Use of medical care tends to decrease after the onset of a psychiatric illness (
1). Even among patients who seek treatment—for mental or physical conditions—medical disorders often are not detected. Some characteristics of psychiatric patients may contribute to missed diagnoses, such as an impaired ability to verbalize concerns (
2,
3,
4,
5), poor insight into illness (
5), denial of illness (
3), or an unwillingness to see a physician other than their psychiatrist (
2). Patients with severe mental illnesses such as schizophrenia and bipolar disorder have an unusually high tolerance for physical pain (
4,
5); if such patients delay communicating their discomfort until the pain caused by a medical illness is severe, interventions may not occur until the illness has progressed to advanced stages (
4). These problems may be exacerbated when multiple clinicians care for the same patient. Both psychiatrists and primary care practitioners provide treatment according to their specialty and may assume that other providers are doing the same. Unfortunately, patients still fall through the cracks (
3).
Of particular concern are people with severe mental illnesses, who frequently have unidentified or untreated medical conditions (
6). Research has demonstrated that 25 to 80 percent of patients with severe mental illnesses have significant medical illnesses, with up to 53 percent of these illnesses being undiagnosed (
7). Both the number of medical illnesses (
8) and the mortality rates due to medical illness are substantially higher for patients with severe mental illnesses than for the general population (
8,
9,
10). The incidences of diabetes mellitus (
2,
3,
9,
10) and hypertension (
2,
3,
10) are particularly high in this population, and the incidence of chronic obstructive pulmonary disease is somewhat high (
7). Interventions are needed to broadly improve medical services for people with any mental illness, but especially those with severe mental illnesses. The design of these interventions would benefit from a better understanding of the characteristics of the populations that are underusing medical care.
One solution that has been suggested involves psychiatrists and primary care physicians providing some treatment typically given by the other specialty—for example, psychiatrists giving flu shots—which would increase opportunities for the delivery of needed services. However, many psychiatrists are unwilling to give physical examinations (
4), and many are not up-to-date on the management of even common medical disorders. Similarly, primary care providers may misperceive the medical complaints of psychiatric patients as psychosomatic (
5), be uncomfortable treating them (
11), or be unskilled in treating this population. The problem is exacerbated by inadequate information in research studies, such as when studies investigating medical illness exclude subjects with severe mental illnesses and when studies of severe mental illnesses exclude patients with a serious medical illness (
5).
Improving access to care and better integrating medical and psychiatric services for patients with severe mental illnesses (
12,
13) is needed, but relatively little information is available to inform these efforts. Most research on integrating care is conducted in mental health systems that have minimal or no linkages with medical care organizations, so the relationship between the two has been difficult to evaluate. Eligible veterans, however, have access to both medical and mental health services within one health care organization through the Department of Veterans Affairs (VA). Investigating use of medical care in a comprehensive system may provide important information about patients who do and do not use services. This data will inform the design of interventions to improve medical care for all people with mental illness.
In this study we investigated use of medical services among people using VA health care in Southern California and Nevada. We examined receipt of medical care and the intensity of medical care among several subgroups. We evaluated the impact of demographic characteristics, psychiatric diagnoses, and comorbid medical conditions on the use of medical services.
Methods
Sample
This study was a secondary analysis of centralized VA utilization data, requiring no informed consent. Institutional review board approval was obtained for the study. The sample included all patients who received treatment during fiscal year 2000 at any one of seven medical centers or 18 outpatient clinics throughout Veterans Integrated Service Network 22 (VISN 22), which comprises facilities in Southern California and Nevada. The total number of patients was 175,653. Within this group, a primary psychiatric diagnosis was assigned to 47,516 patients on the basis of the ICD-9 diagnoses recorded in the outpatient data file. Patients with multiple psychiatric diagnoses were categorized in the group with the more severe illness. The sample included patients with schizophrenia (N=6,581), bipolar disorder (N=3,694), anxiety disorders (N=14,930), depressive disorders (N=6,295), posttraumatic stress disorder (PTSD) (N=2,588), substance use disorders (N=13,428), and those with no psychiatric diagnosis (N=128,137).
Data sources
The sample was identified in the Outpatient Clinic files at the VA Austin Automation Center. Patients who had used any type of service—for example, medical, psychiatric, occupational therapy, or telephone triage—during fiscal year 2000 were included. We defined "medical visits" as visits to primary care or specialty care clinics only. We extracted demographic information and patient factors that could be predictive of greater service utilization. General medical diagnoses were determined by ICD-9 codes in the data files. Since the database contained multiple entries of the same or similar diagnoses, only the first three digits of the ICD-9 numbers were considered. The number of medical diagnoses was determined by summing the number of different ICD-9 three-digit numbers.
