slope variable for each unit type, which we used to estimate the annual change in fall rate for each unit type.
Finally, two mixed logistic regression models were fitted to examine the effect of a fall being unassisted on the odds of a fall-related injury. First, we modeled odds of any injury (versus no injury) as a function of whether the fall was unassisted (yes or no) and unit type. Second, we modeled odds of moderate-or-worse injury (versus minor or no injury) as a function of these same variables. Each model included a random intercept for unit to adjust for clustering of patients experiencing falls within the unit.
Results
Sample hospitals and units are described in
Table 1. The majority of hospitals were general acute care hospitals (96%), and the majority of units were adult psychiatric units in a general hospital (73%). The median number of patient-days reported by units was 21,146 (IQR=9,104–34,593).
Total and Injurious Fall Rates
Of the 119,246 falls reported, 25,807 (21.6%) resulted in injury. Of these injurious falls, 22,197 (86.0%) resulted in mild injury, 2,338 (9.1%) resulted in moderate injury, 1,258 (4.9%) resulted in major injury, and 14 resulted in death.
As shown in
Tables 2 and
3, total and injurious fall rates were much higher for geriatric psychiatric units than for adult psychiatric units, in both general and psychiatric hospitals. Differences in fall rates between general and psychiatric hospitals were less pronounced, but for a given patient population (adult or geriatric), both falls and injurious falls were more common in general hospitals than in psychiatric hospitals. With adult psychiatric units in general hospitals as a referent, adult psychiatric units in psychiatric hospitals had model-estimated total fall rates 23% (95% confidence interval [CI]=13% to 32%) lower, and injurious fall rates 11% (95% CI=−5% to 23%) lower, when the analyses were controlled for hospital characteristics. Total and injurious fall rates on geriatric psychiatric units in psychiatric hospitals were higher than those on adult psychiatric units in general hospitals by estimated factors of 1.81 (95% CI 1.57 to 2.08) and 2.36 (95% CI=1.96 to 2.83), respectively. These differences were even larger for geriatric psychiatric units in general hospitals, which had estimated total and injurious fall rates 2.34 (95% CI=2.18 to 2.52) and 2.63 (95% CI=2.40 to 2.89) times higher than those for adult psychiatric units in general hospitals.
Assisted and Unassisted Fall Rates
Adult psychiatric units in general and psychiatric hospitals had similar rates of assisted falls (6.6%) (
Tables 2 and
3). Geriatric psychiatric units in general hospitals had higher assisted fall rates compared with geriatric units in psychiatric hospitals (8.3% versus 6.8%). Overall, only 8,435 (7.0%) of the 119,246 falls in the study were reported as having been assisted by a staff member (
Table 4). Injury occurred more frequently with unassisted falls. Our logistic regression models showed that falling unassisted was associated with a higher likelihood of injury (adjusted odds ratio [AOR]=1.69, 95% CI=1.59 to 1.80) and a higher likelihood of moderate or greater injury (AOR=1.56, 95% CI=1.33 to 1.82) (see the
online supplement accompanying this article).
