Board-and-care homes provide supportive living environments for mentally disabled individuals. These important homes offer asylum to former long-stay mental hospital patients (
1) and other chronically mentally ill individuals (
2). They provide needed supervised living environments (
3) in the absence of family support and an alternative to nursing home placement (
4) and homelessness (
5) among older mentally ill adults. Board-and-care homes offer affordable, supportive, long-term care services in a variety of settings, ranging from small adult foster care homes to large, quasi-institutional hotel-like facilities.
Several factors threaten the well-being of mentally disabled board-and-care residents. To make a profit and stay in business, operators of board-and-care homes face strong economic pressures to reduce operating expenses (
6). Less skilled, lower-wage caregiving staff may provide inadequate levels of support. Residents often lack the power to demand adequate support, given the lack of alternative affordable long-term-care living environments.
The Veterans Administration began a foster home program in 1951, which has evolved into a program that regulates health and safety standards and monitors the well-being of mentally ill veterans discharged from VA medical centers to privately operated board-and-care homes in the community (
16). The community residential care program is a model of a "voluntary" regulatory approach. That is, to promote quality of care in board-and-care homes, VA uses the carrot of a reliable source for new residents, rather than the stick of legal sanctions against the operators.
The study reported here examined the relationship between the receipt of monthly home visits from case managers in a community residential care program and psychiatric hospitalization among 321 veterans followed for up to five years. At some time during the study, all 321 veterans lived in board-and-care homes approved by the community residential care program; two-thirds of them received monthly home visits.
Psychiatric hospitalization was used as an indicator of poor-quality patient care. The vulnerability-stress model of schizophrenia suggests that mentally disabled individuals relapse and are often hospitalized during times of stress when community support is inadequate (
17). Low-functioning mentally ill adults often have lower rates of psychiatric hospitalization after the introduction of intensive case management and community support (
18,
19,
20,
21,
22,
23). Yet we know little about the effectiveness of moderate-intensity community-based case management, such as that provided in the community residential care program, in reducing psychiatric hospitalization among moderately functioning mentally ill adults living in board-and-care homes.
Methods
Study site
The VA West Los Angeles community residential care program is among the largest of more than 100 such programs administered by VA medical centers and outpatient clinics nationwide (personal communications, Van Stone W, Brake S, Apr 2000). The average daily census of the program is 290 veterans residing in 24 privately operated board-and-care homes approved by the community residential care program. The homes are located within a ten-mile radius of the VA West Los Angeles Healthcare Center in the cities of Los Angeles and Santa Monica.
As of October 1999, program staff consisted of nine case managers, five of whom were community health nurses (registered nurses) and four of whom were master's-level social workers. Six of the nine case managers split their work time between the community residential care program and other work assignments at the West Los Angeles Healthcare Center. Case managers were assigned to monitor one to five board-and-care homes, or 2.7 homes on average. The number of facilities monitored by each case manager ranged from one to five homes. When a case manager was assigned to a facility, all of the veterans living in that facility became part of his or her caseload. On average, a case manager visited 28 mentally ill veteran patients living in board-and-care homes each month. Caseloads ranged from four to 60 veterans.
The community residential care program was compared with three case management models— outpatient clinics, community-based treatment, and assertive community treatment— using the Community Practice Philosophy Scale (CPPS) (
24). The community residential care program was found to be more intensive than outpatient clinic programs and less intensive than both community-based and assertive community treatment programs. The community residential care program was comparable to outpatient clinic programs in the degree to which it resembled assertive community treatment programs. In four of the five CPPS subscales used to define similarity to assertive community treatment, scores for the community residential care program were lower than those for community-based programs and much lower than those for assertive community treatment programs.
The community residential care program used an individual treatment approach rather than a team approach. Case managers in this program rarely provided emergency services themselves, did not dispense medication, and were not available to assist clients outside of normal business hours. The single aspect of the community residential care program that was similar to assertive community treatment was its emphasis on maintaining long-term regular contact with most clients.
Sample
The sample included all patients of the VA West Los Angeles Healthcare Center identified on September 7, 1998, by hospital records as living in a board-and-care home approved by the community residential care program (N=321). Based on program records, 214 of these patients were participants in the community residential care program.
