In 2018, an estimated 19% of U.S. adults reported having a mental health condition in the past year (
1). Among them, an estimated 19% also had a substance use disorder (
1). The population with mental health conditions and a co-occurring substance use disorder grew by 12% from 2014 to 2018 and tends to include those with more severe mental health conditions and general medical comorbid conditions (
1,
2). Mental health conditions and substance use disorders can be effectively managed as chronic conditions, but care is often underutilized and poorly integrated with the broader health care system (
3). Only 43% of adults with a mental health condition and 51% of adults with both a mental health condition and a substance use disorder report receiving treatment for either their mental health condition or substance use disorder within a year, and financial barriers are a primary factor contributing to foregone care (
1,
4,
5).
High-deductible health plans (HDHPs) comprise an increasing proportion of the employer-sponsored health insurance market (
6). In 2019, nearly 30% of Americans in this market were enrolled in an HDHP, with deductibles in these plans averaging $2,476 (
6). HDHPs are intended to motivate enrollees to control costs by avoiding low-value health care, but enrollees have been shown to cut care indiscriminately (
7). For those with chronic conditions, such as mental health conditions, skipping or delaying necessary care could lead to negative health consequences (
8–
10).
Among commercial health plan enrollees with mental health conditions or substance use disorders, those enrolled in HDHPs tend to have higher out-of-pocket spending on health care costs annually but lower total health care expenditures, compared with non-HDHP enrollees (
11–
13). Among persons with bipolar disorder, one study found that enrollment in HDHPs was associated with a significant reduction in nonpsychiatrist outpatient mental health visits but not with reductions in psychiatrist visits, medications, hospitalizations, or emergency department care (
14). HDHPs might differentially affect those with both a mental health condition and a substance use disorder. Among those with a mental health condition, those with a co-occurring substance use disorder more frequently indicate that their mental health condition interferes with daily activities, and they are more likely than those without a co-occurring substance use disorder to have other conditions requiring medical care, such as heart disease, respiratory disorders, and gastrointestinal disorders (
1,
2,
15,
16). Those with co-occurring substance use disorders face unique barriers to accessing care and more often require higher levels of intensive care, such as inpatient and emergency services, that might be less sensitive to cost-sharing (
5,
17,
18). The severity and multitude of conditions, the types of care received, and existing barriers to care associated with substance use disorders may contribute to differences in how enrollees with mental health conditions respond to HDHPs.
We would expect treatment to decrease among all enrollees with mental health conditions in response to HDHPs. We explored whether enrollees with a co-occurring substance use disorder differ in their response to an HDHP, compared with those with mental health conditions alone. Given their higher care needs and the likelihood of meeting their deductible earlier in the year, enrollees with a co-occurring substance use disorder may decrease utilization to a lesser extent than those with mental health conditions alone. On the other hand, the financial barriers associated with high deductibles combined with existing barriers to treatment may lead enrollees with a co-occurring substance use disorder to reduce their care to a greater extent, compared with those without a co-occurring substance use disorder.
The limited research on the implications of HDHPs for populations with mental health conditions points to potential reductions in service use and heightened financial burden for these populations (
11,
14,
19). We built on this literature with a quasi-experimental evaluation of the effect of HDHPs on commercial health insurance enrollees in the United States with a broad range of mental health conditions and explored the extent to which effects differ among those with a co-occurring substance use disorder.
Methods
In this study, we conducted a difference-in-differences analysis examining the effect of a firm’s decision to offer an HDHP to its enrollees on health care spending and utilization among enrollees with mental health conditions, stratified by whether the enrollee had a co-occurring substance use disorder. This study was approved by the Johns Hopkins University Institutional Review Board.
Study Data
We used deidentified employer-sponsored commercial health insurance claims and detailed benefit design data from the OptumLabs Data Warehouse from 2007 to 2017 to analyze enrollee health care spending (
20). Insurance claims included enrollee and health plan spending for inpatient, outpatient, and pharmacy services for enrollees in plans with medical, pharmacy, and mental health coverage. Benefit design data included in-network medical deductibles, pharmacy deductibles, and blinded firm-level identifiers.