Analysis
SAS was used for all analyses (
14). We constructed four models. The first model evaluated the intensity of medical care—that is, the total number of primary care and specialty care visits—for veterans who had at least one medical visit during fiscal year 2000. Independent variables included sex, marital status, race, income, age, score on the Global Assessment of Functioning (GAF) (
15), number of medical diagnoses, and diagnoses of diabetes, hypertension, and chronic obstructive pulmonary disease. Also included was each veteran's level of service-connected disability, which is based on having an illness or injury incurred or aggravated during active military service. We used Poisson regression to model the dependent variable.
The sample for the second model was restricted to patients with diabetes who had at least one medical visit in fiscal year 2000. The independent variables included sex, marital status, race, income, age, service-connected disability, GAF score, and number of medical diagnoses. The dependent variable was the total number of medical visits during that year. Using Poisson regression, we examined factors that affected the likelihood that veterans with a severe mental illness and diabetes received medical treatment. The design for the hypertension model was similar to that of the diabetes model, except that the sample was restricted to all patients with hypertension who had at least one medical visit during the study period.
The fourth model examined whether patients 50 years of age and over had at least one medical visit during the one-year study period. The independent variables for this model included sex, marital status, race, age, income, GAF score, and service-connected disability. Through logistic regression, the model evaluated the probability that older veterans with severe mental illness had a yearly medical visit as a function of a number of predictors.
Results
Descriptive statistics
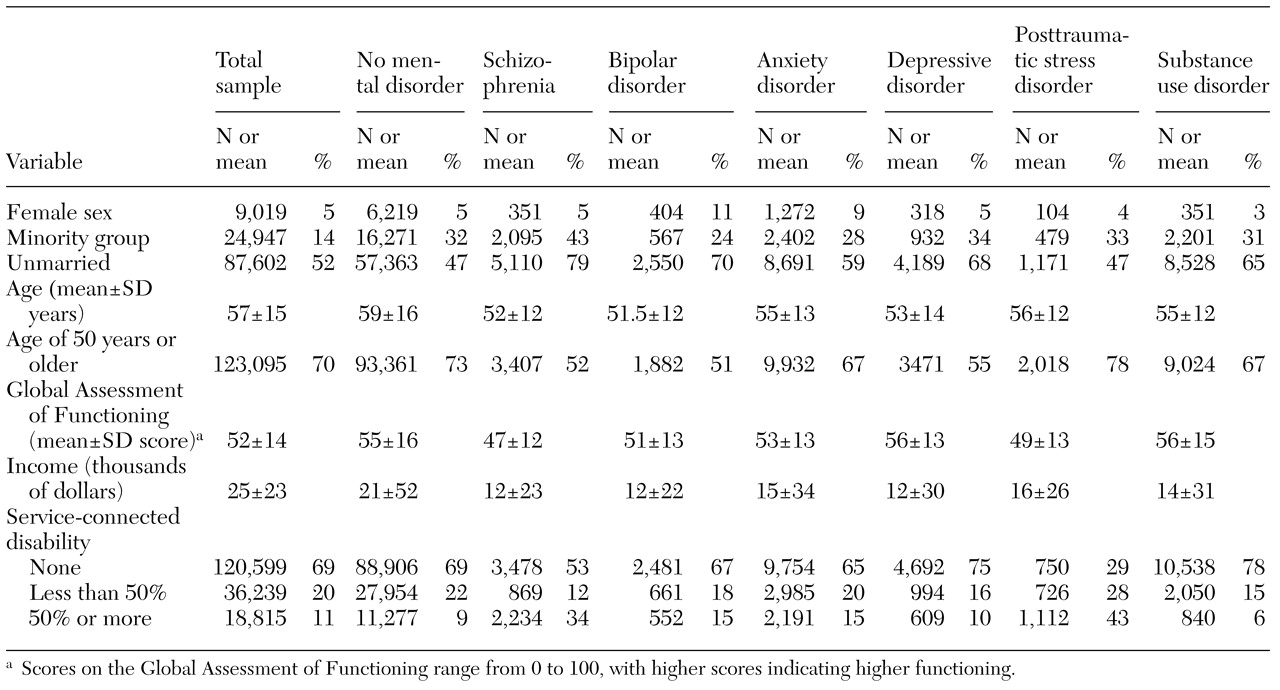
The sample's demographic characteristics are listed in
Table 1. Rates of comorbid medical diagnoses were examined for all veterans in VISN 22 who received some service in fiscal year 2000. Among veterans with no psychiatric diagnosis, 16,160 (13 percent) had a diagnosis of diabetes, 4,608 (4 percent) a diagnosis of chronic obstructive pulmonary disease, and 46,518 (36 percent) a diagnosis of hypertension. Rates for these diagnoses among patients with severe mental illnesses were far lower: 982 (10 percent) had diabetes, 395 (4 percent) had chronic obstructive pulmonary disease, and 2,750 (27 percent) had hypertension. In fact, the groups with severe mental illnesses had the highest proportions of patients who did not have a diagnosis of any of the medical illnesses targeted in this study. Sixty-six percent of the patients who had schizophrenia (N= 4,315) and 65 percent of those with bipolar disorder (N=2,396) had no diagnosis of chronic obstructive pulmonary disease, hypertension, or diabetes. Patients with a diagnosis of an anxiety or substance use disorder, on the other hand, were more likely to have a diagnosis of chronic obstructive pulmonary disease (5 to 10 percent) or hypertension (39 to 41 percent) than any other group.
