The impetus to develop alternative models of delivery of primary medical care for seriously mentally ill patients is driven by their increased physical morbidity (
1,
2,
3,
4,
5,
6) and the barriers they encounter in gaining access to primary care. In addition, this population experiences increased mortality (
7,
8,
9), with more frequent deaths from cardiovascular, respiratory, digestive, metabolic, genitourinary, cerebrovascular, and HIV-related illnesses than among the general public (
10,
11,
12,
13,
14,
15). The increased mortality apparently is not attributable solely to socioeconomic status, because mortality rates among persons with serious mental illness are high even when this group is compared with matched low-income subjects (
16).
The increased risk of physical disease among persons with serious mental illness may be partly attributed to their reduced access to primary care (
17) and to adverse health behaviors. They may have difficulty complying with treatment once a problem is noted, which may accelerate the development of complications (
18). Increased risk for medical problems and reduced access to care may contribute to unmet needs for physical health care (
14,
19,
20,
21).
In the usual "cooperative" model of health care delivery, primary care services and specialty mental health care services are provided by clinicians separated in time and space. However, clinicians not attuned to the special needs of persons with serious mental illness may fail to address key issues or may work at cross-purposes. For example, they may prescribe medications that interfere with management of medical or psychiatric problems. Clinicians' lack of awareness of the special needs of this population may lead to delay of effective interventions, increased complications, functional impairment, increased use of services, and higher costs.
Consolidating care to one physician may redress some problems associated with delivery of primary care services to persons with serious mental illness. However, the typical primary care provider may not be well suited to addressing the primary care and psychiatric needs of these individuals. Primary care providers may fail to integrate treatment for psychiatric problems. They may manifest negative attitudes toward persons with serious mental illness and their emotional and behavioral problems. The psychiatrist may fear that such patients will create an uncomfortable environment for their patients without serious mental illness (
7,
22,
23",
24,
25). Indeed, studies have concluded that "recognition and management of common mental disorders in primary care are deficient" (
26) and that "general practitioners [caring for patients with mental illness] are required to undertake a significant body of work for which they may be inadequately trained" (
27).
Efforts to improve management of psychiatric illness in the primary care setting focus on detection of common nonpsychotic disorders and do not meet the needs of persons with serious mental illness. A related strategy involves primary care management with on-site psychiatric backup; in this case, too, the primary care physician has the dominant role, despite the predominantly psychiatric needs of persons with serious mental illness.
At the same time, the typical psychiatrist may lack competence to care for physical health problems and interest in caring for such problems and may fear that countertransference or transference devolving from aspects of primary care could adversely affect the therapeutic relationship (
28,
29,
30). Management of patients by a psychiatrist with on-site delivery of primary care by a primary care physician is viable but does not address many of the barriers described above. Some joint primary care-psychiatry residency programs have been established, but funding for such programs is limited (
31), and dually trained physicians remain scarce.
A potential solution may be to reorganize the mental health clinic to provide integrated access to primary care for persons with serious mental illness by using a single practitioner. In the model considered here, this practitioner would be a "primary care psychiatrist"—that is, a psychiatrist with additional primary care training and supervision by an on-site internist. This approach has the potential to provide enhanced management of psychiatric conditions by providers who best know the patient and who are schooled in the special problems of this population, while at the same time facilitating patients' access to primary care. Psychiatrists are often the physician of first and most consistent medical contact for persons with serious mental illness (
32), and they may be more astute observers of the interaction between physical and mental illness (
14,
29,
33).
A recent survey of community mental health directors in Veterans Affairs and community facilities identified substantial interest in psychiatrists' providing primary care to persons with serious mental illness (
34). Analogous approaches have been successfully employed in other specialty care settings for patients with cancer and HIV and for geriatric patients (
35,
36,
37,
38,
39). However, in these instances the principal providers were typically internists with substantial training in primary care delivery.