Analytic Sample
Our analytic sample included enrollees with a mental health condition during the period 2007–2017 at firms that began offering or never offered an HDHP. We defined firms that did not offer an HDHP and then began offering an HDHP as treatment firms and firms that never offered an HDHP during the study period as comparison firms (
21).
We excluded enrollee-years with Medicare or without medical, pharmacy, or mental health coverage. We included enrollees ages 12 to 64 who were continuously enrolled and who had valid deductible and demographic information for at least 11 months within a calendar year. Large changes in the number of enrollees at a firm may indicate that enrollees switched to health plans unobserved in the data, so we included only enrollees at firms with stable firm size (<50% change) year over year.
To designate a plan as an HDHP, we used the U.S. Internal Revenue Service’s definition of the minimum individual deductible that is allowed for a plan to also have a health savings account, which varies year to year but averaged $1,214 during our study period. We calculated the proportion of enrollees at the firm enrolled in an HDHP and identified a treatment firm as one that had at least 1 year with none or very few (<5%) of its enrollees enrolled in an HDHP, followed by at least 1 year with a greater share (>5%) of its enrollees enrolled in an HDHP, as in prior literature (
22,
23). We designated firms with 0% of enrollees in HDHPs in all years during the study period as comparison firms.
Within these treatment and comparison firms, we restricted our sample to enrollees with a mental health condition. Following other work, we included enrollees in our analytic sample if they had at least one claim with a mental health diagnosis during the current or a previous year, using
ICD-9-CM codes 295–302 and 306–314 and
ICD-10-CM codes F20–F69, F84, and F90–F99 (
24).
We identified enrollees who also had at least one claim with a substance use disorder diagnosis by using
ICD-9-CM codes 291, 292, 303, 304, and 305 (excluding 305.1 tobacco use disorder and 305.8 antidepressant abuse) and
ICD-10-CM codes F10–F19 (excluding F17.2x tobacco use disorder). Enrollees who had both a mental health and a substance use disorder diagnosis at any point during the study period were categorized as having a co-occurring disorder the first year with either a mental health or a substance use disorder diagnosis and in all subsequent years. We ensured that treatment and comparison firms had a similar proportion of enrollee-years included in the sample both before and after the HDHP offer. (Detailed sample selection specifications and criteria are listed in an
online supplement to this article.)
Measures
Our outcomes included annual spending on combined mental health and substance use disorder care and annual spending on care for conditions other than mental or substance use disorders. We calculated annual spending on combined mental health and substance use disorder care by summing spending on claims with a primary diagnosis for a mental health condition or substance use disorder and spending on claims for psychotropic medications and medications to treat substance use disorders. We calculated annual spending on non–mental health care and non–substance use disorder care as all other claims. Within the combined mental health and substance use disorder category and the non–mental health care and non–substance use disorder care category for all other conditions, we separately calculated spending associated with inpatient hospitalizations, emergency department use, outpatient evaluation and management (E&M) services, and medications. For enrollees with a co-occurring substance use disorder, we separately calculated spending on medications to treat the substance use disorder and psychotropic medications. We top-coded spending at the 99.9th percentile.
We calculated the total days’ supply for psychotropic medications and the average spending per day’s supply of psychotropic medication throughout the year. Among enrollees without a co-occurring substance use disorder, we calculated the number of E&M visit days and the average spending per E&M visit day throughout the year for both mental health and non–mental health E&M visits. (Additional details on outcome construction are provided in the
online supplement.)
Our main independent variable was a firm-level flag indicating that an enrollee-year was at a treatment firm that was interacted with a flag indicating that the enrollee-year occurred after the HDHP offer (i.e., the “post” period among treatment firms). This interaction provided our estimated effect of the impact of an HDHP offer on outcomes.