The remaining 107 patients made up the comparison group. Some of the comparison group patients had moved from a board-and-care home before the home was approved by the community residential care program and did not advise hospital staff of their change in address. Others lived in the approved home without the case manager's knowledge; this situation was more likely for those living in larger, hotel-like facilities. Still others in the comparison group received home visits so infrequently that the case manager failed to add their names to the patient roster of the community residential care program.
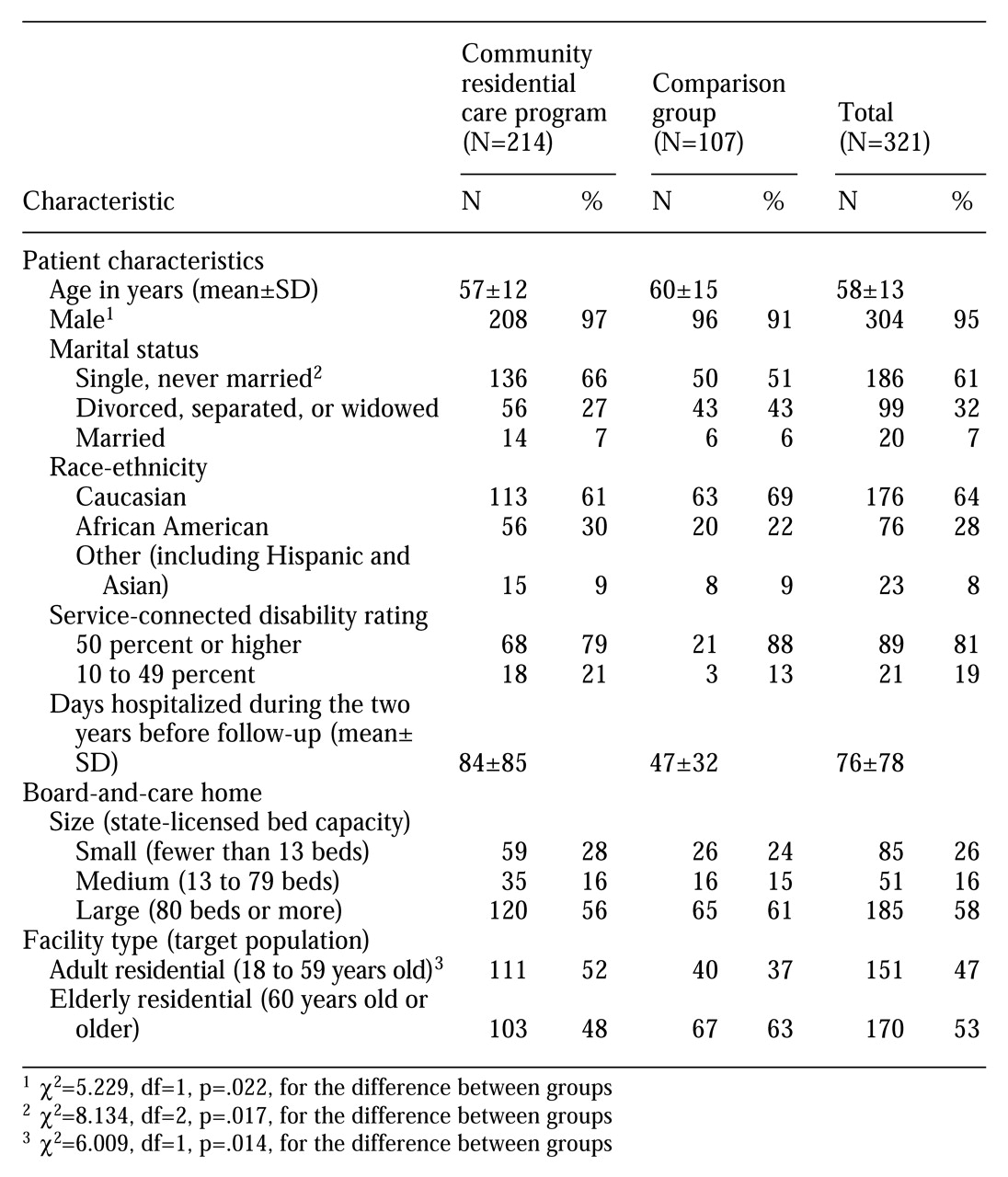
Table 1 presents characteristics of the total sample and of subjects in the community residential care program and the comparison group. The typical subject was a 58-year-old Caucasian male who had never married and had been hospitalized on a psychiatric or substance abuse ward for 76 days during the two-year period preceding the study. More than half of the subjects lived in a large board-and-care facility with more than 80 beds that was licensed to care for elderly persons.
