However, the cost to families of care for children may be very high even though a child's care is covered by insurance—for example, if their insurance plans include high copayments, dollar limits on coverage, and explicit limitations or exclusions. The Mental Health Parity Act of 1996 (P.L. 104-204) was designed to improve behavioral health coverage by bringing it more into line with traditional medical coverage. However, federal parity legislation addressed only some expenditure limitations. It did not address other coverage issues that may create problems for children's access to behavioral health services.
In this article we present the results of a retrospective review of a sample of private, employment-based behavioral health plans to illustrate the types of restrictions on benefits, services, and diagnoses that are relevant to children's behavioral health care. We also discuss the implications and appropriateness of these limitations and exclusions.
Methods
We examined 128 behavioral health plans administered by one of two large managed behavioral health organizations. Although employers chose the health plans from standard products managed by these organizations, they could customize the attendant benefit limits and service and treatment exclusions in accordance with their own objectives.
Forty-six plans, with 496,911 covered lives, were selected from 71 contracts with Magellan Behavioral Health. These 46 plans were selected because they were in effect for the entire 1996 calendar year, had stable enrollment, and enrolled at least 1,000 employees each. Eight-two plans, with 118,780 covered lives, were randomly selected from 1,787 United Behavioral Health managed care plans that were in effect in 1998. Collectively these plans covered residents of all 50 states. Data on service and treatment exclusions and benefit limits were obtained for each plan. The limits and exclusions discussed here are those relevant to children's behavioral health care, but they applied to all enrollees in the plans.
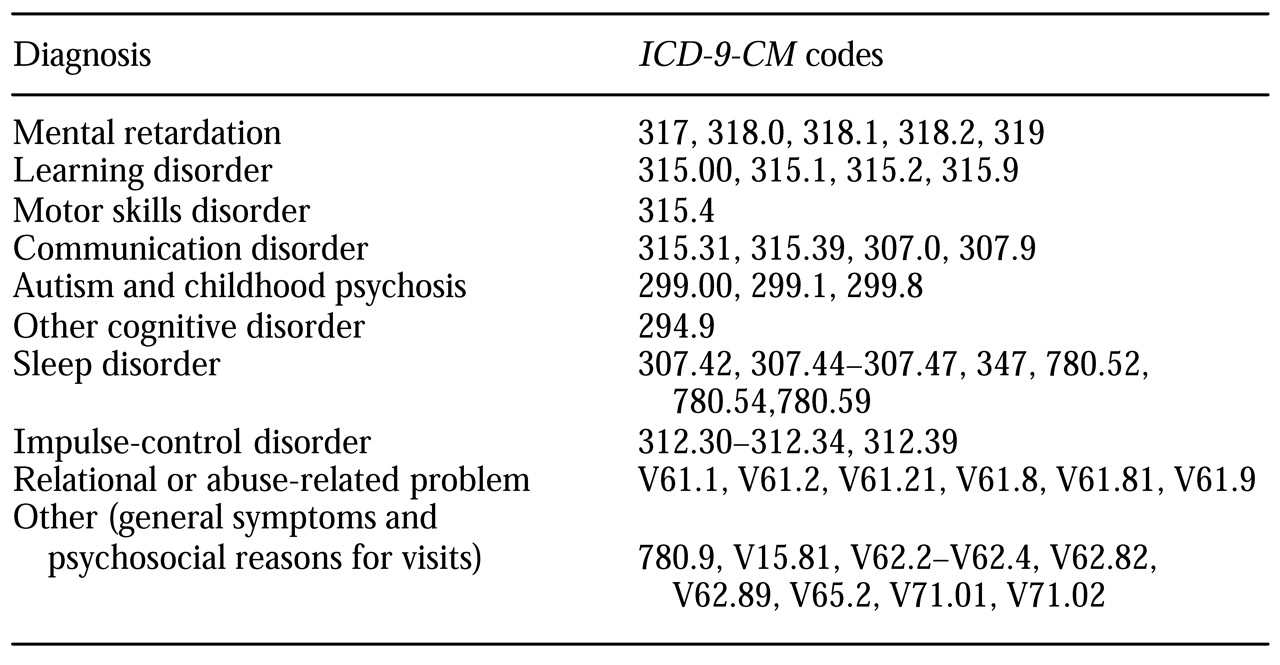
A diagnostic exclusion is defined as any diagnosis that is explicitly excluded from insurance coverage. Services rendered explicitly for an excluded diagnosis are not covered by the plan, even if the same services would be covered if rendered for other diagnoses. Only the plans that were in effect in 1996 contained explicit diagnostic exclusions, all of which were still in effect in 2000. A treatment or service that is excluded from insurance coverage is not covered for any diagnosis.
