Although antipsychotic pharmacotherapy is an important component of treatment for most people with schizophrenia, most antipsychotics are associated with some weight gain. The atypical agents, with the exception of ziprasidone, are especially problematic (
1). This observation is troubling given the association of obesity with a variety of adverse health outcomes and elevated mortality rates as well as data showing that persons with schizophrenia have a greater risk of obesity even in the absence of antipsychotics (
2).
The psychological distress and quality-of-life impairment caused by weight gain (
3) may also interfere with medication compliance (
4). According to a recent review by Perkins, "Among patients treated with conventional neuroleptics, approximately 40 percent stop taking their antipsychotic medication within one year, and about 75 percent stop taking the medication within two years" (
5). One of the most frequent reasons patients offered for this nonadherence was weight gain. Naber and colleagues (
6) conducted a chart review of 480 people with schizophrenia who had taken clozapine and found that 13 percent experienced clinically significant weight gain. Of these, 14 percent discontinued their treatment. In addition, Fakhouri (
7) presented data indicating that among patients who reported weight gain as a side effect of antipsychotic medications, more than 70 percent described the weight gain as "extremely distressing." This percentage was higher than that for any other side effect.
Given these data and the obvious importance of this problem, we sought to assess the association between weight gain and quality of life among persons with schizophrenia.
Methods
An eight-page, self-administered questionnaire designed to explain and predict health care attitudes and behaviors among persons with schizophrenia was distributed in September 1999. For confidentiality purposes, respondents were contacted indirectly through chapters of the National Alliance for the Mentally Ill (NAMI) and the National Mental Health Association (NMHA), which distributed questionnaires to their members who had schizophrenia. A cover letter explained the project and informed respondents of their rights. The project methods and questionnaire received institutional review board approval.
Consumer Health Sciences, an independent market research company located in Princeton, New Jersey, designed the survey in consultation with medical professionals working and conducting research in schizophrenia. A total of 1,527 questionnaires were mailed to 203 NAMI and NMHA chapters across the United States; 304 surveys were returned. Because the surveys were distributed indirectly, precise response rates could not be calculated.
The survey respondents were asked how many pounds they gained in the previous six months and were categorized into four groups: those who gained no weight, those who gained one to ten pounds (.5 to 4.5 kg), those who gained 11 to 20 pounds (5 to 9.1 kg), and those who gained more than 20 pounds.
The respondents were asked to rate their quality of life on a scale from 1 to 10, with higher scores indicating a better quality of life. A 16-item scale was also used to evaluate specific domains. Respondents reported how satisfied they were with each domain on a scale from 1, not at all satisfied, to 5, extremely satisfied. The 16 items had high internal consistency (Cronbach's alpha=.91). An overall score was calculated on the basis of the mean across all domains.
Psychological well-being was measured with the Psychological General Well-Being Index (PGWB) (
8). This 22-item scale measures intrapersonal affective or emotional states, reflecting subjective well-being. Participants rated the frequency of each state during the previous month, from 0, none of the time, to 5, all the time. Responses were summed so that possible scores ranged from 0 to 110, with higher scores indicating greater well-being. The PGWB also has six subscales: anxiety, depressed mood, general health, positive well-being, self-control, and vitality.
Other factors that could explain the relationship between weight gain and quality of life were evaluated as control variables. One such factor was gender, because there are known differences between men and women in concerns about weight gain. We also hypothesized that there would be differences in side effects and attitudes toward medications between people who were taking atypical antipsychotics and those who were taking conventional agents. The Physicians' Desk Reference was used to classify medications.
Age and current relative weight were also included as covariates. Relative weight was based on body mass index (in kg/m
2), calculated from respondents' self-reported height and weight. These types of self-reports have been highly correlated (r>>.90) with measured height and weight and with direct measures of body fat (
9).
The bivariate relationship between weight gain and quality of life was evaluated for all study participants by using analysis of variance (ANOVA). Linear regression analyses were then used to test the independent effect of weight gain on quality of life, with potential confounders controlled for. The number of pounds gained was the independent variable in separate models in which the two quality-of-life measures and seven PGWB scales were dependent variables. All statistical tests were two-tailed at an alpha level of .05 and were conducted with SPSS.