To competently fill a role in the integrated model of primary care service delivery, psychiatrists must be partially retrained in routine diagnostic and primary care skills and provided with support from primary care physicians and medically oriented staff as well as from information tools, such as practice guidelines and diagnostic and treatment algorithms (
20). An integrated model of primary care delivery with the psychiatrist designated as the primary care provider may partly overcome some of the system, provider, and patient barriers that persons with serious mental illness encounter in obtaining primary care and may provide an expanded clinical role for psychiatrists. Such a model may result in improved care, enhanced patient satisfaction, and reduced health care costs due to timely use of appropriate primary care services.
The study reported here sought to identify elements of primary care that might be appropriately performed by primary care psychiatrists. A multidisciplinary panel of health practitioners and administrators formally rated whether a psychiatrist, a primary care psychiatrist, an internist, or a medical specialist could reasonably provide evaluation, treatment, or preventive care for uncomplicated instances of selected physical health conditions or procedures.
Methods
An adaptation of the appropriateness rating methods jointly developed by Rand and the University of California, Los Angeles (
40), was used to ascertain which elements of primary care could reasonably be provided by psychiatrists with primary care training. The overall study encompassed six elements: defining the population of seriously mentally ill persons to whom integrated care would be delivered; defining the integrated model of primary care delivery; identifying and convening an appropriateness panel representing the views of health practitioners and hospital administrators to rate which medical care practices might be performed by psychiatrists with and without additional primary care training; constructing a list of conditions, preventive interventions, and procedures to be rated; defining the rating procedure; and conducting the rating. These elements are discussed below.
Target population. The target population for integrated primary care delivery included persons with serious mental illness who did not have an established relationship with a primary care provider in a VA primary care clinic. An established relationship with a primary care provider was defined as two or more visits to a primary care provider, including one visit within the past year.
The definition of the target population was from the Veterans Health Administration's committee on care of severely and chronically mentally ill veterans, which defines persons with serious mental illness as patients with a
DSM-IV diagnosis that results in a disability. The diagnoses included in our definition were similar to those included in the definition of severe mental disorders used by the National Institute of Mental Health (
41). Patients in the study were enrolled in the Veterans Affairs San Diego Healthcare System's outpatient mental health clinic and were diagnosed as having schizophrenia-spectrum illness (schizophrenia, schizoaffective disorder, and delusional disorder) or major mood disorder (unipolar and bipolar mood disorder).
Defining the integrated model. The integrated model of primary care delivery in the mental health clinic includes several elements. Psychiatrists involved are recruited from staff psychiatrists currently working in the Veterans Affairs San Diego Healthcare System's mental health clinic. Psychiatrists assigned to the integrated model receive an orientation to primary care followed by weekly didactic sessions related to primary care issues that they would be expected to address.
Algorithms and guidelines for each condition to be addressed are developed or adapted from several sources, including the American College of Physicians (ACP), the National Heart, Lung, and Blood Institute, the Agency for Health Care Policy and Research (AHCPR), the Canadian Task Force on the Periodic Health Examination, and Kaiser guidelines as well as from algorithmic approaches available in texts and review articles. Increased use of such guidelines may improve quality of care; adherence to guidelines as well as use of strategies to increase compliance with practice guidelines and protocols, are areas of ongoing interest and research (
42,
43,
44,
45).
In the integrated model, psychiatrists are encouraged to follow guidelines and to consult the on-site internist if any questions arise about diagnosis or treatment planning. If at any time the internist and psychiatrist judge a patient's physical condition as too complex for the integrated model, the patient is referred to the internal medicine clinic for treatment, whether or not the patient was initially rated as appropriate for management by a primary care psychiatrist. This policy ensures that psychiatrists do not care for patients with conditions that are outside their scope of training.
The appropriateness panel. The appropriateness panel consisted of the chief of staff and the chief of psychiatry or their designees from three southern California VA health care systems—San Diego, Loma Linda, and West Los Angeles—as well as staff internists, psychiatrists, and representatives from the nursing service from these systems. The full panel was made up of 14 panelists, although, as described below, only 11 panelists were raters.