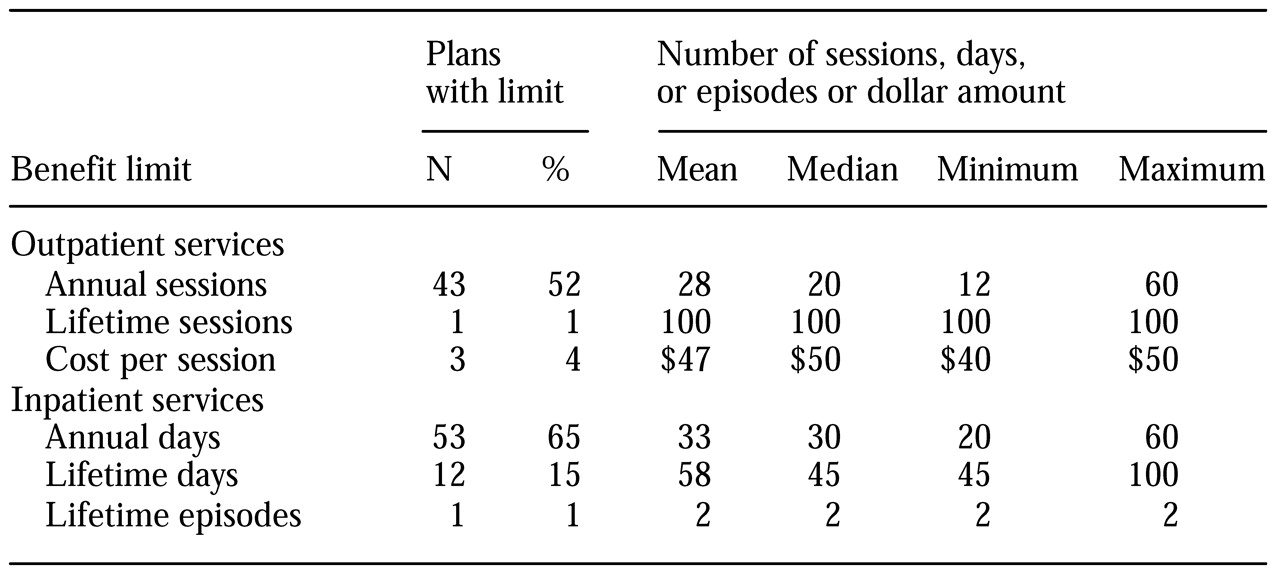
Benefit limits are defined as restrictions on the amount of treatment that will be covered by the plan. These limits can be specified as annual and lifetime restrictions on inpatient and outpatient care, expressed in terms of units such as number of inpatient days or number of outpatient visits, or expressed in terms of a dollar amount. We do not present information on limits contained in the 1996 plans, because the passage of the Mental Health Parity Act in 1996 has made them less relevant.
Discussion and conclusions
We have presented information on a sample of plans from large self-insured employers to illustrate the nature of benefit limits and exclusions of treatments, services, or diagnoses that are applicable to children's behavioral health insurance. Our findings on benefit limits are similar to those observed in a national sample of behavioral health plans (
2). Although we are not aware of any published reports or lists of service and diagnostic exclusions, we expect that the plans reported on here are not atypical.
Behavioral health plans have three distinct types of restrictions on coverage that can affect care for children and influence the children's insurers: diagnostic exclusions, service exclusions, and benefit limitations. Diagnostic exclusions limit the scope of an insurance plan by identifying conditions that are not covered. Excluding disorders such as mental retardation, developmental disorders, and relational or abuse-related problems might have serious consequences for children and thus merits some discussion. A recent review of the literature on child abuse showed that children who are abused are at high risk of adverse psychological sequelae but that timely psychological services for these children may offset the need for intensive therapy by preventing more severe conditions (
3). Frequently the onset of impulse control disorders, such as kleptomania and pyromania, is during childhood. The explicit exclusion of these disorders calls into question the ability of providers to deliver new and promising treatments to children diagnosed as having such a disorder.