Trends in Total and Injurious Fall Rates
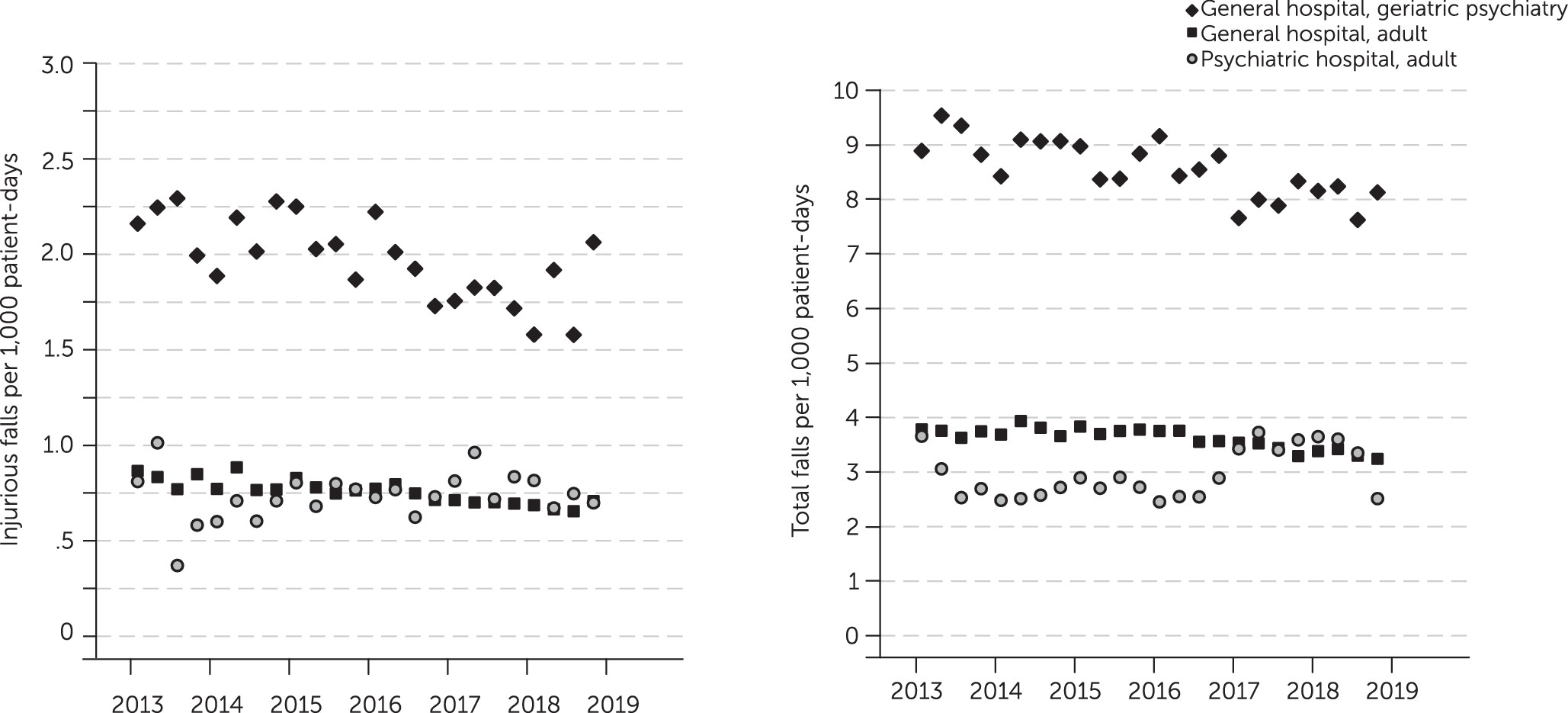
As shown in
Figure 1, we found evidence of meaningful declines in total and injurious fall rates in general hospitals across this 6-year study. According to estimates from the time trend models, total fall rates on adult and geriatric psychiatric units in general hospitals fell by respective averages of 2.1% (95% CI=1.1% to 3.1%, p<0.001) and 3.8% (95% CI=1.9% to 5.7%, p<0.001) per year. Injurious falls for these unit types fell at average rates of 3.7% (95% CI=2.2% to 5.2%, p<0.001) and 4.8% (95% CI=2.0% to 7.5%, p<0.001) per year, respectively. There was no clear time trend in the plots for fall rates on adult units in psychiatric hospitals. According to model estimates, total fall rates fell by an estimated 0.5% (95% CI=−3.4% to 4.2%, p=0.805) per year on average, and injurious fall rates increased by an estimated average of 0.8% (95% CI=−4.8% to 6.7%, p=0.780) per year.
Discussion
The goal of this study was to estimate the incidence of falls of patients in U.S. psychiatric care. This study is the first to our knowledge to provide a recent estimate of fall rates of patients in U.S. psychiatric care and the first to estimate what percentage of falls are slowed by staff (assisted falls). Our study suggests that fall rates in psychiatric units may be similar to those of other unit types (e.g., medical and/or surgical) in the United States (
39). In contrast, the percentage of assisted falls may be substantially lower in psychiatric care compared with other settings (
44). Finally, our study shows that although fall rates for psychiatric units in general hospitals have decreased somewhat, falls remain a serious problem, pointing to the need for additional intervention. We provide implications for research and practice below.