The panelists were chosen for their clinical expertise and their administrative influence within VA, which would permit them to provide ratings that were administratively and clinically viable. The panelists represented several different perspectives—psychiatry, internal medicine, specialty medicine, and hospital administration. Individuals' geographical proximity to San Diego, to facilitate panel logistics, also influenced the choice of panelists.
The entire panel was convened for a one-day meeting in January 1997. The meeting began with an overview of primary care (
46), a description of the problem of access to primary care for persons with serious mental illness, and a description of the integrated model of primary care delivery in a mental health setting. Although input from all panelists was welcomed during the discussion, only physician panelists performed the ratings. Eleven panelists (nine men and two women) were physicians. They included five internists, five psychiatrists, and one other specialist, all of whom were active practitioners.
List of conditions. A list of physical health conditions was assembled on the basis of a review of several guidelines for primary care medicine, including those from AHCPR, ACP, and Kaiser. Also used were a book of algorithms related to outpatient medical care, a textbook on ambulatory medicine, and the 12th edition of
Harrison's Textbook of Internal Medicine (
47,
48,
49,
50,
51,
52,
53,
54,
55,
56).
As used here, the term "conditions" denotes not only physical health conditions but also procedures and preventive care measures. A total of 344 such conditions were identified and were subdivided into five categories: preventive screening and counseling, preventive treatment, evaluation of medical conditions, treatment of medical conditions, and procedures. Panelists were asked to consider each condition in the context of an uncomplicated presentation. Several conditions that are clearly the province of psychiatrists or medical specialists were retained in the list to provide face validity for the rating procedure.
Rating system. The appropriateness rating methods developed jointly by Rand and the University of California, Los Angeles, were adapted for use in this study (
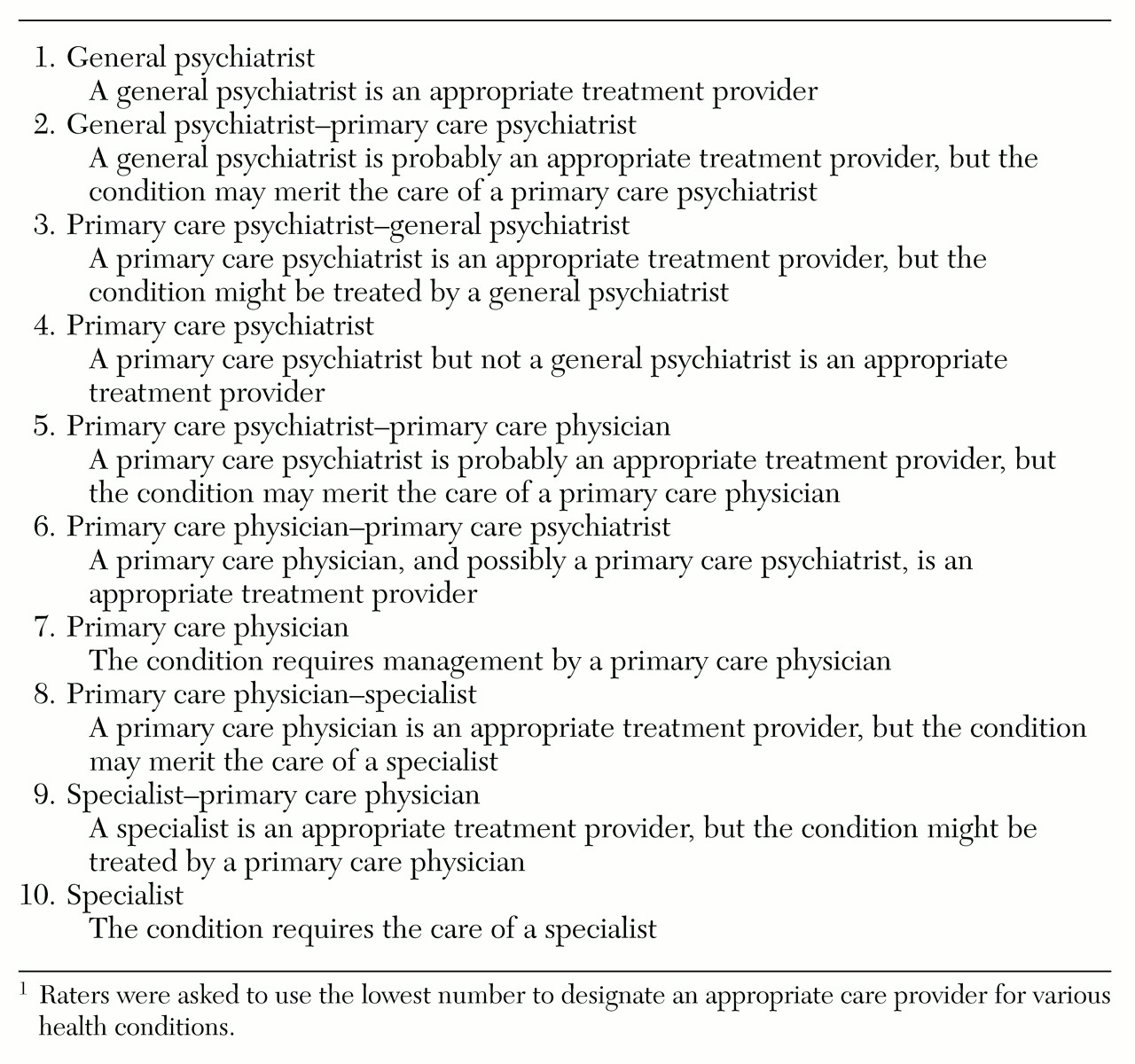
40). At the one-day meeting described above, each panelist was provided with the ten definitions shown in
