Racial-ethnic disparities in health service outcomes, satisfaction, and engagement for youths are well documented. Although examination of outcomes by race-ethnicity remains limited and findings have been mixed (
1,
2), results show that youths of color generally have poorer treatment outcomes compared with their White counterparts (
3,
4). Disparities in satisfaction and attrition also remain a consistent theme in recent literature. Johnson and colleagues (
5) found that caregivers with children of color reported greater barriers to care and poorer quality of care in their child’s mental health services. This finding is consistent with previous studies in which caregivers of children of color receiving mental health services reported higher levels of disrespect, less satisfaction, and poorer quality of care (
6). These perceptions of care are often linked to premature termination of services for Black youths and families compared with their White counterparts (
6,
7).
Wraparound care coordination is a comprehensive, family-driven model for providing services to families and youths with emotional and behavioral challenges (
8,
9). Guided by 10 principles for individualized, culturally competent, and community-based practice (
8), wraparound care includes regular child and family team (CFT) meetings, in which youths, caregivers, service providers, and natural supports (i.e., supports that occur from relationships developed in natural environments, such as school, work, family, etc.) are brought together with a care coordinator to develop and progress through an individualized, comprehensive plan of care. Wraparound literature has highlighted the positive impact of these services on a variety of outcomes (
10). A 2009 meta-analysis (
10) revealed the positive influence of a wraparound approach on youths’ living situations, mental health, functioning, and justice involvement. The same study noted that although the literature on wraparound care is expanding and findings are generally positive, outcomes research remains preliminary (
10).
Furthermore, there have been recent calls to integrate evidence-based models such as wraparound care within existing systems of care (SOCs) (
11). SOCs are comprehensive networks of community-based services (e.g., mental health, child welfare) aimed at increasing access to and quality of care for children with emotional and behavioral difficulties and their families (
12–
14). Literature on wraparound care within SOCs has often focused on fidelity in service implementation (
7,
15–
17). Findings show that coordination across multiple types of service (wraparound) within the infrastructure of an SOC can decrease gaps in care and increase communication between service providers (
18,
19). Positive outcomes for youths include clinical improvements, fewer contacts with law enforcement, and more stable living conditions (
20–
22).
Recent literature also provides evidence that wraparound care improves access to care and mental health functioning across racial-ethnic backgrounds (
7,
23). Miech and colleagues (
23) found potential for wraparound care within an SOC to improve treatment access for historically marginalized youths and youths of color. Similarly, Yohannan and colleagues (
7) found consistent improvement in functioning across racial groups receiving wraparound care within an SOC. However, the same study also found higher levels of dropout among low-income African American families. Although preliminary evidence shows that wraparound care coordination in some key areas may be beneficial, more research is needed to investigate the comprehensive impact on youths and families across racial-ethnic identities.
The current study aimed to understand racial-ethnic disparities in access and outcomes among youths with emotional and behavioral disorders and their caregivers who completed wraparound care coordination in a statewide SOC. We investigated differences across racial-ethnic groups regarding the characteristics of intake, service provisions, and outcomes. We then examined the impact of participation in wraparound care coordination on the level of racial-ethnic disparities in outcomes at follow-up. Finally, we conducted analysis to investigate predictors of mutual discharge from services (i.e., reached agreement between family and care coordinator that goals had been met).
Methods
Procedure
This exploratory study utilized care coordination data from a statewide SOC providing wraparound care collected at intake, during service provision, and at follow-up to understand the experiences of youths and caregivers across racial-ethnic identities. Because the average length of stay in care is 6 months, follow-up data included 6-month assessment and discharge information. We hypothesized that wraparound care coordination provided within an SOC would have a positive impact on youths and families. This hypothesis is consistent with previous studies (
20–
22); however, the literature examining racial-ethnic disparities remains limited. Therefore, our study was exploratory.
Data
We used a subset of data collected from all families enrolled in wraparound care from 2016 to 2020. Specifically, the subset included information from families who gave permission for their data to be shared with investigators. Data on characteristics of services and CFT meetings and on discharge status were collected by care coordinators. Demographic characteristics, outcome assessments, and perceptions of care were collected from caregivers at intake and at a 6-month follow-up assessment. Data were analyzed with IBM SPSS, version 26.0. This study was waived from institutional review board approval.
