Despite national mental health treatment guidelines emphasizing the importance of shared decision making, patient preferences often play only a limited role in shaping clinicians’ recommendations and informing treatments offered by health care organizations (
1–
3). Individuals with serious mental illness, including schizophrenia, are unlikely to be asked about their preferences, even though research has shown that they frequently wish to receive information about treatment options (
4) and to participate in medical decisions (
5,
6). Improved strategies are needed to facilitate routine, accurate assessment of their preferences.
Many factors are likely to contribute to suboptimal involvement of individuals with schizophrenia in clinical decisions, including brief clinical appointments, which may be dominated by urgent issues; potential belief by providers that their patients have limited decisional capacity, judgment, or health literacy because of their mental illness; and patient-provider role and power dynamics that may make patients hesitant to express their preferences (
3,
7–
9). The lack of understanding of patient preferences has made it difficult for managers and policy makers to know which treatments should be prioritized for implementation. It has been suggested that aligning delivery of appropriate mental health services with patient preferences could produce large benefits, including improved satisfaction, service utilization, and mental health outcomes (
10–
13).
Accurate assessment of preferences is not straightforward, because responses to direct questioning may be skewed by views of the “right” or most socially acceptable answer to provide, leading to stated preferences that may differ from choices made in real life (
14). Marketing research has shown that choice-based methods of eliciting preferences, such as conjoint analysis, more accurately predict preferences, as revealed by subsequent behavior (
15,
16). In conjoint analysis, possible features of a treatment or product are combined into hypothetical packages and presented sequentially as pairs or groups from which the user selects a preferred combination. In addition to producing results that are reliably associated with consumer behavior, conjoint analysis reveals the relative importance of individual features (e.g., setting, format, and participants) in driving overall preferences, allowing for appropriate prioritization of key features to align with consumer preferences (
14). These features make conjoint analysis popular in health care and suggest that it could provide a useful lens for understanding the weight treatment preferences of people with schizophrenia. The use of conjoint analysis in health care is well documented (
17–
22), and interest in its application in mental health services has grown (
23–
28).
Computerized, automated interfaces have the potential to overcome some of the barriers to assessing preferences of people with schizophrenia. Assessment can be done independently, outside the time-limited clinician-patient interaction; this may increase the efficiency and cost-effectiveness of assessments while also providing privacy, which may improve accuracy (
29). Patient-facing, computerized systems have been successfully applied to routine assessment of clinical status and service use in this population (
30–
32). However, the feasibility of using computerized systems for more involved assessment methods, such as conjoint analysis, is unclear. Questions remain about the validity of assessments and the ability of people with schizophrenia to engage in automated systems involving complicated decision tasks, given variable computer literacy and potential cognitive limitations among individuals in this population (
33,
34). Recent work suggests that computerized conjoint analysis could potentially be used to examine treatment preferences of people with schizophrenia; however, the recruitment settings for these studies, including an online panel (
26) and a clinical trial (
27), may limit the generalizability of results. An additional study examined priorities in quality of life in a community-based sample (
28). Although these early results are promising, further research is needed to establish computerized conjoint analysis as a valid, feasible method of assessing treatment preferences in schizophrenia.
Obesity disproportionately affects people with schizophrenia (
35), contributing to high rates of cardiovascular disease, diabetes, and premature death and leading to reduced quality of life (
36–
39). Antipsychotic medications significantly contribute to weight gain (
40,
41), and recent guidelines have focused on the use of evidence-based psychosocial weight treatment programs in this population (
42). Although numerous such programs exist (
42–
45), uptake and sustained utilization of these interventions by people with schizophrenia are poor (
46–
49). Further research is needed to understand the factors affecting utilization. A recent meta-analysis found that alignment of psychosocial mental health interventions with patient preferences is associated with improved retention (
13). Thus, understanding weight management preferences of people with schizophrenia may improve treatment utilization and outcomes. Although numerous methods exist for assessing preferences, conjoint analysis may be particularly useful in the weight treatment space for people with schizophrenia for several reasons, including association with revealed choices, straightforwardness of the choice task, and nuanced information that can be used to prioritize features.
In this article, we describe the patient-centered development and implementation of an automated, computerized conjoint analysis system for assessing weight management treatment preferences of overweight individuals with schizophrenia. Using a mixed-methods approach, we examined the feasibility and acceptability of this system at an urban community mental health clinic, identified groupwide preferences as determined by the system, and examined the extent to which preferences predicted use of evidence-based weight services.