Table 1. The definitions form a 10-point rating scale, from 1, indicating a condition for which the least specialized (nonpsychiatric) medical training is needed, to 10, indicating a condition that requires care by a medical specialist.
Panelists rated each of the 344 conditions on scannable forms by designating the lowest number that corresponded to the practitioner who might appropriately provide the indicated care. It should be noted that in deeming a psychiatrist an appropriate provider for a condition, the panelists were not making a judgment about who is the most appropriate provider. The forms were scanned, and responses were analyzed using software developed for the rating process.
The second round of rating focused on items for which simple consensus was not achieved. Simple consensus was defined as agreement by eight of the 11 raters (or seven of ten, if one failed to vote) that a psychiatrist with or without primary care training could appropriately address the condition or that an internist or specialist was required. Each condition for which simple consensus was not achieved was discussed by the entire panel and rerated by the 11 raters, after modifications in the description of the condition were made for clarification.
Agreement was defined as all raters agreeing that a psychiatrist (ratings 1 to 5) or an internist (ratings 6 to 10) was an appropriate treatment provider for a given condition. Agreement could be subjected to sensitivity analysis, by first evaluating on which conditions all 11 raters agreed (referred to as 11-rater agreement) and then comparing results with those obtained by discarding the one or two extreme ratings, respectively, at each end of the psychiatrist-internist spectrum (nine- and seven-rater agreement).
Disagreement was defined as at least one rater assigning care to a general psychiatrist (a rating of 1 or 2) and one rater assigning care to a specialist (a rating of 9 or 10). Disagreement can also be subjected to sensitivity analysis, by eliminating the one or two extreme high and low ratings. Ratings can also be evaluated using the central tendency. We report median ratings instead of means and standard deviations because we considered the characteristics of the 1-to-10 scale more consistent with those of an ordinal than an interval scale (
40).