As
Table 1 shows, subjects in the community residential care program were less likely to be female (3 percent versus 9 percent), and were more likely never to have married (66 percent versus 51 percent). The groups appeared to be comparable with respect to the size of the board-and-care facility, race-ethnicity, service-connected disability ratings, and previous psychiatric hospitalization.
Procedures
The dates for the start of follow-up were determined for the 214 subjects in the community residential care program and the 107 subjects in the comparison group. The dates for the subjects in the residential care program were based on the date of their first monthly home visit in the program. Subjects in the comparison group were matched to subjects in the program once the follow-up start dates were established for program subjects. Matching was based on the size of the facility they lived in— fewer than 13 beds, 13 to 44 beds, 45 to 98 beds, 99 to 120 beds, and 121 beds or more. They were also matched on age (under age 45 years, 45 to 49, 50 to 54, and so forth up to 85 years or older).
Ninety-six of the 107 comparison subjects could be matched to one or more subjects in the program. The comparison subjects were given the same start date as their matched counterparts. The remaining 11 comparison subjects were assigned the median start date for the program subjects— May 1, 1994.
Psychiatric hospitalization data for ten years, 1989 to 1998, were collected for all subjects. Psychiatric hospitalizations, including substance abuse treatment, were categorized according to the ward from which the patient was discharged. Twenty different inpatient wards were included. Information about patients' sociodemographic characteristics, their treatment in the community residential care program, and the facilities where they lived was collected from several secondary sources, including hospital and program records and state licensing records of board-and-care homes.
Variables
Two independent variables were used— group status (community residential care program versus the comparison group) and duration of home visits in the community residential care program (the number of months subjects received consecutive monthly home visits). We hypothesized that program subjects would be less likely to be hospitalized because of case managers' ability to identify acute stressors during home visits and to intervene before patients relapsed and required hospitalization. Case manager-patient rapport requires time to develop. Regular visits by interested persons to residents of institutional settings have been associated with improved quality of care provided by facility caregiving staff (
25).
A two-part measure of hospitalization was used— psychiatric bed days and recidivism. Recidivism was defined as readmission to an inpatient psychiatry or substance abuse treatment ward after the start of follow-up. We view psychiatric hospitalization as a negative event, which could— and should— be prevented through supportive community living environments and effective mental health outpatient treatment delivered as close to the individual's residence as possible. Although this view is shared by many mental health professionals and advocates for the mentally ill, there are some who argue that psychiatric hospitalization is both necessary and beneficial to mental health consumers (
26).
Ten moderating variables were used, including one community residential care program variable (the case manager's profession), one variable related to the board-and-care environment (size of the facility), and eight patient characteristics (age, marital status, race-ethnicity, family support, psychiatric diagnosis, substance abuse comorbidity, income, and eligibility for VA disability benefits). The variable on the case manager's profession was included because differences between social workers and community health nurses in professional training and associated practice orientations might have influenced patient outcomes, and thus the analyses adjusted for that variable.
Previous studies have found that patients living in smaller homes adjust better and become more integrated into the community than those living in larger homes (
27,
28). Also, older married individuals from ethnic minority groups diagnosed as having schizophrenia with comorbid substance abuse have been found to be at greater risk for relapse and rehospitalization than others (
29). The income variable was used because the lack of financial resources typical among mentally ill individuals makes coping with life stressors more difficult, thereby increasing the risk of relapse.