The findings of our study suggest that fall rates in psychiatric care may not be that different from those in other units in acute care hospitals (
39). Our study found that the fall rate in adult psychiatric units in general hospitals was 3.62 per 1,000 patient-days, a rate similar to estimates from U.S. adult medical and/or surgical units of 3.5 per 1,000 patient-days (
39). This finding contrasts with estimates from prior studies from other countries that suggest fall rates are higher in psychiatric care settings (
7). Consistent with prior studies, our research suggests that fall rates are higher in geriatric versus adult psychiatric units (
9,
11,
43). This finding was expected because age and age-related conditions contribute to fall risk (
41,
42,
46). We also found that psychiatric units in general hospitals had higher fall rates than units in psychiatric hospitals. This finding may have been due in part to psychiatric patients in general hospitals having more comorbid conditions (
47).
Our findings suggest that the percentage of assisted falls is lower among psychiatric units compared with other inpatient units. Studies (
44) of other acute inpatient units have estimated that 15% of falls were assisted, compared with our study, in which only 7.0% of falls on psychiatric units were found to be assisted. One potential explanation for this difference is that patients in psychiatric units ambulate more frequently and spend more time outside of their rooms in recreational spaces (
48–
50). One study (
50) reported that spaces with limited visual access and supervision are a key barrier to fall prevention in psychiatric care. Further study is needed to evaluate environmental risk factors for unassisted falls (e.g., visibility, environmental hazards) and their impact on fall injury rates in psychiatric care. Our results indicate that unassisted falls were associated with a higher likelihood of injury (AOR=1.69, 95% CI=1.59 to 1.80).
It is also possible that improving fall prevention practices would increase the likelihood of staff assistance during falls in psychiatric units. Hospitals often put fall prevention protocols in place that increase monitoring of at-risk patients, such as staff assigned to sit with patients (
1). Studies have shown, however, that fall prevention practices are inconsistently implemented in psychiatric care settings. One study (
51) found that practices recommended in the hospital’s fall prevention protocol were underutilized (e.g., signage) in psychiatric units compared with other units. Future studies should examine fall prevention interventions designed for inpatient psychiatric care and test implementation strategies (e.g., audit and feedback) that might improve the quality of implementation.
We found that fall rates for psychiatric units in general hospitals decreased across this 6-year study, but no recent studies examining trends in other U.S. hospital units are available to serve as a comparison. Although these trends in fall rates in general hospitals are encouraging, the scale of the problem remains daunting. In 2018 alone, the 840 units in this study reported 19,242 falls, of which 3,937 (20.5%) were injurious. The trend for fall rates in psychiatric units of psychiatric hospitals was less clear, suggesting that no national initiatives have reduced patient falls in psychiatric hospitals over the past 6 years. One potential explanation for this finding is that national-level policies, such as Medicare’s nonpayment policy for fall-related injury, have largely targeted general hospitals rather than psychiatric facilities (
52). Another potential explanation is the lack of fall prevention interventions designed specifically for psychiatric care.
Unlike other areas of patient safety (e.g., pressure ulcers), the evidence for hospital fall prevention programs is low and has been understudied in psychiatric settings (
53–
58). Studies (
1,
59,
60) suggest that tailored fall prevention programs—or strategies based on patients’ risk factors—may be effective at reducing inpatient falls. Because patients in psychiatric units have unique risk factors, new fall prevention approaches may be needed for this population. For example, psychiatric staff may need to balance the promotion of independent self-care against the need to provide more hands-on assistance to prevent falls. Further study is needed to develop and test fall prevention programs for psychiatric care.
This study had a number of limitations. First, the study sample included only hospitals that participated in the NDNQI. Hospitals participating in NDNQI may differ from hospitals not participating in the NDNQI. Second, this study was intended to estimate the incidence of falls in psychiatric care, rather than to assess patient-, unit-, or hospital-level predictors associated with fall rates. It is possible that changes in patient characteristics over time could explain trends in falls among psychiatric patients. Further studies are needed to evaluate the multilevel risk factors associated with falls in psychiatric care and the impact on fall trends. Future studies could use databases that combine electronic health record and claims data. Finally, U.S. data on falls in psychiatric care started being collected in 2013, and as a result, we could not estimate trends prior to 2013.
Conclusions
Falls are a persistent safety problem in psychiatric care, suggesting further intervention is needed. Future research is needed to test fall prevention interventions in psychiatric care that target multilevel fall risk factors, including those of patients, providers, and environments.