Statistical Analysis
We estimated two-way fixed-effects models for enrollees with mental health conditions stratified by the presence of a co-occurring substance use disorder. Calendar year fixed effects controlled for secular trends, and firm fixed effects controlled for time-invariant firm-level differences. Differences between enrollees at treatment and comparison firms on a range of covariates were minimal (with standardized mean differences below 0.1) (see
online supplement), but our models controlled for age, gender, race-ethnicity, census division geography, household income level, median census-block education level, and Chronic Conditions Data Warehouse’s chronic medical conditions (
25,
26). Ordinary least-squares regression models were used for all outcomes. Standard errors were clustered at the firm level. All analyses were conducted in Stata, version 16 (
27).
Results
Sample Characteristics
Table 1 displays unadjusted descriptive characteristics of enrollees with a mental health condition with and without a co-occurring substance use disorder before and after an HDHP offer at treatment and comparison firms. Mean annual total health care spending among enrollees with a co-occurring substance use disorder was $15,637, nearly twice that of enrollees without ($7,912). Among enrollees with mental health conditions at firms that offered an HDHP, 43% of enrollees with a co-occurring substance use disorder and 46% of enrollees without, enrolled in an HDHP (see
online supplement).
Effects of HDHPs on Health Care Spending
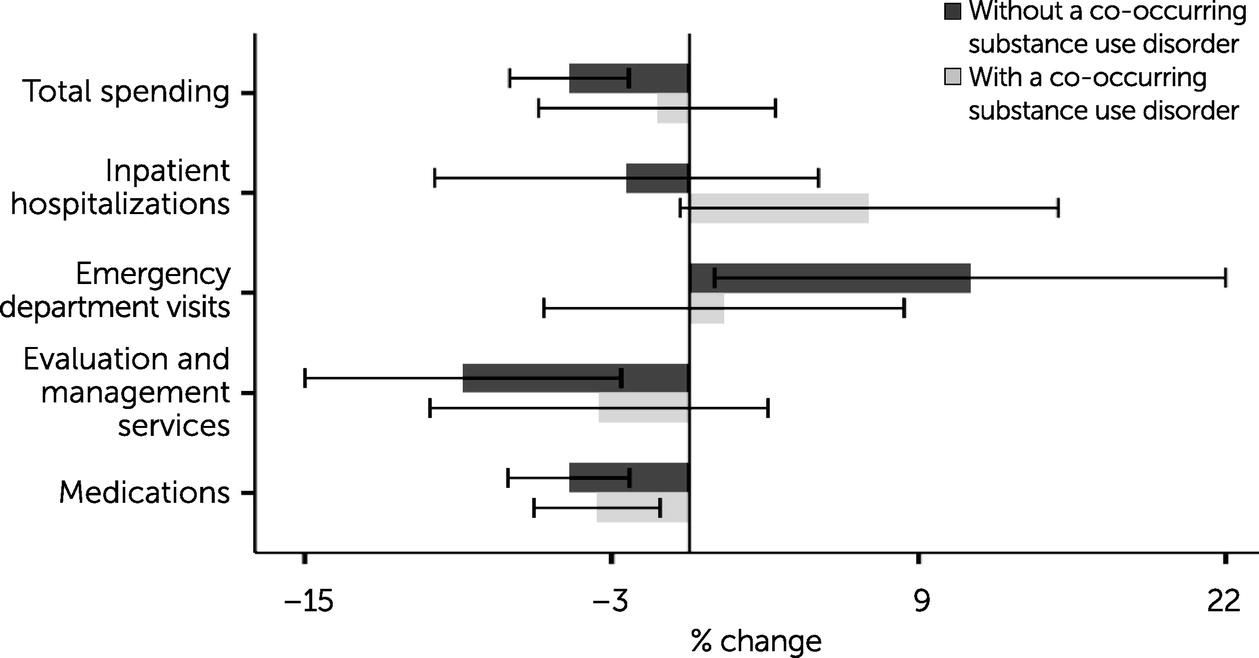
Figure 1 displays estimates of percentage changes in spending on combined mental health and substance use disorder care associated with a firm’s decision to offer an HDHP among enrollees with mental health conditions. We estimated that an HDHP offer was associated with a $40 (95% confidence interval [CI]=$20–$59) average annual reduction in spending on all mental health care among enrollees without a co-occurring substance use disorder. Average annual spending on mental health care before an HDHP offer totaled $821, and this corresponds to a 4.8% (95% CI=2.4%–7.2%) reduction attributable to an HDHP offer. Among enrollees without a co-occurring substance use disorder, we also estimated a 9.1% (95% CI=2.7%–15.4%), or $7, reduction in spending on mental health outpatient E&M services; a 4.8% (95% CI=2.4%–7.3%), or $23, reduction in spending on psychotropic medications; and a 11.3% (95% CI=1.0%–21.6%), or $3, increase in spending on mental health–related emergency department visits.