Regression models
Receipt of any medical care was examined for each psychiatric diagnosis. A total of 11,518 patients with a substance use disorder (86 percent) had at least one medical visit, 12,724 (85 percent) of those with anxiety disorders, 2,830 (77 percent) of those with bipolar disorder, 98,010 (76 percent) of those with no psychiatric diagnosis, 4,566 (69 percent) of those with schizophrenia, and 4,100 (65 percent) of those with a depressive disorder. There was no significant difference between use of primary care and specialty care visits, so the categories were lumped together as "medical visits" for the purposes of the analysis.
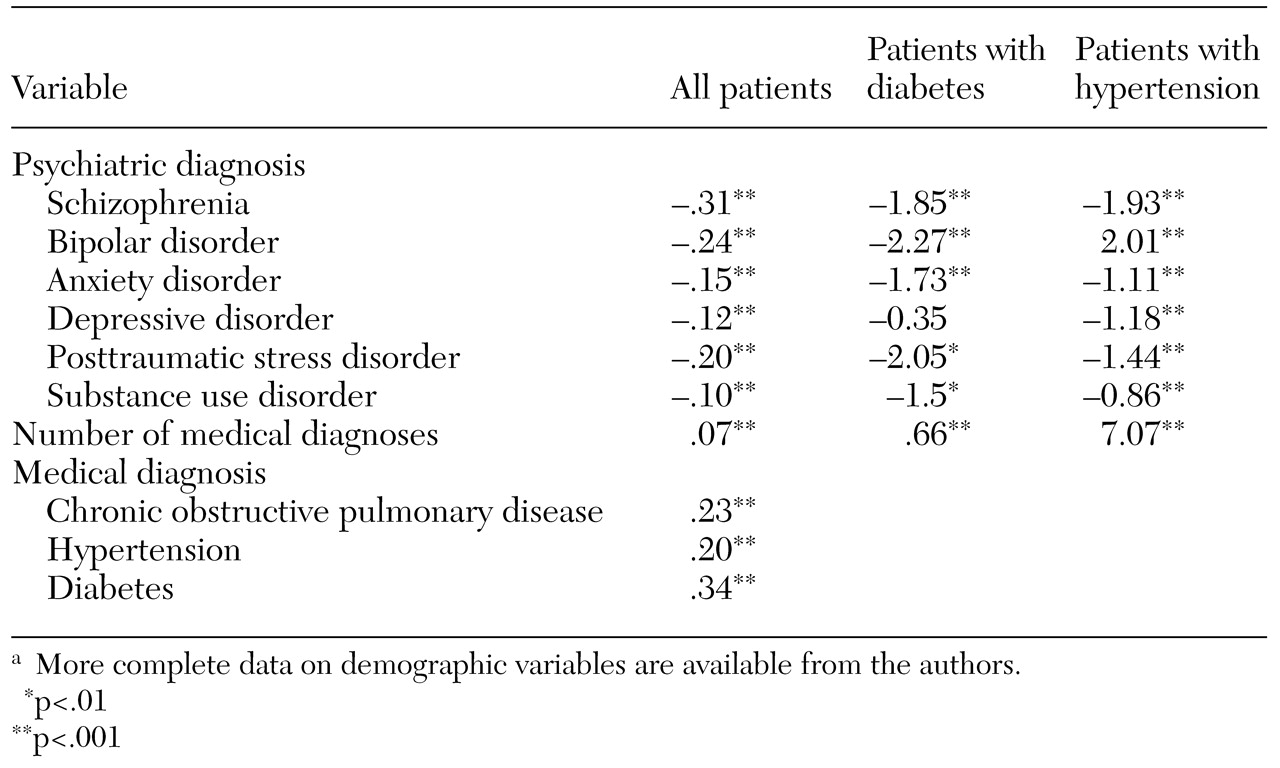
As
Table 2 shows, the intensity model indicated that patients with any psychiatric diagnosis had fewer medical visits than patients with no psychiatric diagnosis. Patients with schizophrenia and bipolar disorder had particularly few medical visits. Veterans who were older or female had more medical visits. Patients with comorbid diagnoses of chronic obstructive pulmonary disease, hypertension, or diabetes had more medical visits.