Participants
Families were included in the analyses if they completed at least 3 months of services and a follow-up assessment within 7.5 months of intake. A total of 111 families (10%) were excluded from the analysis because they either completed less than 3 months of services or completed 3–7.5 months but withdrew from services before the completion of a follow-up assessment. Preliminary analyses regarding these 111 families revealed no significant differences in youths’ race-ethnicity, gender, or age compared with families included in the analyses.
Instruments
Demographic and service characteristics.
Demographic information collected from caregivers included youths’ age, sex, and race-ethnicity. Service characteristics included days of service enrollment and discharge status. Discharge status was dichotomized to determine whether the families were mutually discharged from services or discharged because of either having no contact for 90 days or withdrawing from or refusing treatment. Families with other discharge statuses (e.g., clinically referred out, death, other) were excluded from relevant analyses.
CFT meetings.
Data collected to document adherence to the National Wraparound Initiative practice standards (
24) were recorded by care coordinators. These analyses included the number of CFT meetings between intake and 6-month follow-up and time elapsed between intake and the first CFT meeting.
Ohio Scales (parent rating).
The Ohio Scales (
25) are a valid and reliable measure of youths’ functioning and problem severity (
26) across race-ethnicity (
27; Laba, 2020, unpublished master’s thesis). The parent rating form (OSP) was used to collect information regarding youths’ level of functioning and problem behavior at intake and follow-up. Cronbach’s alphas were 0.909 and 0.941 for the functioning scale and 0.884 and 0.898 for the problem behavior scale at intake and follow-up, respectively.
Child Trauma Screen (CTS).
The CTS is a brief screening instrument (
28) that measures trauma exposure and symptoms of posttraumatic stress disorder among youths. In a validation sample where 32% of children were African American, 26% Latinx, and 18% White, the CTS demonstrated strong validity (
29). The caregiver form of the CTS was used to understand the frequency of trauma exposure and the level of trauma symptomatology among youths. A cutoff score of 8 or higher on trauma symptomatology was used to indicate clinical significance (
29). Cronbach’s alpha was 0.789.
Caregiver Strain Questionnaire–13 (CGSQ-13).
The CGSQ-13, a 13-item version of the CGSQ (
30) that was used to measure caregiver strain as part of the national evaluation for Substance Abuse and Mental Health Services Administration SOC grantees, includes three subscales—objective strain (OS), subjective internalized strain (SIS), and subjective externalized strain (SES)—as well as a global strain score. Cronbach’s alphas were 0.877 and 0.913 for the OS, 0.761 and 0.809 for the SIS, 0.664 and 0.747 for the SES, and 0.883 and 0.918 for the global strain scores at intake and follow-up, respectively.
Perceptions of care.
The Perceptions of Care section of the National Outcomes Measures was used to understand caregivers’ satisfaction with services (
31). Caregivers indicated their level of agreement on eight items regarding the services they and their child received. Questions inquired about service staff (e.g., “Staff treated me with respect”), inclusion in youths’ services (e.g., “I helped choose my child’s services”), and satisfaction with services (e.g., “Overall, I am satisfied with the services my child received”).
Results
Caregiver-reported information regarding 1,138 youths were included in the analyses. A total of 238 (21%) caregivers identified their youths’ race-ethnicity as non-Latinx Black, 352 (31%) as non-Latinx White, and 458 (48%) as Latinx of any race. Youths of other racial-ethnic identity (e.g., Asian, Native Hawaiian, American Indian, multiracial) were excluded from the study because of small group sample size (N=42). Furthermore, 725 (64%) youths identified as male. The age of youths ranged from 3 to 19 years, with a mean±SD age of 11.53±3.73 years.
Disparities at Intake
Analyses of variance (ANOVAs) were completed to assess for significant differences at intake on the basis of youths’ race-ethnicity, while analyses controlled for age and sex. On the Ohio Scales, non-Latinx White youths exhibited significantly more problem behaviors (F=9.62, df=2 and 984, p<0.001) and significantly lower functioning (F=9.69, df=2 and 981, p<0.001), compared with their non-Latinx Black and Latinx counterparts. Similarly, caregivers of non-Latinx White youths reported significantly higher levels of global strain (F=6.93, df=2 and 962, p=0.001) and OS (F=6.64, df=2 and 984, p=0.001) on the CGSQ-13 at intake, compared with caregivers of non-Latinx Black and Latinx youths. Outcomes regarding number of lifetime traumatic events, trauma symptomatology, CGSQ-13 SIS score, and CGSQ-13 SES score yielded no differences across youths’ race-ethnicity. Likelihood of past trauma exposure revealed a significant overall ANOVA (F=3.65, df=2 and 963, p=0.026) but no post hoc differences on the basis of youths’ race-ethnicity.