Methods
Setting and Participants
Participants were recruited through flyers and clinician referrals at a public mental health clinic in Los Angeles. Inclusion criteria were a
DSM-IV chart diagnosis of schizophrenia, age ≥18 years, and either a body mass index (BMI) of 28.0–29.9 with weight gain of 10 pounds in the past 3 months (per self-report) or a BMI of ≥30.0. Exclusion criteria were a medical condition for which a weight program is contraindicated (as determined by a physician), current pregnancy or lactation, previous attendance of a group-based psychosocial intervention for weight management (per self-report), or non-English speaking. Thirty-five individuals participated in feedback sessions during the development of the conjoint analysis system interface. An additional 35 participants completed a conjoint analysis session with the developed interface and were referred to a weekly Enhancing Quality and Utilization in Psychosis (EQUIP) Wellness Program, a manualized, evidence-based psychosocial weight treatment program (
46,
50), which was conducted in 16 weekly sessions at the mental health clinic. Data were collected from September 2016 to July 2017. The project was approved by the University of California, Los Angeles, Institutional Review Board, and all participants provided informed consent.
Development of the Conjoint Analysis Program and User Interface
We used an iterative design process with end users and content experts to develop the preference assessment interface. From the literature, we identified key attributes or features that vary among weight services and that may have substantial outcome effects for patients with schizophrenia. Initially, 22 participants with schizophrenia reviewed options for each attribute and provided feedback, with subsequent modification of options. This process was repeated with a group of 13 additional participants, which produced four final program attributes: location (community or clinic), delivery mode (Internet or in person), leader (clinician or layperson), and training mode (individual or group).
We then developed an attribute image inventory that included several icon choices. A panel of content experts, including psychiatrists, social workers, an anthropologist, a psychologist, and a consumer provider, reviewed the icon options and provided recommendations (e.g., use of icons reflecting racial diversity and icons resembling community buildings). After consensus was achieved, text and screens were presented to an end-user focus group of four individuals with schizophrenia (a subset of those who reviewed the program attributes). Further modifications, based on their feedback, reflected consideration of the cognitive and attentional capacities of the specific end users and included reduction of the number of attributes from four to three presented on each page and better demarcation of transitions between question screens.
The final product was delivered in an interactive interface that included audio and video delivered at a touch-screen kiosk. Each participant was presented with 16 different choice task screens, each displaying two sets of weight treatment program options from which to select one set. Each set of options had three of the four variable program attributes. Choice task screens featured text and representative icons for each attribute, with audio narration of options and instructions. (A sample screen is included in an online supplement to this article.)
Testing of the Conjoint Analysis Program and User Interface
Data were collected from 35 additional participants with schizophrenia. Participants completed a survey that included demographic and household information and items from the 24-item Behavior and Symptom Identification Scale (BASIS-24) (
51). BMI was calculated from measured weight and height. Next, participants completed a preference assessment session with the developed conjoint analysis interface. Finally, they completed the IBM Computer System Usability Questionnaire (CSUQ) (
52) to assess user satisfaction and usability of computer systems and participated in a semistructured interview asking about their experience with the conjoint session. Participants were provided a referral to a 16-session, weekly weight management group, held at the recruitment clinic site.
After 3 months, a subset of participants (N=23) was selected, stratified by whether they had attended any weight management sessions, to complete a qualitative interview exploring their preferences for and barriers to receiving weight management services.
Analysis
CSUQ and BASIS-24 scores were calculated and compared with established norms. Qualitative interviews were transcribed verbatim and analyzed with a content analysis approach (
53). A codebook was developed with a combination of key topics and emergent themes, and transcripts were coded by one team member (A.W.P.F.) and frequently reviewed by the study team. Example codes included lack of transportation, familiarity of program site, and peers/“people like me.” Coded segments were reviewed to identify patterns and overarching themes. Member checking was performed with clinical stakeholders.
Conjoint analysis choice task data were analyzed by using a multilevel logit model to estimate both aggregate and individual preference parameters. The aggregate preference parameters indicated the overall weight of each specific feature of the intervention in the logistic model predicting the choice between two interventions.
Individual Preference Score
The multilevel analysis framework enabled an estimation of the parameters of each participant’s logistic regression predicting the participant’s choice between any two interventions with known features. Using the individual’s preference models, we estimated the person’s likelihood of choosing an intervention with the features of the offered in-person weight management group, compared with a neutral reference intervention with no features. Using this likelihood, we studied how closely the offered intervention matched the individual’s ideal intervention; we report this as a treatment preference score.