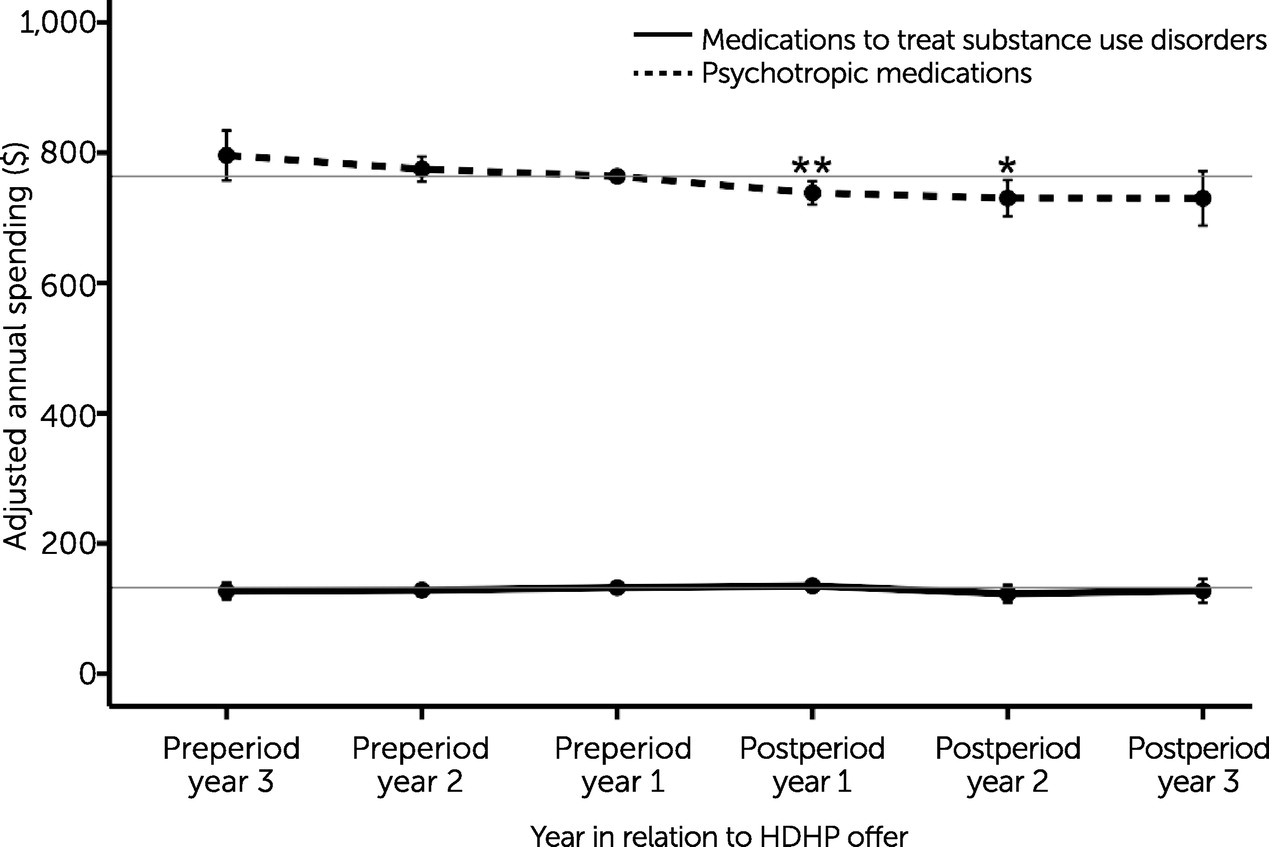
Adjusted mean annual spending levels for psychotropic medications and medications to treat substance use disorders before and after an HDHP offer among enrollees with a co-occurring substance use disorder are displayed in
Figure 2. A 3.7% (95% CI=1.2%–6.2%), or $34, reduction in combined spending on these medications was driven by a $25 (95% CI=$7–$44) reduction in spending on psychotropic medications in the year following the HDHP offer that was sustained in the following year. Across all study years following an HDHP offer, we estimated an average 4.5% (95% CI=1.9%–7.2%), or $35, reduction in annual spending on psychotropic medications among enrollees with a co-occurring substance use disorder. Spending on medications for substance use disorders remained unchanged.