Given a significant ANOVA finding, regression analyses (either logistic or linear, depending on the nature of the outcome) were conducted to examine the extent to which race-ethnicity affected outcome variables, while analyses controlled for age and sex. Non-Latinx White was used as a reference category for all regression analyses. Overall, regression analyses mirrored ANOVA findings in that non-Latinx White youths exhibited significantly higher likelihood for a history of trauma (odds ratio=0.67, p=0.025), compared with Latinx youths, as well as high problem behavior scores and lower functioning scores on the Ohio Scales, compared with non-Latinx Black (β=–5.186, p<0.001; β=3.973, p=0.001) and Latinx (β=–3.540, p=0.001; β=3.546, p<0.001) youths, respectively. Similarly, caregivers of non-Latinx White youths reported significantly higher levels of caregiver strain on the CGSQ-13 global (β=–2.438 and –2.604; p=0.015 and 0.001) and CGSQ-13 OS (β=–1.430 and –1.592; p=0.014 and 0.001) scales at intake. Full regression results are presented in
Table 1.
Disparities During Service Provision
A similar analysis strategy was used to investigate racial-ethnic disparities in service provision measured by characteristics of CFT meetings. Results revealed no racial-ethnic differences in the number of days until participants’ first CFT meeting. Significant differences were found in the number of CFT meetings (F=4.91, df=2 and 812, p=0.007): non-Latinx White youths had significantly more CFT meetings (3.48±1.46) compared with their non-Latinx Black (3.11±1.55) and Latinx (3.13±1.52) peers. In subsequent regression analyses, these ANOVA results were confirmed. Specifically, administrative records demonstrated that non-Latinx White youths had more CFT meetings compared with their non-Latinx Black (β=−0.371, p=0.014) and Latinx (β=–0.371, p=0.001) counterparts.
Disparities at Follow-up and Discharge
Next, the same analytic strategy was applied to examining racial-ethnic disparities among outcomes collected at follow-up, while we controlled for scores at intake. ANOVA results revealed no racial-ethnic differences in the amount of change from intake to follow-up on any outcome measures, including all scales of the CGSQ-13 and OSP, with one exception. Although the amount of change in trauma scores between baseline and follow-up were nonsignificant on the basis of race-ethnicity, regression results revealed that non-Latinx White youths displayed higher levels of trauma symptoms at follow-up and increased likelihood that their trauma symptoms fell above the clinically significant range in comparison with non-Latinx Black (β=−1.077 and –0.0786; p=0.002 and 0.004) and Latinx (β=−1.000 and –0.778; p=0.001 and<0.001) youths, respectively. Finally, no racial-ethnic disparities were found in examinations of differences in mutual discharge (F=2.21, df=2 and 966, p=0.110) or the number of days enrolled in services (F=1.61, df=2 and 878, p=0.201).