Results
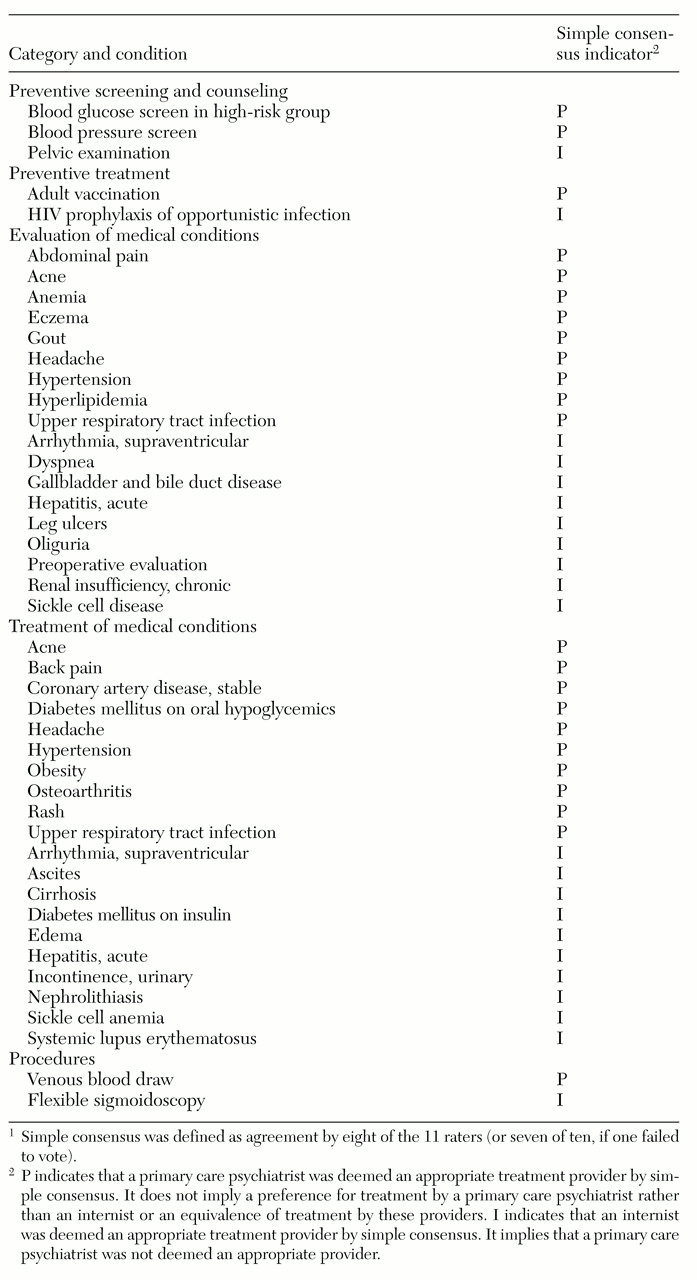
A sample of the conditions for which simple consensus was achieved is shown in
Table 2. (A complete list of ratings for all 344 conditions is available from the authors.) Simple consensus was achieved for 72 percent of all conditions rated (or 246 of the 344 conditions). In the category of preventive screening and counseling, simple consensus was achieved for 92 percent (or 35 of the 38 conditions). The proportions were 43 percent for preventive treatment (three of seven conditions), 69 percent for evaluation of medical conditions (109 of 157 conditions), 69 percent for treatment of medical conditions (86 of 125 conditions), and 77 percent for procedures (13 of 17 conditions).
As defined here, the likelihood of simple consensus being achieved by chance for a given condition—that is, achieved even if the ratings were produced randomly—was fairly high (a 55 percent chance). However, it is extremely unlikely that simple consensus would be achieved by chance for 246 or more of the 344 conditions; the probability is well under one in ten to the 50th power (
57), which provides some face validation of the consensus approach.