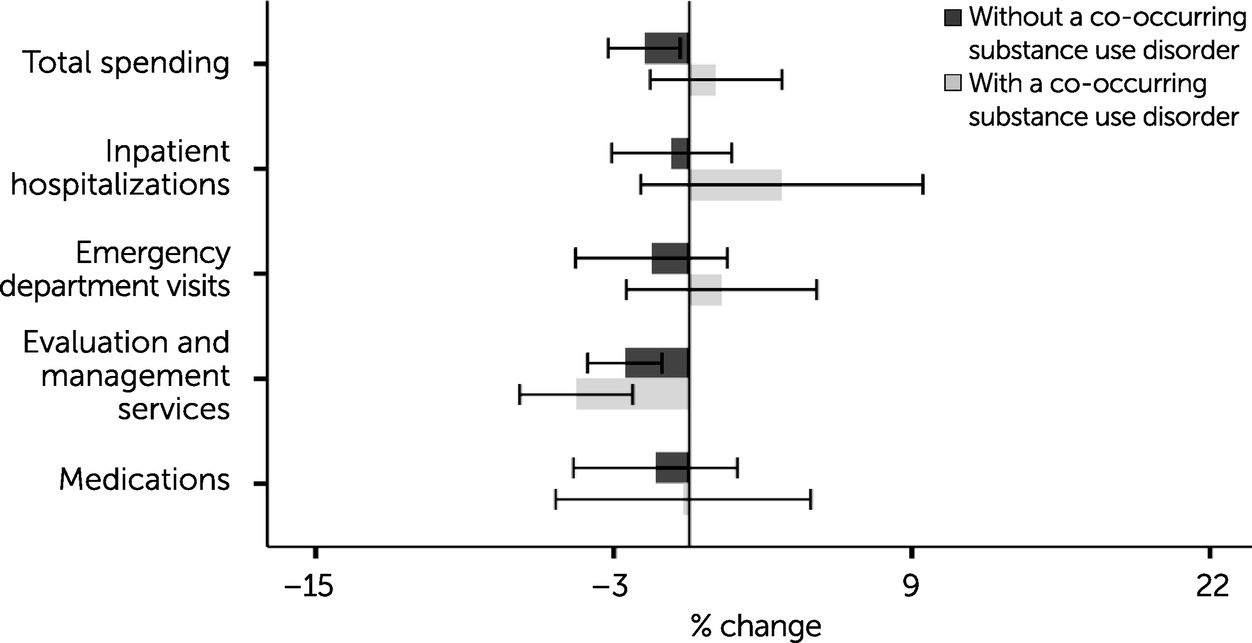
Figure 3 displays estimates of changes in spending on non–mental health care and non–substance use disorder care associated with an HDHP offer among enrollees with mental health conditions. Among enrollees without a co-occurring substance use disorder, an estimated 1.9% (95% CI=0.4%–3.3%), or $128, average annual reduction in spending was detected for non–mental health care. Likewise, among enrollees without a co-occurring substance use disorder, an estimated 2.7% (95% CI=1.1%–4.2%), or $18, reduction in spending on non–mental health outpatient E&M services was associated with an HDHP offer. Among enrollees with a co-occurring substance use disorder, we detected an estimated 4.7% (95% CI=2.3%–7.0%), or $39, reduction in annual spending on non–mental health and non–substance use disorder outpatient E&M services.