Finally, veterans whose mental illness has been judged to be more than 50 percent connected to their military service have better access to VA mental health care and might be readmitted to the hospital more readily than veterans whose mental illness is not service connected. Veterans suffering serious mental disability as a result of mental disorders sustained during or resulting from active military duty are afforded the right to psychiatric hospitalization as needed; psychiatric admission of other veterans is largely discretionary— that is, not solely a function of need.
Analysis
Use of inpatient services. Mann-Whitney independent-samples tests were used to compare the community residential care subjects and subjects in the comparison group on the median number of bed-days used during the two years before and after the start of the follow-up. Utilization gain scores were also compared between the two groups. Gain scores were calculated by subtracting the number of bed-days used in the second two-year period from the number used in the first. Wilcoxon signed-ranks related-samples tests were used to compare changes in median bed-day use over time for each group. Nonparametric tests were chosen because the outcome (use of psychiatric bed-days) was quite skewed, and we prefer the more intuitive interpretation of nonparametric findings to the interpretation of parametric findings resulting from log-transformed, or otherwise transformed, more normally distributed outcomes.
The two-year period before and after the start of follow-up was selected to balance a maximal sample size with a reasonable observation period. Measurement of less frequent events, such as psychiatric hospitalization, requires longer follow-up periods to obtain adequate numbers of case events for statistical analysis. Two years is a commonly used observation period for hospital recidivism in studies of outcomes of case management for mentally ill adults (
18,
19,
20,
21,
22). All subjects were observed for the entire two-year period after the start of follow-up.
Subjects not hospitalized during the two-year periods before and after the start of follow-up were excluded from the analysis to avoid median bed-day findings of zero; a majority of subjects were not hospitalized during the two-year periods. Only bed-days used during the two periods were counted; if a patient's hospitalization extended beyond the cutoff points in either direction, those days were not counted. For subjects who had multiple psychiatric hospital stays, bed-days were summed for the entire period. Group medians were calculated on the basis of individual bed-day totals for both periods.
Recidivism. Two logistic regression models were used to predict recidivism, defined as the first readmission to a psychiatric or substance abuse treatment ward after the start of follow-up until August 31, 1998. The first model included all 321 subjects. In this model, recidivism was regressed on group status— the community residential care group versus the comparison group; the analysis adjusted for factors for which data from hospital and other records were available for all 321 subjects. These factors included size of facility, age, marital status, race-ethnicity, and eligibility for VA disability benefits. The backward conditional method of entry was used.
The five covariates were dichotomized to increase statistical power, given the low rates of hospitalization. The size of the facility, fewer than 80 beds versus 80 beds or more, and patients' age, less than 62 years versus 62 years or older, were dichotomized on the basis of median values for all subjects. Marital status was dichotomized as never married versus ever married, race as minority group member versus Caucasian, and eligibility for VA disability benefits as a 50 percent or higher service-connected disability versus a service-connected disability of less than 50 percent. These covariates were either known risk factors for recidivism (larger facility, younger age, never-married marital status, and minority racial-ethnic status) or were believed to be a risk factor (eligibility for VA disability benefits).
A second logistic regression model was used to predict recidivism among subjects in the community residential care program only, taking advantage of additional data on these subjects from the program's administrative records. In this model, recidivism was regressed on the duration of home visits from staff of the community residential care program. The duration was dichotomized as less than two years and two years or longer. We decided on the two-year cutoff after the study was completed. Five exploratory models were run for the community residential care subjects only, with the duration of home visits ranging from one to five years. The results for durations of two through five years were nearly identical, suggesting that patients' risk of recidivism changed little after they received home visits for two years.
This model was adjusted for several factors in addition to those adjusted for in the model that included all subjects. The additional factors were the case manager's profession, the subject's income, presence of family support, psychiatric diagnosis, and substance abuse comorbidity. As in the first model, all covariates were dichotomized— community health nurses versus social workers, income of less than $10,000 (the median) versus income of $10,000 or more, minimal family support as assessed by the case manager, a diagnosis of schizophrenia or schizoaffective disorder versus all other diagnoses, and the presence or absence of a diagnosed substance use disorder. Family support, psychiatric diagnosis, and substance abuse were evaluated by case managers using intake forms of unknown reliability and validity from the community residential care program.