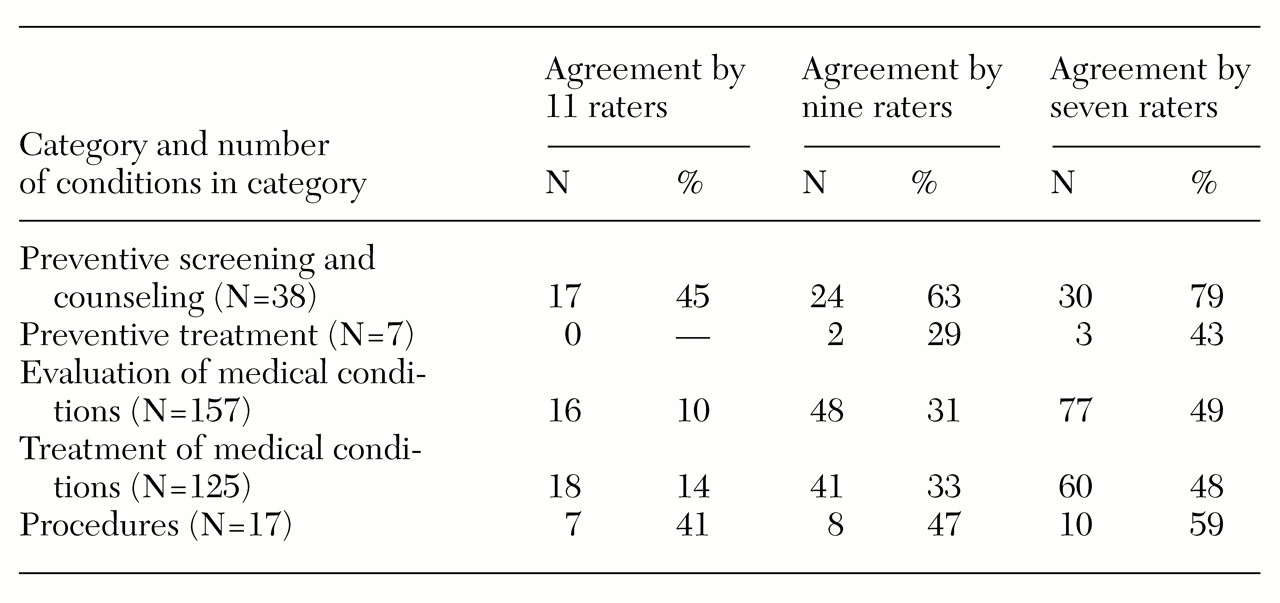
Table 3 shows the level of agreement for the five categories of conditions. A greater percentage of agreement was found for conditions in the category of preventive screening and counseling than for those in the categories of evaluation and treatment of medical conditions. In general, consensus was achieved more often than agreement. Examples of conditions for which all 11 raters agreed about internist or specialist care included evaluation of AIDS, endocarditis, osteomyelitis, acute renal failure, complicated urinary tract infection, ventricular arrhythmias, class III or IV congestive heart failure, and "brittle" or complicated diabetes mellitus. These indications would not therefore be considered appropriate for treatment by a primary care psychiatrist.
As
Table 3 shows, all 11 raters agreed that a primary care psychiatrist would be an appropriate provider for 45 percent of the preventive screening and counseling indications. A primary care psychiatrist was also deemed appropriate by all 11 raters to evaluate alcohol abuse, altered mental status, constipation, insomnia, sleep disorders, and onychomycosis and to treat uncomplicated diabetes mellitus (when the patient is not on hypoglycemic medications), insomnia and sleep disorders, weight gain, and weight loss.
As
Table 3 shows, when a less strict definition of agreement was used, such as nine-rater or seven-rater agreement, a primary care psychiatrist was deemed an appropriate treatment provider for 32 to 61 additional conditions in the evaluation category and 23 to 42 additional conditions in the treatment category.