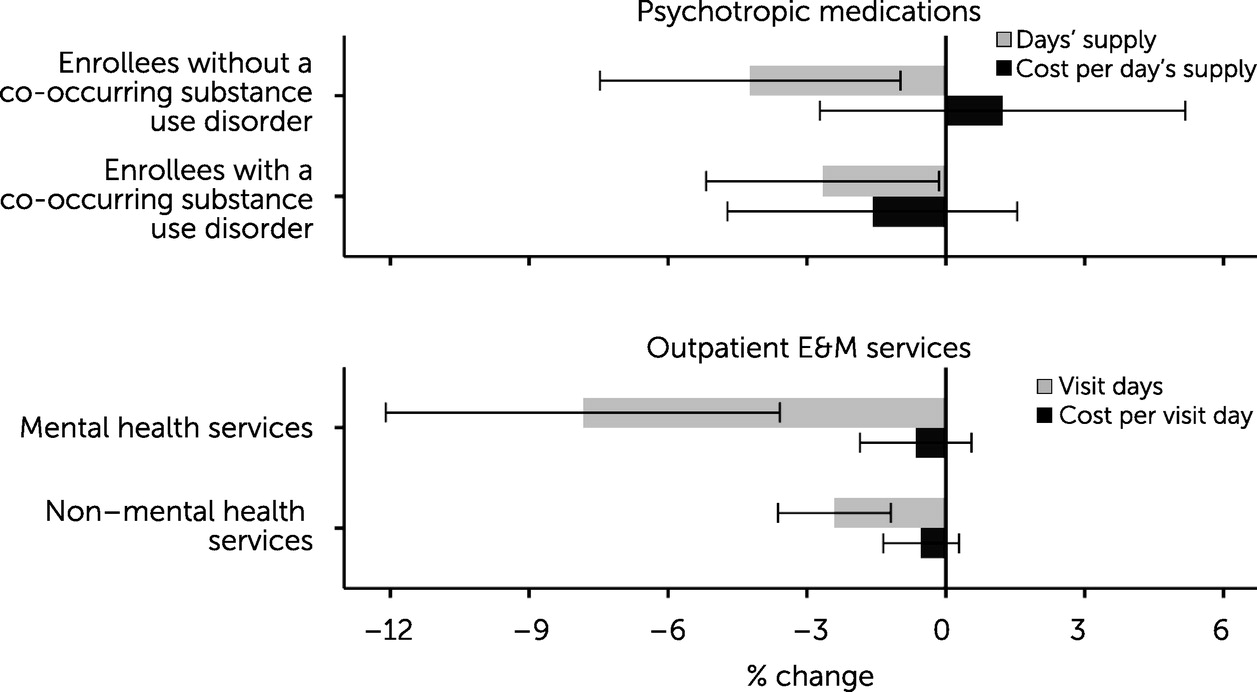
As shown in
Figure 4, for enrollees with mental health conditions, the observed reduction in spending on psychotropic medications was driven by a 4.2% (95% CI=0.9%–7.4%), or 8.1-day, reduction in quantity of the days’ supply of these medications within a year for those without a co-occurring substance use disorder and a 2.7% (95% CI=0.1%–5.1%), or 7.6-day, reduction for those with a co-occurring substance use disorder. Similarly, among enrollees without a co-occurring substance use disorder, we found a 7.9% (95% CI=3.6%–12.2%), or 0.07–visit-day, reduction in mental health outpatient E&M visits and a 2.4% (95% CI=1.1%–3.6%), or 0.12–visit-day, reduction in non–mental health outpatient E&M visits. We did not detect changes in the cost per unit of these medications or services associated with an HDHP offer. (Full model results for Figures
1–
4 are included in the
online supplement.)