Results
Inpatient utilization
Among the 214 subjects in the community residential care program, 45 (21 percent) were hospitalized during the two years before the start of follow-up. The number hospitalized increased slightly to 49 (23 percent) during the two years after. Among the 107 comparison subjects, 12 (11 percent) were hospitalized in the two years before the start of follow-up and 24 (22 percent) in the two years after. Thus hospitalization rates remained essentially unchanged for the community residential care group and doubled for the comparison group.
Hospitalized subjects from the community residential care program used a total of 3,798 psychiatric bed-days during the first two-year period and 3,170 in the second period. The mean±SD length of stay among subjects in the program decreased from 84±85 days in the two years before the start of follow-up to 67±71 days in the following two-year period. Subjects in the comparison group used a total of 562 bed-days in the first period and 2,004 bed-days in the second period. The average length of stay for comparison subjects increased between the two periods— from 47±32 to 84±97 days.
Among subjects in the community residential care program, the distribution of total bed-days used ranged from seven to 429 days during the first period and from two to 319 days during the second period. Among comparison subjects, the distribution ranged from five to 113 bed-days during the first period and from 12 to 413 bed-days during the second. Thus variation in bed-day use among hospitalized subjects in the community residential care program decreased modestly between the two periods, while it increased dramatically among comparison subjects.
Between the two periods, the median per capita number of psychiatric bed-days decreased from 59 to 50 days for the community residential care group (Z=-2.126, N=45, p=.033) and increased from 42.5 to 49 days for the comparison group (Z=-.845, N= 12, p=.398). The per capita utilization for the two groups appeared to converge during the two years after the start of follow-up; the difference between groups in the first two-year period was 16.5 days, which decreased to one day in the second two-year period. Neither difference was significant.
Analyses between groups and between time periods among all subjects showed no differences or changes. Because hospitalization was rare in the sample, median values for both groups during both time periods were zero. However, the community residential care group had a larger gain score for hospital utilization than the comparison group (score of 165 versus 154; Z=-1.901, N=321, p= .057). These scores further suggested a greater decline in inpatient utilization among subjects in the program.
Predictors of hospitalization
Seventy-six of the community residential care subjects (36 percent) and 47 of the comparison group subjects (44 percent) were hospitalized at least once during the follow-up period. Among hospitalized subjects, the median time to first psychiatric hospitalization was 322 days for subjects in the community residential care group and 389 days for comparison subjects.
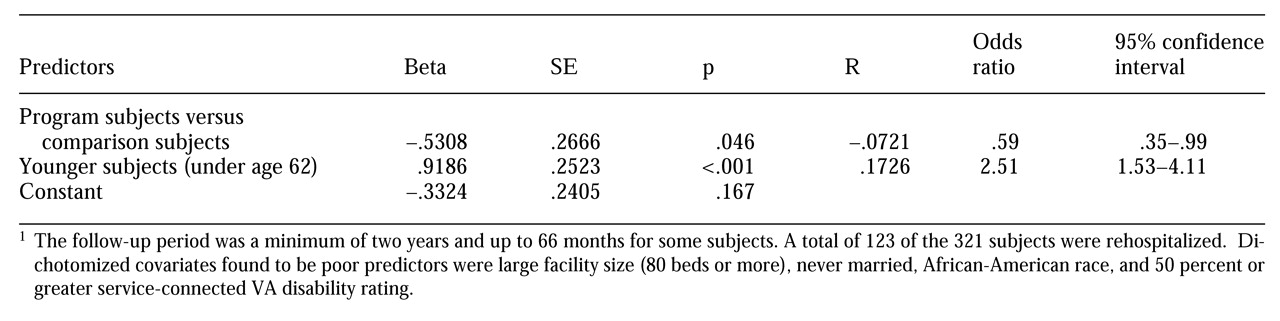
Table 2 presents results from the logistic regression model predicting psychiatric hospitalization among the total sample of 321 subjects. Group status and subjects' age were significant predictors of rehospitalization. During the follow-up period, subjects in the community residential care program were hospitalized about half as often as comparison subjects (odds ratio=.59), after the analysis adjusted for size of the board-and-care facility, age, marital status, race-ethnicity, and eligibility for VA disability benefits. Subjects under age 62 were hospitalized 2.51 times more often than subjects age 62 or older.