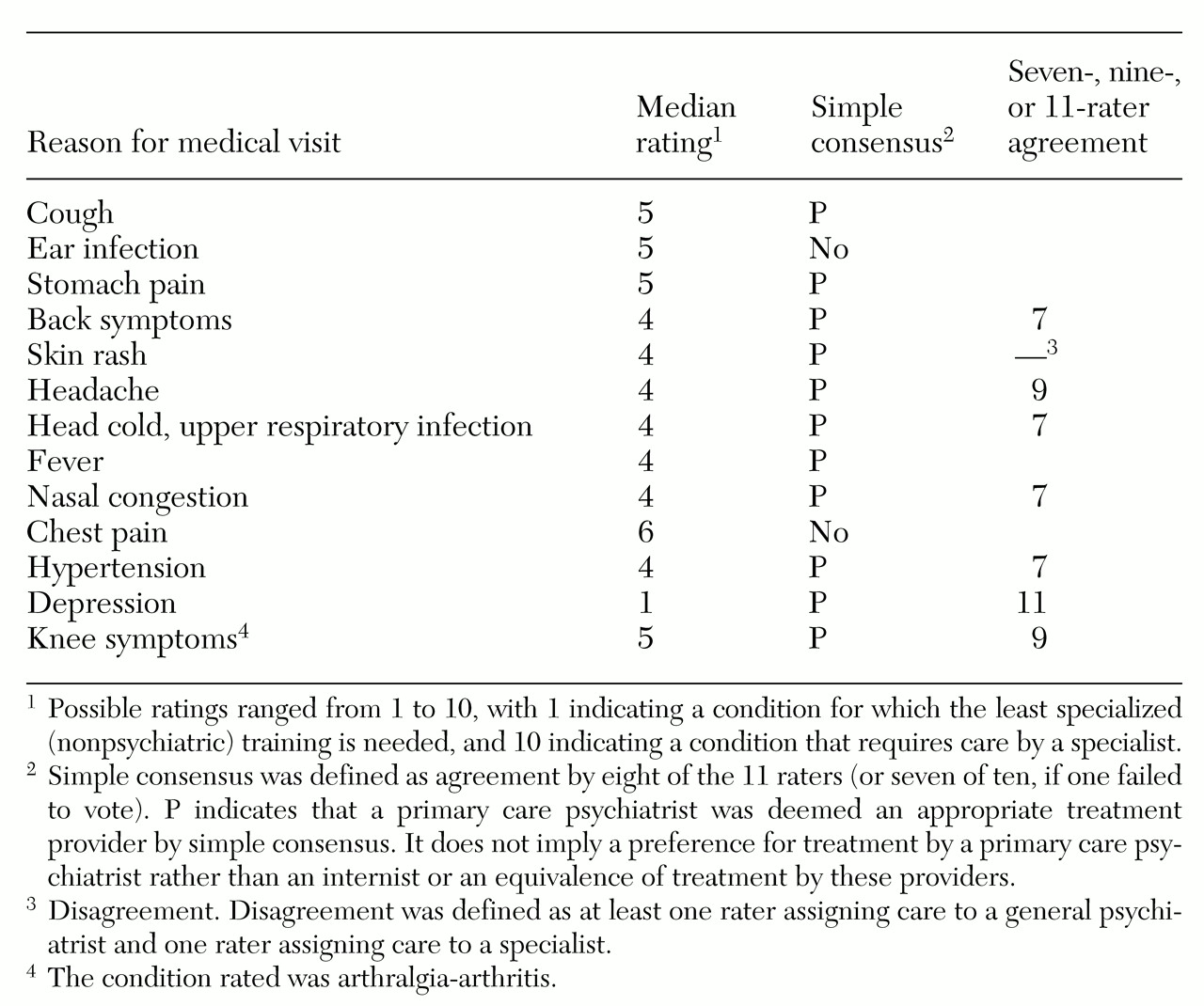
Table 4 shows panelists' ratings for 13 of the 20 conditions reported by patients in a national survey as the most common reasons for their ambulatory care visits (
58). (The seven conditions not rated by the panel were a well-baby examination, a routine prenatal examination, a postoperative visit, a general medical examination, symptoms referable to the throat other than an upper respiratory infection, visual dysfunction, and a progress visit not otherwise specified.) The 20 conditions accounted for 42.2 percent of all ambulatory care visits in the national survey (
58). For 11 of the 13 conditions rated by the panel (85 percent) a primary care psychiatrist was deemed by simple consensus as an appropriate treatment provider. Simple consensus was not achieved for evaluation of chest pain or earache.