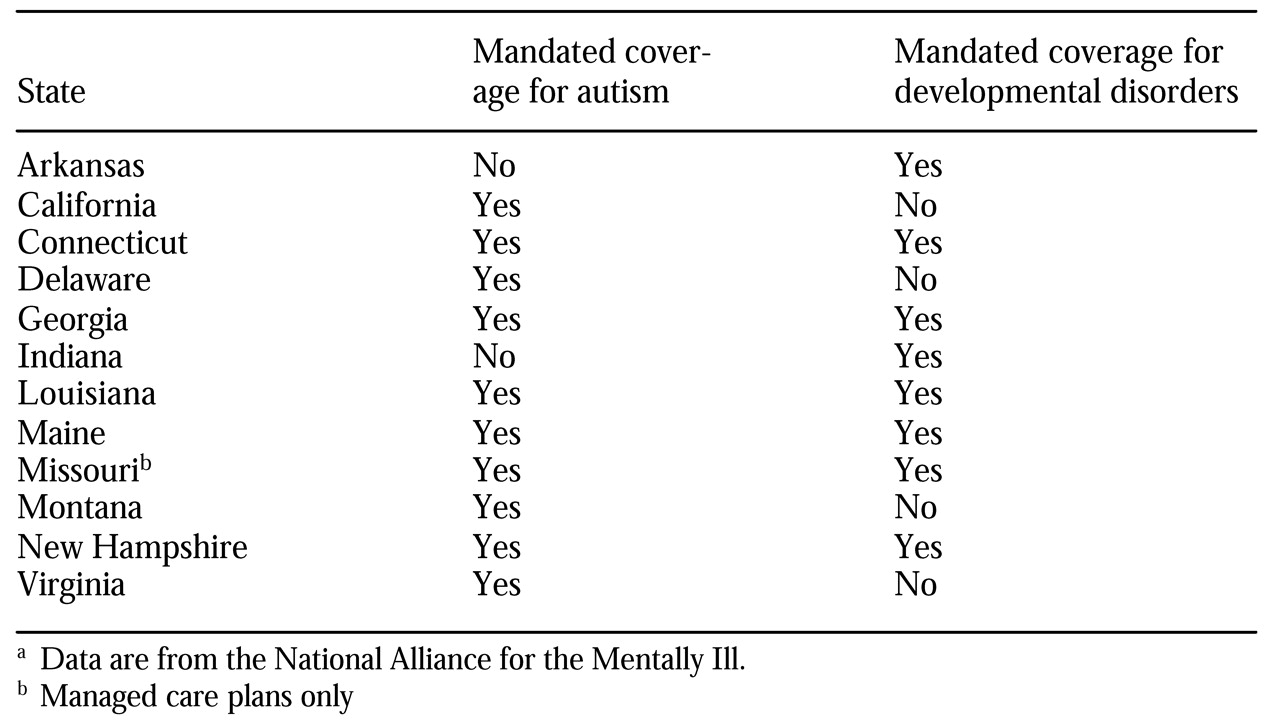
Developmental disabilities among children range from the most pervasive disorders, such as autism, to various degrees of mental retardation. The fact that exclusion of these diagnoses from health insurance coverage presents problems for children's care is reflected in the enactment by 12 states, listed in
Table 4, of legislation mandating coverage for these diagnoses in behavioral health plans. Legislation is pending in several other states, including Iowa, Kansas, New York, and Massachusetts, that would require behavioral health plans to cover specific childhood diagnoses. However, plans offered by self-insured employers, such as the plans in this study, are often exempt from such mandates under the Employee Retirement Income Security Act (ERISA), which may explain the apparent lack of compliance among the plans we studied.
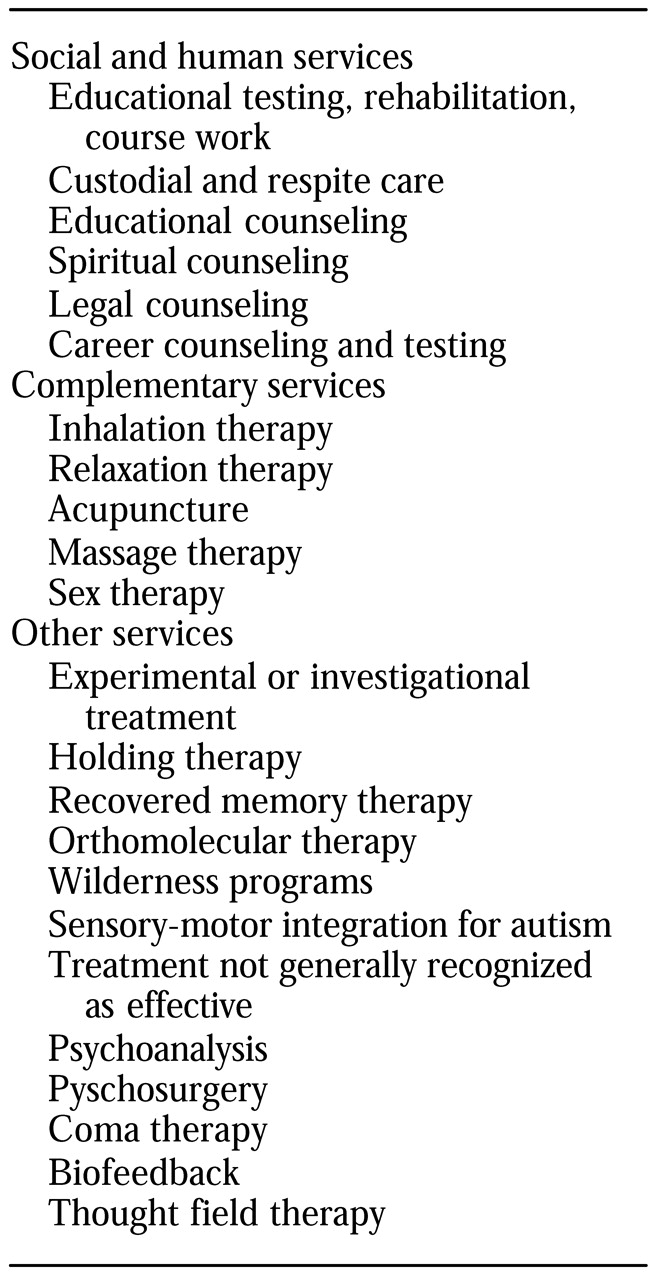
Service exclusions limit the scope of insurance coverage and raise questions about what types of services should be covered by behavioral health insurance. Many of the services excluded in the plans in this study, such as legal counseling and educational testing, can logically be categorized as social and human services. Should such services be covered under behavioral health insurance, or are they more appropriately the responsibility of individuals themselves or of other branches of society, such as the school system or the courts? Some services, such as recovered memory therapy and coma therapy, conceptually belong in the domain of behavioral health care, but their effectiveness has been questioned. We suggest that services that are unique—those for which there is no substitute—and that are also known to be effective should be covered.