Poisson regression showed that patients with diabetes were less likely to have more than one medical visit if they also had a diagnosis of an anxiety disorder, schizophrenia, bipolar disorder, PTSD, or a substance use disorder. Patients were more likely to have multiple medical visits if they were in ethnic minority groups, were older, or had additional medical diagnoses. Among patients with hypertension, those who had any psychiatric diagnosis were less likely to have more than one medical visit. Patients who were female, in an ethnic minority group, or older were more likely to have had medical visits.
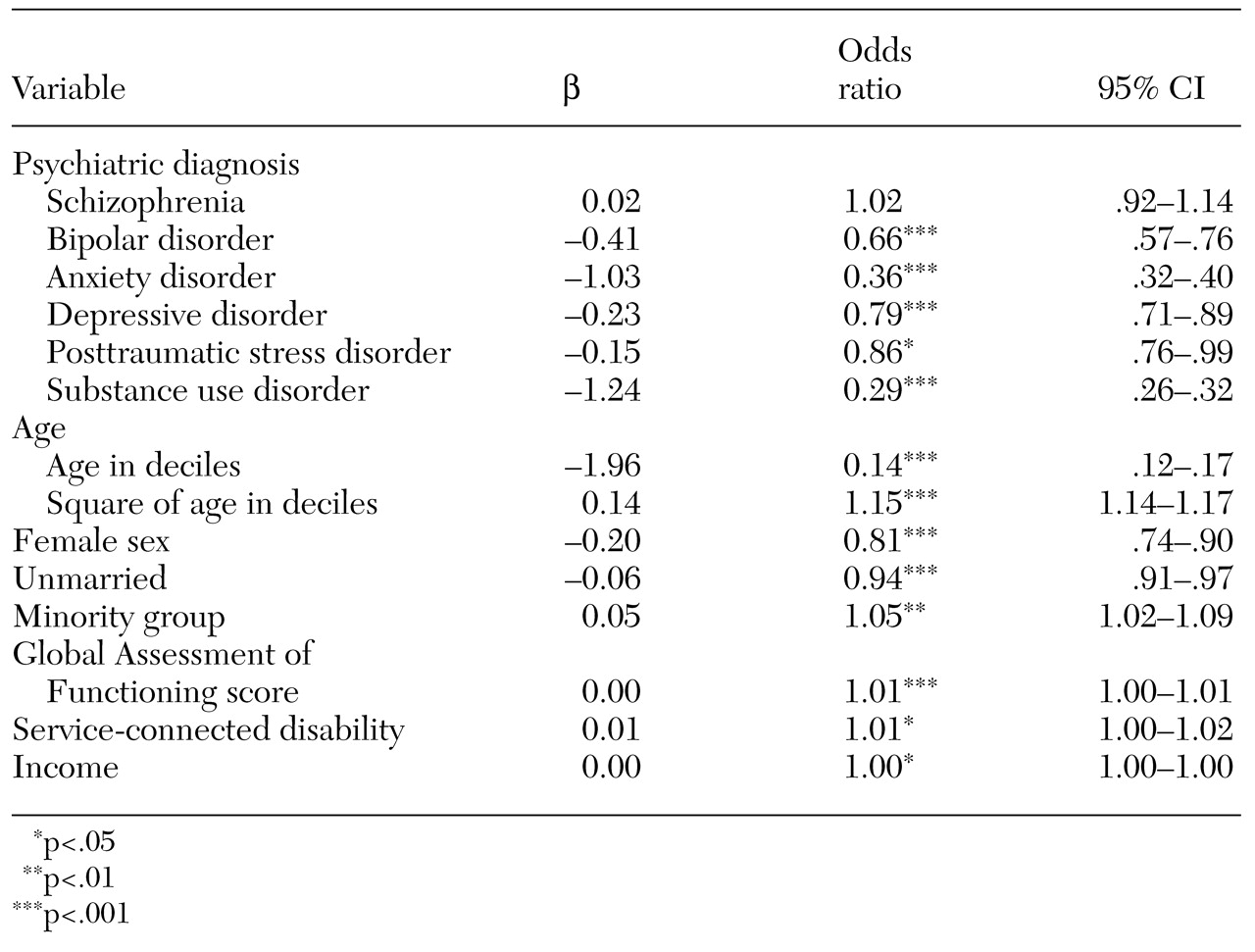
Table 3 presents the results of logistic regression analyses predicting one or more medical visits during the year for veterans 50 years of age and over. Patients in this group were less likely to have a medical visit if they had a diagnosis of a substance use disorder (odds ratio [OR]= .29), a depressive disorder (OR=.79), an anxiety disorder (OR=.36), a bipolar disorder (OR=.66), or PTSD (OR=.86). There was no significant difference for patients with a diagnosis of schizophrenia. Patients who were older were more likely to have had a medical visit (OR=1.15).