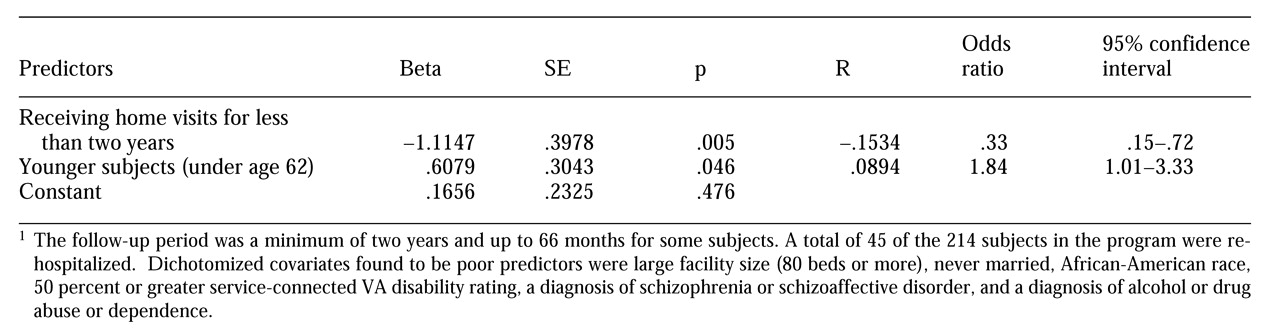
Table 3 presents results from the logistic regression model predicting psychiatric hospitalization among the 214 subjects in the community residential care group. The duration of home visits and subjects' age were significant predictors of psychiatric hospitalization. Subjects receiving home visits for a period of less than two years were hospitalized about one-third less often (odds ratio=.33) during the follow-up period than those receiving home visits for two years or more. Subjects under age 62 were hospitalized 1.84 times more often than those age 62 or older.
Discussion
Hypothesis
The findings generally support the hypothesis that subjects who received monthly home visits would be hospitalized less often than those who did not receive such visits. The findings on inpatient utilization suggest that subjects in the community residential care group who received home visits reduced their use of psychiatric bed-days from the two years before the intervention to the two years after. The number of bed-days used by subjects in the comparison group did not change significantly. Results of the logistic regression analysis showed that comparison subjects were hospitalized 1.5 times more often than subjects in the community residential care program, when the analysis adjusted for patient and facility characteristics.
The predictive power of most of the covariates was poor. Five of six covariates in the model that included all the subjects and ten of 11 covariates in the model that included the community residential care subjects failed to predict hospitalization. Age was the only significant predictor. The poor predictive power of most of the covariates suggests that characteristics of the facility and of the community residential care program may be relatively unimportant in predicting hospitalization among veterans receiving monthly home visits. Also, effect sizes related to facility and program characteristics may be small. Finally, other variables related to the facilities and the program that may have been significant predictors were not included in the full logistic regression model.
Of these possibilities, the first is least likely, given the increasing evidence that residential treatment environments (
30) and community-based case management interventions (
22,
29) do influence the outcomes of mentally ill patients. Future studies of rare outcomes such as hospitalization may be better able to detect small effects if they use more efficient study designs, such as a case-control design, and larger samples.
Subjects in the community residential care program who received home visits for more than two years were three times more likely to be hospitalized than subjects in the program who received home visits for less than two years. This finding was unexpected. Possible explanations for it include historical bias, information bias, and the natural history of schizophrenia. Reduced hospitalization among patients who had been in the program for less than two years may have resulted from the decreasing supply of psychiatric beds and the increasingly stringent psychiatric admissions policies implemented between 1993 and 1998. The year of entry into the program was not controlled for statistically, and thus changes in the external environment other than the program intervention may have introduced historical bias.