Results
Of 304 respondents, 286 (94 percent) provided weight gain information and were therefore included in the analyses. A total of 156 study participants (55 percent) were men, and the participants' mean±SD age was 42±10 years. About three-quarters of the sample (226 participants, or 79 percent) were white. Most (201 participants, or 70 percent) used atypical antipsychotics (mean duration, 33.9±28.6 months); about a quarter (78 participants, or 27 percent) used conventional antipsychotics (mean duration, 123.2±91 months). The participants' mean body mass index was 30±7 kg/m2. About half the sample (126 participants, or 44 percent) reported gaining weight in the previous six months: 42 percent gained less than ten pounds, 27 percent gained 11 to 20 pounds, and 31 percent gained more than 20 pounds.
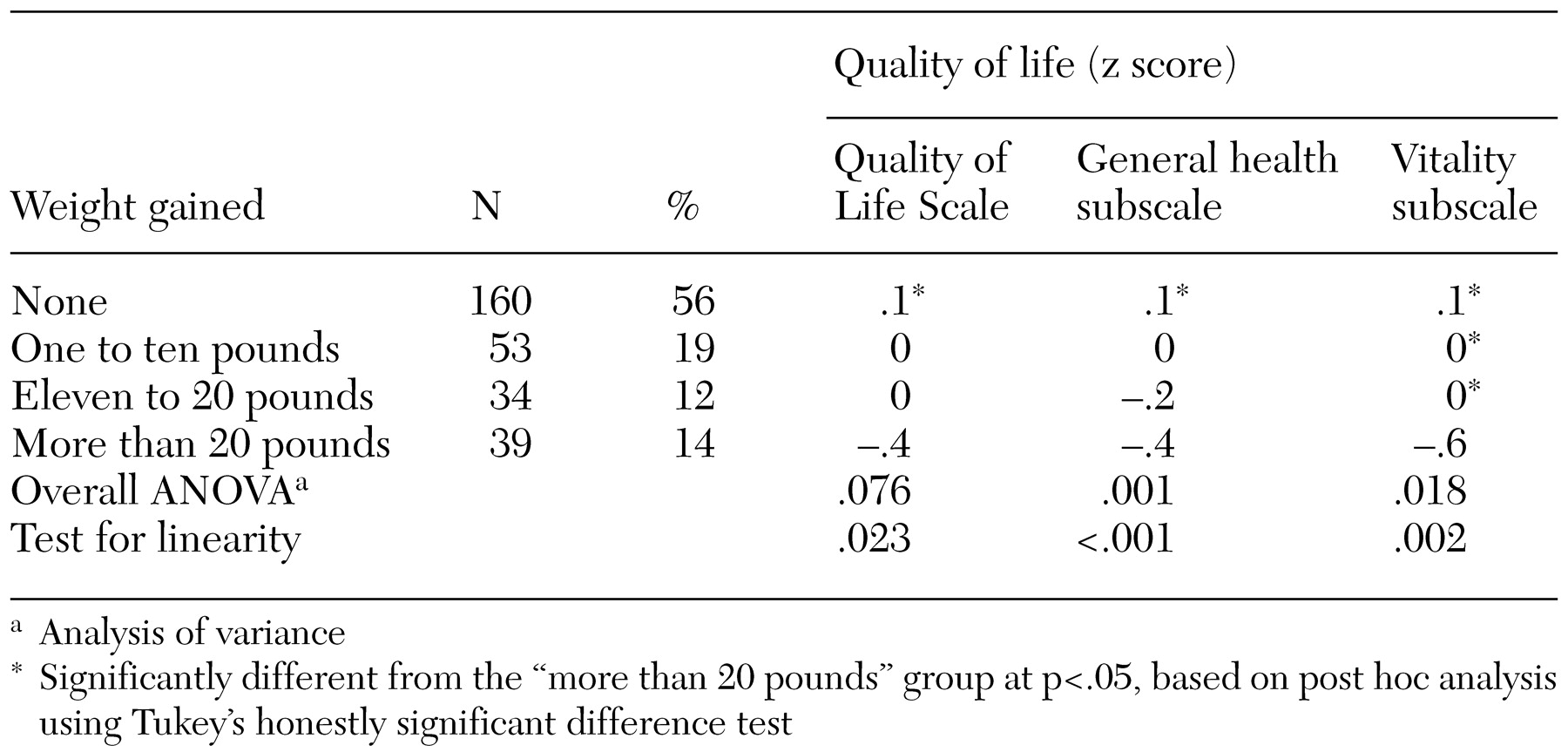
ANOVA results showed that respondents who gained more weight had a poorer quality of life, although the difference was not statistically significant. Those who gained more weight also had significantly lower general health (F=3.43, df=3, 276, p=.02) and vitality (F=5.97, df=3, 276, p<.001), as measured by subscales of the PGWB (
Table 1).