Discussion
Patients with psychiatric diagnoses were less likely than other veterans in VISN 22 to use medical services during fiscal year 2000. This problem was particularly severe for young adults who had schizophrenia or posttraumatic stress disorder and for adults of all ages who had bipolar disorder. Patients with other psychiatric conditions, such as substance abuse and anxiety, were more likely than patients without psychiatric conditions to have at least one medical visit. The nature of these disorders may prompt patients to seek help, either to relieve additional anxiety about physical symptoms or to treat conditions secondary to substance misuse. Our finding that patients with depressive disorders had less service use is different from previous studies that have found more use (
16,
17). Depressive disorders often are not diagnosed (
18), and we had no way to detect undiagnosed depression. It is quite possible that veterans with undiagnosed depression had higher use of medical services. Finally, patients with chronic obstructive pulmonary disease, hypertension, and diabetes had more visits.
With the exception of patients with schizophrenia, patients over the age of 50 were less likely to have any medical visit if they also had a psychiatric diagnosis. This trend is of concern, as annual visits are opportunities for providing preventive care and for detecting medical illnesses before they become severe. Patients with schizophrenia received more medical care after age 50, which may reflect the fact that patients with severe mental illnesses are more likely to be institutionalized and thus to be in direct contact with medical providers.
Clearly, patients with severe mental illnesses would benefit from improved access to medical care. A recent study evaluating an integrated medical clinic for patients with severe mental illnesses found that patients in an integrated care setting had more medical visits than those in other care settings (
19), confirming the usefulness of integrated models found in previous studies (
12,
13). However, implementing integrated care programs can be costly and time-consuming, which limits their feasibility. Such programs also may be insufficient to ensure that patients with the most severe mental illnesses use services.
Other types of interventions may be useful, such as improving provider competencies through education and profiling. For example, psychiatrists might benefit from education in basic medical evaluation, and primary care physicians may need training on symptoms of serious mental illnesses and effective ways to interact and communicate with these patients. Organizational interventions, such as computerized reminders to prompt mental health providers to send their patients for needed primary care, also may increase use of medical services.
Unlike most private health care insurance, VA coverage provides a full range of services to people with severe mental illnesses. However, even when medical and psychiatric services are provided within the same organization, challenges remain. Interventions are needed to ensure that these patients receive basic medical care, and such interventions may need to be adjusted to a patient's psychiatric diagnosis.
Given the nature of secondary data analysis, our study has some limitations. First, we were unable to capture utilization data for patients who did not meet the sample criteria. These patients may have received care outside of the VA system, may have received additional services at a visit that was not primary or specialty care, or may have received no care at all. Second, diagnostic information in large administrative data sets is not as accurate as that obtained in structured research assessments, and severity of illness cannot be fully modeled. Since diagnoses are typically made during medical visits and many patients did not have such visits, our data may underestimate the presence of medical disorders. Finally, while our findings for this sample of veterans may or may not be generalizable to a larger population, it is likely that patients outside of the VA system receive even less care, since their treatment is not delivered in one comprehensive health care system and their mental health benefits are more limited.
Conclusions
Examining the use of medical services through analyses of large databases is useful for evaluating quality of care. Patients who do not use services or who use them infrequently are not receiving good care. This method, combined with additional analyses of organizational or provider variables, can also be used to evaluate changes in utilization patterns over time and to enhance our understanding of gaps in care that need to be remedied.
Acknowledgments
This project was supported by the Department of Veterans Affairs (VA) Health Service Research and Development Service, the VA Desert Pacific Mental Illness Research, Education, and Clinical Center (MIRECC), the VA Center of Excellence for the Study of Healthcare Provider Behavior, and by grant P50-MH-54623 from the National Institute of Mental Health to the University of California, Los Angeles-Rand Research Center on Managed Care for Psychiatric Disorders.