Information bias may also explain this finding. Patients who had been in the program a short time may have been more likely to be hospitalized somewhere other than West Los Angeles VA Medical Center after they moved from the approved board-and-care home and left the community residential care program. Data on psychiatric admissions for these patients may have been less available than data for patients who had received program services for more than two years. Finally, the episodic nature of schizophrenia— the most common diagnosis among patients in the program— may also explain why patients who had received program services for a longer time were more likely to be hospitalized. Many patients in the program are placed in a board-and-care home and enter the program from an inpatient stay in a psychiatric or substance abuse ward. It may be that a typical patient in the program does not relapse to the point of requiring psychiatric admission until he or she has been in the program for more than two years.
One of the most consistent findings was that younger subjects— those under age 62— were hospitalized two times more often than older subjects. This finding is both consistent with the literature and surprising. Among those diagnosed with a mental disorder, younger individuals are more likely to be hospitalized than older individuals (
29). What is surprising is that our younger patients remained at risk, even when "young" was defined as under age 62. This finding suggests that veterans may be an at-risk population for psychiatric recidivism compared with the general population, in which recidivism tends to drop off beyond age 40 to 45.
Limitations
Although the findings of this study suggest that the West Los Angeles community residential care program helped reduce psychiatric hospitalization, these findings should be considered tentative given the many limitations of the study. First, differences between the community residential care group and the comparison group in several baseline characteristics suggest the potential for selection bias. The relatively small number of mentally disabled veterans living in board-and-care homes precluded the use of matching techniques commonly used to reduce selection bias in retrospective observational studies.
Another limitation is the possibility of information bias. Information in the hospital computer system, the source for information about patients' addresses used to develop the sampling frame for the study, is not regularly updated. Also, case managers likely were less attentive to documenting home visits in the earlier years of the program. To the extent that differences between the groups and errors in hospital records may have introduced systematic biases, the findings of this study should be considered tentative.
A third limitation is the use of hospitalization as the only outcome. This outcome is an imperfect indicator of poor patient well-being. For example, patients in the community residential care program may have been hospitalized more often than patients in the comparison group because they were monitored more closely by mental health professionals. The higher rate of hospitalization would not necessarily mean that patients in the program were worse off. The need for hospitalization among patients in the comparison group might have gone undetected longer, which may have resulted in comparison patients getting in trouble with the law, leaving the area and being hospitalized somewhere else, or suffering some other negative consequences. Several clinical and system outcomes should be included in future evaluations of community residential care and other moderate-intensity case management programs.
The external validity of the study is quite limited. Veterans differ from the general population in many ways. They are typically older, more likely to be non-Caucasian, and much more likely to be male. Also, the findings may not be generalizable to other VA community residential care programs or other VA health care centers given the considerable variation in setting, organizational, and patient characteristics found in the VA system. Outcome studies of similar interventions at other public hospitals and VA health care systems are needed to establish the generalizability of the findings.
Despite these limitations, the findings of this study advance the current state of knowledge about the effectiveness of a moderate-intensity community-based case management program serving moderately functioning, older mentally ill adults living in privately operated board-and-care homes. The generally positive findings of this study and the findings of other recent studies of this innovative community-based case management program (
31,
32) indicate a need for more rigorous evaluations. The program may give mental health care providers a less costly alternative to more intensive case management that could support moderately functioning mentally ill patients living in privately operated board-and-care homes or other types of residential care facilities.
Until changes are made in the economics and politics of public monitoring and regulation of board-and-care homes, voluntary regulation and regular monitoring of these facilities by influential mental health providers, such as VA, may be the most effective way to prevent relapse and hospitalization and promote the well-being of mentally ill patients living in community residential care settings.
Acknowledgments
The study was funded by the Cheaspeake Health Education Program of the Maryland VA Health Care System. The authors acknowledge Robert Friedman, Ph.D., M.S.W., for assistance in understanding the community residential care program and designing the study; Lee Ochotorena, B.S.N., for help with data gathering; Michael Mitchell, Ph.D., for assistance with data analysis; and Ted (A. E.) Benjamin, Ph.D., Susan Cochran, Ph.D., and Wendy Belcher, Ph.D., for thoughtful comments on drafts of this paper.