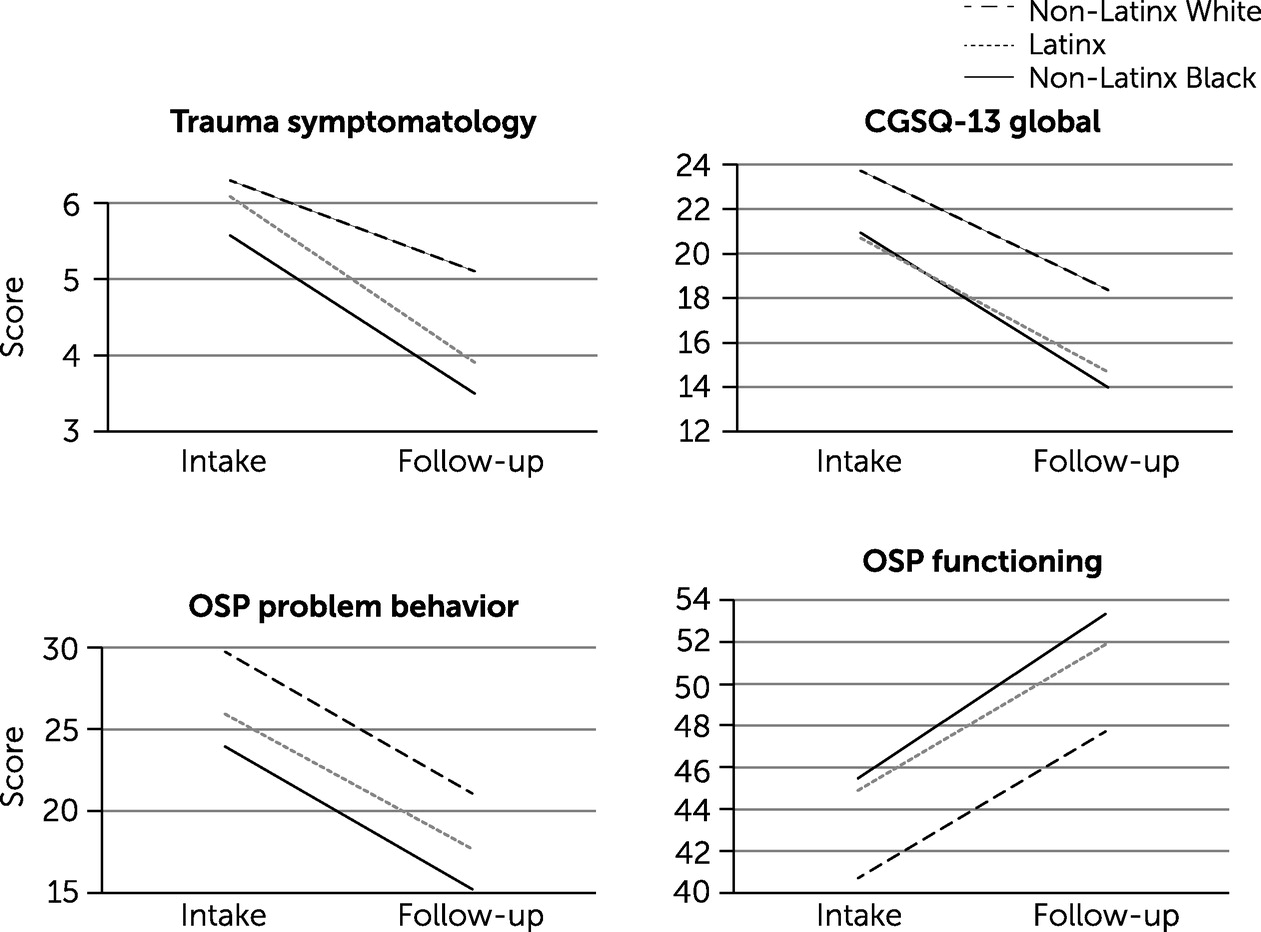
Impact of Wraparound Care Coordination in Level of Disparities
To understand the impact of care coordination on racial-ethnic differences at both intake and follow-up (while analyses controlled for intake scores), we examined ANOVA post hoc results for CGSQ-13 global scores, OSP problem behavior and functioning scores, trauma symptoms, and whether trauma symptoms were clinically significant. Overall, results revealed the positive and equitable impact of wraparound care coordination with no significant differences in rate of change on any outcome variables across race-ethnicity. Although caregivers of non-Latinx White youths reported higher levels of youths’ problem behavior, lower levels of youths’ functioning, and higher levels of caregiver strain at intake and follow-up, their rate of change did not differ from others receiving care coordination. Similarly, while all racial-ethnic groups had similar levels of symptoms related to trauma at intake and experienced a similar and significant decrease in trauma symptoms at follow-up, non-Latinx White youths exhibited significantly higher levels of trauma symptoms compared with their peers. Full results are displayed in
Figure 1.
Satisfaction With Services and Mutual Discharge
ANOVA analyses were conducted to examine differences in perceptions of care on the basis of youths’ race-ethnicity. Results revealed that caregivers of non-Latinx Black youths reported significantly less satisfaction with respect from staff (F=4.08, df=2 and 849, p=0.017) and staff’s respect of their religious beliefs (F=4.80, df=2 and 848, p=0.008) than did caregivers of non-Latinx White and Latinx youths. Post hoc results are outlined in
Table 2. Additionally, chi-square analysis revealed no significant difference in the rate of nonmutual discharge on the basis of youths’ race-ethnicity (χ
2=4.41, N=969, df=2, p=0.110).