Differences in Effect of HDHP Offer
We compared the percentage change in health care spending associated with an HDHP offer among enrollees with mental health conditions without a co-occurring substance use disorder to the percentage change in health care spending associated with an HDHP offer among enrollees with mental health conditions with a co-occurring substance use disorder (displayed in Figures
1 and
3) and found these changes to be largely similar.
Sensitivity Analyses
We conducted a number of sensitivity analyses varying firm-level thresholds used in identifying treatment firms, sample specifications, top-coding thresholds, and modeling approaches and found that these results were qualitatively similar to the results presented above in all specifications (see
online supplement).
Discussion
In this study, we explored how HDHPs affected enrollees with mental health conditions with and without a co-occurring substance use disorder. We found that all enrollees with mental health conditions reduced spending in some treatment categories when offered an HDHP, primarily for outpatient E&M services and psychotropic medications. These findings are largely consistent with those of previous studies evaluating HDHPs that have demonstrated reductions in office visits and medication use for other chronic conditions (
22,
28–
30).
It is not clear why an HDHP offer was associated with reductions in spending on psychotropic medications but not with reductions in spending on medications for substance use disorders or other medical conditions. Our estimate of a reduction in psychotropic medication spending associated with an HDHP offer differs from one recent HDHP study, which found no decrease in utilization of medications for the treatment of bipolar disorder (
14). It is possible that the decreases in spending we observed were driven by medications for less severe mental health conditions. Other work has shown cost-sharing–induced reductions in the utilization of antidepressants and has documented greater price responsiveness for antidepressants, compared with medications to treat serious mental illness (
31,
32).
Prior literature exploring HDHPs has primarily suggested reductions or no changes in the utilization of emergency department services, but some studies have found increases in emergency department utilization among sicker and less wealthy enrollees (
7,
10,
33,
34). In this study, we found a decrease in spending on outpatient E&M services and psychotropic medications coupled with an increase in spending on mental health–related emergency department visits, suggesting that an HDHP offer may be associated with foregoing or limiting necessary mental health care, possibly resulting in adverse events. This is potentially worrisome and needs further study.
Our study had several important limitations. First, despite the rigorous quasi-experimental study design, the study was observational, and enrollees were not randomly assigned to HDHP and non-HDHP plans. Because the decision by an enrollee to select an HDHP is not random and is likely associated with other characteristics of the enrollee, we instead focused on the employer’s choice to offer an HDHP in order to mitigate this selection bias. Additionally, the likelihood of receiving mental health or substance use disorder care, and thus the likelihood of entering the sample, might have been influenced by enrollment in an HDHP. To mitigate any potential biases, we ensured that our clinical criteria were balanced across treatment groups (see
online supplement) and conducted sensitivity analyses requiring enrollee-level fixed effects (see
online supplement), which produced consistent findings. Second, our analytic strategy relied on the assumption that outcome trends at comparison firms were an appropriate approximation for what would have happened at firms that offered an HDHP had they not offered an HDHP. This cannot be directly tested, but outcome trends tested by using event study models were generally parallel in the years directly preceding an HDHP offer, with few exceptions (e.g., psychotropic medications). Findings were also consistent in these event study models (see
online supplement).
Third, with a somewhat higher proportion of enrollees in the South and Central regions, our results may not be generalizable to the broader employer-sponsored health insurance market. Fourth, the data used in this study did not capture services for which enrollees paid cash only, and not all substance use disorder treatment may be accompanied by a diagnosis code, potentially affecting sample selection. A sensitivity analysis that used alternative criteria (
35) for selection of the substance use disorder sample yielded consistent results (see
online supplement). Finally, this study focused on the impact of deductible levels only and did not account for other cost-reduction tools that might have been implemented by the employer at the time of the HDHP offer. Although other studies have incorporated other tools into analyses for a small number of employers, our study has the benefit of examining a large and heterogeneous group of employers over a long study period (
8).
Conclusions
Our findings suggest that HDHPs lead those with mental health conditions to reduce the use of needed medications and outpatient care. Policy makers, employers, clinicians, and health systems should consider the ways in which insurance design leads enrollees with mental health conditions to restrict care, with potentially detrimental health consequences.