We examined associations between individual preference scores and use of an in-person weight management group by using Pearson correlations and point biserial correlations for dichotomous measures of attendance. We used this framework to maximize comparability for the results from the different measures of attendance. We examined three metrics for use: total number of sessions attended (0–16), attendance of any sessions (a dichotomous variable), and the number of sessions attended limited to participants who attended at least one session.
Results
Thirty-five individuals participated in a conjoint analysis session (
Table 1). The study sample was 60% male, 46% White, and 31% African American, with a mean age of 47 years; 97% were not working, and 17% were homeless. The mean baseline BMI was 35.5, with all but one participant meeting criteria for obesity (BMI ≥30). The mean±SD score for baseline psychiatric symptoms as assessed on a modified BASIS-24 (22 items) was 1.58±0.51, compared with scale means of 1.62 and 1.25 for psychiatric inpatients and outpatients, respectively (
51) (possible scores on the modified BASIS-24 range from 0 to 4, with higher scores representing greater symptom severity).
Usability was assessed on the CSUQ scale of 1–7, with 1 reflecting best usability (
Table 2). Mean overall scores for overall satisfaction, system usefulness, information quality, and interface quality ranged from 1.9–2.1. Average time to complete the 16 choice screens was 6.6 minutes. In qualitative interviews, participants frequently praised the ease of use of the system, highlighting its visual aids, audio guidance, and touch-screen interface (“It was easy to read, easy to make your decision”) while criticizing the repetition of response options (“It just got monotonous after a while”).
Groupwide treatment preferences had statistically significant contributions from location (odds ratio [OR]=2.22, favoring clinic over community), leader (OR=1.36, favoring clinician over layperson), and training mode (OR=1.48, favoring group over individual) but not delivery mode (Internet vs. in person) (
Table 3). These preferences did not statistically significantly (p>0.05) correlate with age (r=−0.06), gender (r=−0.19), illness severity as measured with the BASIS-24 (r=0.10), or BMI (r=0.12).
After preference assessment, participants were offered the EQUIP weight management program (
46,
50), which consisted of 16 group-format, in-person sessions held at participants’ usual mental health clinic and led by a mental health professional with training in weight management—features that aligned with overall group preferences. Overall, 49% (N=17) of the participants attended at least one session, with a mean of 8.5±8.0 sessions among those attending, and 23% (N=8) attended eight or more sessions.
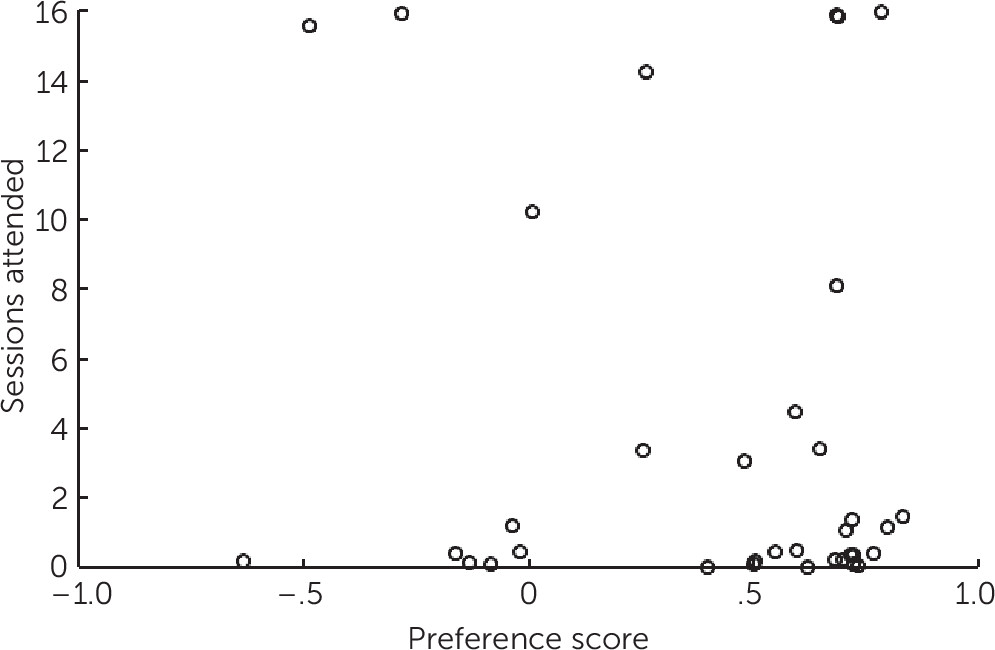
An individual preference score was calculated for each participant, as described above. The relationship between preference scores and attendance is shown in
Figure 1. No statistically significant association was detected between preference score and number of sessions attended (r=0.15, p=0.40), attendance of any sessions (r=0.05, p=0.80), or the number of sessions attended for those attending at least one session (r=–0.34, p=0.18).