Benefit limits that restrict the number of days or visits have been found to affect children disproportionately—children are more likely than adults to exceed the limits (
4). Benefit limits can result in loss of insurance coverage before a course of treatment is complete. For example, treatment for children who have chronic mood disorders often involves a long treatment course—eight months on average, according to one study (
5)—before recovery is achieved, along with follow-up treatment to prevent relapse. Thus a treatment course of 12 sessions—the maximum number of outpatient visits covered under some of the plans we studied—is not likely to result in adequate care for such children.
Traditional medical health insurance has used restrictions on lifetime dollar expenditures rather than on the number of inpatient days or clinic visits. Although expenditure limits in behavioral health plans may increase at some time in the future as a result of federal parity legislation, the use of limits on the number of days or visits—as we observed in the plans in effect in 1998—perpetuates inequities in coverage between mental and physical health plans. Parity in expenditures between mental and physical health plans is consistent with the letter but not the spirit of the Mental Health Parity Act of 1996. Some states have addressed this inequity. Louisiana, Maine, Nevada, South Dakota, and Tennessee have enacted laws that require plans to provide a minimum number of days, visits, or both. Georgia, Nebraska, and New Jersey have laws mandating true equality in benefit limits between physical and mental health coverage. However, self-insured plans are exempt from these mandates under ERISA provisions.
Health insurance generally increases the affordability of children's behavioral health care, but the presence of benefit limits or diagnostic exclusions can mean that some children effectively become uninsured if they require more intensive services than those covered under the plan or if they need treatment for disorders that are excluded under the plan. Although current utilization management strategies employed by managed behavioral health organizations, through which few patients ever reach their benefit limits, render benefit parity almost irrelevant, some children do exceed their benefit limits (
4,
6,
7,
8). The cost of obtaining uncovered services can be very high, because the price of services that are not billable to an insurance plan can be significantly higher than payments for those same services under negotiated agreements between insurers and providers.
Children who exceed their benefit limits face significant access problems. An important but often overlooked fact is that children enrolled in employment-based health plans who use up their insurance benefits are generally ineligible for public assistance on the grounds that their parents are gainfully employed. Limits and exclusions in behavioral health plans not only can affect the affordability of care for children but also raise questions about the purpose and appropriateness of insurance coverage.
That some children need a wide range of services to treat or manage their mental health conditions is not in question. What is in question is which of these services should be financed through behavioral health insurance and which should be the responsibility of physical health insurance plans, individuals, or other sectors of society. Debates about who is responsible for providing services—both behavioral health management services and more typical family services—to these children are not likely to be easily resolved. The absence of any real discussion of this question perpetuates the use of lists of services explicitly excluded by behavioral health plans.
The use of diagnostic and service exclusions can be justified only in the absence of the case-by-case management that was the promise of managed care. The wholesale adoption of managed care plans by employers is proof that they value managed care. The persistent retention of supply-side constraints—such as the exclusions and limits discussed here—in employer-sponsored health plans shows that employers do not trust managed care to fulfill its promise of providing necessary services.
The focus of advocates and lobbyists on benefits parity to the exclusion of the fundamental question of which services should be provided by behavioral health plans makes their efforts seem off target. Frank and McGuire (
7) and Burnam and Escarce (
8) have recommended shifting the focus toward equity between physical and behavioral health care, which would redirect attention to broader issues of access to effective and needed services rather than maintain a narrow focus on equality of benefits between physical and behavioral health services. However, parity legislation, although important in ensuring mental health coverage, is unlikely to keep pace with the changing world of managed care. Future studies should examine the appropriate scope of behavioral health services for children.