Finally, to investigate whether race-ethnicity and perceptions of care affected the discharge status of families from care coordination, a logistic regression was completed to determine predictors of whether families mutually discharged from services, with age, sex, race-ethnicity, and perceptions of care as predictors. Results revealed that caregivers’ feeling that they had the ability to choose their child’s services was the only significant predictor of mutual discharge from services (β=0.927, p=0.001).
Discussion
Racial and Ethnic Disparities at Intake, Service Provision, and Follow-up
This study aimed to better understand racial-ethnic differences in the experiences of youths with emotional and behavioral difficulties and their caregivers enrolled in wraparound care coordination within a statewide SOC. Results from caregiver-reported data revealed few significant differences across racial-ethnic groups and an overall positive impact of services on youths and caregivers. These findings expand the literature highlighting the positive impact of a wraparound approach in promoting positive outcomes for youths and families across racial-ethnic groups (
7). In contrast to findings in previous literature regarding racial-ethnic disparities in outcomes of clinical care (
3,
5,
32,
33), the availability of wraparound care coordination, in combination with an SOC philosophy of individualized, family-centered care, likely proved especially beneficial for youths and families across racial-ethnic backgrounds and contributed to the lack of disparities found in the current study. Choice in services was also a significant predictor of mutual discharge, demonstrating the importance of youths’ and caregivers’ engagement in service planning. These findings point to the benefits of services that are based on the family’s identified strengths and needs; include collaboration across providers; and allow families, supported by a care coordinator, to lead their service planning.
Results revealed that at intake, caregivers of non-Latinx White youths reported higher levels of caregiver strain, youths’ trauma, and problem behaviors and lower levels of functioning compared with their peers. Furthermore, although non-Latinx White youths had more CFT meetings, their caregivers reported that these youths experienced higher levels of trauma symptoms after 6 months. Overall, this pattern points to a disparity in outcomes, with non-Latinx White youths and their caregivers entering and exiting care with higher levels of trauma, problem behavior, and caregiver strain and lower functioning compared with other groups. Future research would benefit from examining factors that affect this pattern, including the threshold by which youths are referred to services and the influence of self-report. Although the CGSQ-13 exhibited adequate validity in this study, previous literature has noted possible racial-ethnic differences in the self-report of caregiver strain (
34).
Satisfaction and Mutual Discharge
Results revealed no racial-ethnic differences in the rate of mutual discharge from services. This finding is contrary to previous literature that found higher rates of attrition among African American youths in wraparound care compared with White youths (
7,
32). Although the cause of this incongruity is beyond the scope of this article, the findings indicate an encouraging prospect for the ability of wraparound care to reach and engage families across racial-ethnic groups.
Findings did not indicate a link between satisfaction with care and early termination. Although non-Latinx Black caregivers reported less satisfaction than their counterparts with the level of respect from staff and of respect for their religious beliefs, there were no differences in rates of mutual discharge from services. Lower satisfaction ratings among non-Latinx Black caregivers are consistent with recent literature (
5) and point to the need for increased attention and effort to explore the factors influencing satisfaction with care and increased efforts to eliminate this disparity and ensure effective and satisfactory services for all families.
Limitations and Future Directions
This study had several limitations. First, because of sample size, youths with some racial-ethnic identities were excluded from the analyses, and we were unable to delineate racial identities within the Latinx group; future studies are encouraged to investigate these possible differences. Second, the study utilized caregiver-reported data. Reports from youths on their perceptions of services and their impact on mental health would be valuable to explore. Finally, the current study did not examine all measures of wraparound adherence (e.g., youth or family participation), and future studies should examine differences in these factors on the basis of youths’ race-ethnicity.
Conclusions
Because racial-ethnic disparities in children’s services remain, investigations are needed of services that support families across racial-ethnic groups. The current study examined racial-ethnic disparities among youths and caregivers enrolled in wraparound care coordination within an SOC. With few exceptions, individualized services were provided with equity, and significant improvement in outcomes was found across racial-ethnic groups. Although rates of dropout and mutual discharge were similar across groups, non-Latinx Black caregivers reported less satisfaction with respect from staff and staff’s respect of their religious beliefs. The findings highlight the need to investigate perceptions of care among non-Latinx Black caregivers and the potential for wraparound care within an SOC to address the mental health needs of families across racial-ethnic identities.