For seven of the 13 conditions (54 percent), a primary care psychiatrist was deemed appropriate at the seven-rater level of agreement. For two conditions (15 percent), the nine-rater level was achieved, and for one (7 percent), the 11-rater level was achieved. Although simple consensus was achieved for skin rash, this condition met criteria for disagreement at the 11-rater level.
In general, when the mean ratings of psychiatrists differed from those of internists, with one group deeming a psychiatrist an appropriate provider (median ratings of less than 5) and the other group deeming an internist necessary (median ratings of more than 5), the five psychiatrists on the panel were more likely than the five internists to rate conditions as requiring care by an internist. The sole exception was dizziness-vertigo; psychiatrists rated this condition as appropriate for treatment by a primary care psychiatrist and internists did not.
In its discussion, the full panel concluded that although primary care psychiatrists could competently perform certain intrusive medical procedures such as a digital rectal examination or a pelvic examination, the psychiatrist-patient relationship might be compromised by such procedures. In final ratings, a primary care psychiatrist was deemed appropriate for performing digital rectal examination by simple consensus and at the seven-rater level of agreement. However, a primary care psychiatrist was judged by simple consensus as inappropriate to perform a pelvic examination and a Pap smear.
Discussion
Physician-panelists, representing psychiatry, internal medicine, and one specialty, rated whether a psychiatrist with additional primary care training and access to an on-site internist would be an appropriate care provider for 344 conditions that a person with serious mental illness might present with. Among 13 conditions cited in a national patient survey as the most common reasons for ambulatory care visits, psychiatrists were rated appropriate providers for 11. Panelists expressed specific concerns about procedures that pertain to private body parts.
No research has directly examined the effects of the integration of primary care into the psychiatric setting. This study took the first essential step in evaluating such integrated care, by asking a panel of physicians to systematically assess whether a primary care psychiatrist would be appropriate to deliver care for certain health conditions. The findings provide the framework for future efforts that may seek to implement integrated care for persons with serious mental illness. According to the approach considered here, psychiatrists with limited additional primary care training in conditions for which they are deemed appropriate care providers and who have access to an internist could provide both psychiatric and primary care to their patients.
A key element of the methods used in this study was first asking panelists to rate the various conditions without knowledge of other panelists' ratings. This first step was followed by a discussion and rerating of the items for which consensus was not achieved. In past studies that have used the appropriateness rating methods, panelists have in some instances been provided in advance with available outcome data indicating whether a condition is appropriate for care by a certain type of provider. However, in the study reported here, we could find no existing data about outcomes for persons with serious mental illness treated by psychiatrists or internists. Instead, the purpose of the rating process was to identify conditions of persons with serious mental illness that could appropriately be treated by psychiatrists. It is up to future studies to evaluate outcomes of such treatment.
The results of this study may not be generalizable to settings outside VA. Different results might be obtained for different patient populations or with panelists from health care systems other than the VA system. However, VA is a major provider of care for persons with serious mental illness. Thus findings in this setting remain of widespread interest. Although the panelists came from different VA facilities, all were from Southern California; it is conceivable that panelists from different regions may have made different appropriateness ratings. Moreover, idiosyncratic panel responses and the influences of individual panel members are concerns in any panel process.
Defining who may appropriately provide care for persons with serious mental illness may be of secondary importance to ensuring that adequate time is permitted for care—an issue not addressed in this study. Finally, expanding the role of psychiatrists to include primary care may provoke dissent. However, philosophical disagreement about the theory of primary care psychiatry must ultimately be judged against the effect of primary care psychiatry on the delivery of care; moreover, when primary care psychiatry is implemented, the satisfaction of patients and providers must also be taken into account. Efforts to implement primary care psychiatry and evaluate its outcomes are currently under way.
Acknowledgments
The authors gratefully acknowledge the research and administrative assistance of Brittany Mache, B.A. Financial support was provided by the San Diego Veterans Affairs Medical Center.