Linear regression analyses were then conducted to evaluate the independent relationship between weight gain and quality of life, controlling for potential confounders—gender, type of antipsychotic medication, age, and body mass index. Weight gain was significantly associated with poorer quality of life on the basis of the 16-item scale (regression coefficient, -.01; p=.011). Respondents who gained weight also had poorer general psychological well-being (not statistically significant), self-reported general health (regression coefficient, -.03; p=.033), and vitality (regression coefficient, -.05; p=.007).
Discussion and conclusions
We found that weight gain was associated with lower quality of life, even after gender and body mass index were controlled for. For men and women, and at any body mass index, gaining weight was associated with reduced quality of life.
Specifically, weight gain was associated with perceptions of poorer quality of life, general health, and vitality. These associations were of a fairly large magnitude: study participants who gained more than 20 pounds had quality-of-life scores that were 12 percent lower, general health scores that were 19 percent lower, and vitality scores that were 32 percent lower than those of participants who did not gain weight. At least one empirical study (
4) and substantial anecdotal evidence suggest that weight gain is distressing to persons with schizophrenia. However, to our knowledge, this is the first large survey offering evidence that weight gain is directly associated with reduced quality of life.
This study had several limitations. Because the study was cross-sectional and nonrandomized, we cannot infer causality. Although it is a reasonable supposition that weight gain was responsible for the participants' poorer quality of life, we cannot rule out the possibility that individuals who experience a decline in quality of life tend to gain weight or the possibility that a confounding factor predisposed people to both weight gain and poorer quality of life. Further research—longitudinal and experimental—will be necessary to definitively disentangle these hypotheses.
The fact that the data were self-reported is an additional potential limitation. People who experience a decline in quality of life could be more likely to recall weight gain. Moreover, self-reported height and weight are prone to small but statistically significant biases (
9). Although these limitations must be acknowledged, it is not obvious how they might have influenced the current results.
In addition, the recruitment through NAMI and NMHA raises the possibility of selection bias and limited generalizability. The fact that the sample was predominantly white (70 percent) and middle-aged (average age of 42 years) suggests that there may have been some bias. However, the poorer quality of life we observed among respondents who gained weight may be more exaggerated among patients who do not participate in structured support groups such as those offered by NAMI and NMHA.
Despite these limitations, this research has important implications. First, the results should alert health care providers to attend to weight gain and consider the weight-gain effects of various drugs. Second, the results underscore the deleterious effects of weight gain among persons with schizophrenia, even among those who do not become obese. Such effects suggest the need for research evaluating methods for preventing and treating weight gain in this population. Given that weight gain and obesity increase the risk of many physical ailments, it may be that impaired physical health leads to the decrements in subjective well-being we observed in this study.
Finally, although this analysis did not include information about compliance, a reasonable conjecture is that people who gain weight and experience a decline in quality of life will be less compliant with their medication regimens. Further research is clearly necessary to test this hypothesis. Recent research using the same data showed that people with a higher body mass index are more likely to be nonadherent to medication regimens (
10). Thus the association between weight gain and adherence deserves further exploration. If the hypothesis is supported, research that aims to reduce the impact of weight gain on quality of life or compliance—or, more important, to reduce weight gain itself—is warranted.
Acknowledgment
Funding for this study was provided by Pfizer, Inc.