Twenty-three participants completed a 3-month follow-up interview asking about their experiences with the offered weight management program. This included 11 individuals who attended one or more weight management sessions and 12 who did not attend any sessions. Among nonattenders, transportation and scheduling challenges were universally cited as the most significant barriers to session attendance. Barriers less frequently mentioned by the nonattenders included preference for one-on-one sessions over groups because of social anxiety, privacy concerns, and previous experiences with group therapy; illness; and lack of motivation. Regarding program features, participants consistently expressed appreciation for services tailored toward individuals with mental illness. The mental health clinic setting was favored for convenience (“Everything happens here for me, as far as medical stuff goes”) and as a trusted location (“I know this place; I already know the people here”). Participants appreciated learning in a group consisting of peers—that is, “people like me.” Likewise, participants consistently favored weight management group leaders with mental health experience, citing the need to understand medication-related weight gain as well as mental health symptoms (“If someone doesn’t know you have a mental health issue, they may not know why you’re acting a certain way”). Participants did not respond favorably to the idea of Internet-based weight management, citing concerns over lack of computer proficiency or access.
Discussion
An understanding of the treatment preferences of people with schizophrenia is important for the implementation of patient-centered, appropriate services. Innovative approaches are needed for eliciting these preferences from such individuals. To address this need, here we developed, implemented, and studied a novel conjoint analysis system to assess preferences for weight management services among individuals with schizophrenia. The automated, interactive, and touch screen–based preference assessment system was feasible to implement, was well received by participants, and had high usability ratings. Preference assessment was valid and produced useful information about weight treatment preferences in this population. Preferences did not consistently correlate with service use, and our qualitative results suggested reasons for this discrepancy.
The conjoint analysis system was designed to meet the needs of individuals with schizophrenia, adapted to accommodate limitations in attention, cognition, or computer literacy. Consumer input was provided throughout an iterative development process involving tailoring that included simple, user-friendly icons and explanatory text, as well as interactive audio and video. Modifications made during the development phase in response to consumer feedback included simplification of text, reduction in features shown in each choice option, and reduction in the total number of choice pages. All participants successfully completed the assessment tasks, and an analysis indicated clear groupwide preferences. Although qualitative and quantitative feedback about the interface was generally positive, some participants disliked the repetition of the system. Accordingly, future applications of conjoint analysis for this population should be designed with consideration for attentional fatigue.
In previous work, weight-loss interventions were less effective for individuals with serious mental illness than for those without mental illness (
54), and it has been suggested that approaches developed for the general population may require specific tailoring to be effective for people with mental illness (
55). However, little is known about the preferences of this population regarding weight management interventions. In this study, groupwide preferences favored weight-loss services based in a mental health clinic rather than the community, led by a clinician with mental health and weight-loss expertise rather than by a layperson with knowledge of weight loss only, and offered in a group format rather than one on one. These preferences were echoed in qualitative interviews with participants after they completed the weight management program. Our results provide support for a model of weight management services tailored to the unique needs of individuals with schizophrenia and housed in a familiar environment. These results may inform the development of future psychosocial weight management interventions for this population.
Although the features of the program offered were consistent with groupwide preferences as assessed by conjoint analysis, individual preferences did not predict program attendance. Our ability to meaningfully interpret the relationship between treatment preferences and service use was somewhat limited by the small sample in this pilot study; however, our results suggest that service utilization was driven by factors beyond preferences. In follow-up interviews, many study participants cited transportation and scheduling as significant barriers to session attendance, consistent with recent findings by Olmos-Ochoa et al. (
56). Clinics and policy makers may want to consider these potential barriers when designing programs, particularly for populations with limited financial resources. Further research is needed regarding the interplay of patient preferences with barriers to and facilitators of service use to improve uptake and utilization in this population.
Conclusions
This work provides critically needed information about the preferences of individuals with schizophrenia regarding delivery of psychosocial weight management interventions. Our results indicate that alignment of services with patient preferences, although likely important, is one of multiple factors affecting utilization by clients. We demonstrated that conjoint analysis may be used for routine, automated assessment of treatment preferences of individuals with schizophrenia, a population that may be among the most challenging for eliciting preferences. Given study participants’ encouraging assessments, adaptation of the interface may prove useful, including tailoring to other vulnerable populations, to assist in routine shared decision making and in the design and deployment of patient-centered services.