Medication errors—prescribing, transcribing, dispensing, and administration errors—are associated with considerable patient morbidity and mortality. An estimated 1 to 2 percent of inpatients in the United States are harmed as a result of such errors (
1). Administration errors are one of the most common types of medication errors. On the basis of the findings of a number of U.K. observational studies in general hospitals, administration errors affect approximately 5 percent of all administered doses (
2). However, in a U.S. study of 36 health care facilities, the reported frequency was 19 percent (
3).
Much of the research on administration errors has focused on general hospitals and on errors involving intravenous drugs and infusions. Few studies of medication errors have been conducted in psychiatric settings, and even fewer have concentrated on administration errors (
4). A U.S. study of medication errors, based on a retrospective review of records in a state psychiatric hospital, showed that administration errors were more frequent than prescribing, transcribing, and dispensing errors combined (
5).
The aim of the study reported here was to conduct a retrospective survey of the nature, frequency, and potential severity of and contributing factors to medication administration errors reported by nurses in a large psychiatric hospital in the United Kingdom. We aimed, on the basis of these findings, to make recommendations to improve medication administration practice and systems.
Methods
The survey was approved by the hospital's clinical audit and research committees. St. Andrew's Hospital in Northampton, United Kingdom, is a 450-bed charitable psychiatric hospital that provides inpatient treatment under mainly secure conditions for patients who have diverse mental health problems. The hospital consists of five subunits (divisions), which provide services for various patient groups: general and forensic adolescent services, adult forensic and rehabilitation services, brain injury rehabilitation services, services for elderly patients, and services for persons with learning disabilities. Approximately 80 percent of patients are given prescriptions for regularly administered antipsychotics; 40 percent for lithium or antiepileptics, or both; 35 percent for antidepressants; and 20 percent for benzodiazepines. No data are available for as-needed medications.
Prescription orders are written on a paper prescription chart. Each time a medication is administered to a patient, the administering nurse is required to sign the chart. The hospital has a policy that all medications are to be administered by a registered nurse. Medications are generally administered by one designated nurse.
All administration errors are reported on a standard (paper) form. On this form, the reporting nurse describes the error, the drug or drugs involved, and any contributing factors. Reports are forwarded to a senior nurse manager, who takes appropriate action—for example, requiring the nurse who made the error to undertake additional training or correcting faults inherent in the environment.
We undertook a retrospective review of medication administration error reports made between October 1, 2000, and March 31, 2004. We defined a medication administration error as a deviation from a prescriber's valid prescription or the hospital's policy in relation to drug administration, including failure to correctly record the administration of a medication. We used standardized taxonomy to classify errors (
6). Incidents that met the study's definition but had been detected before administration ("near misses") were classified as errors. Administration errors were graded as 1, of doubtful or negligible importance; 2, having the potential to cause minor adverse effects or worsening of the condition; 3, having the potential to cause moderate adverse effects or worsening of the condition; 4, having the potential to cause serious adverse effects or relapse; or 5, potentially fatal. Each incident report was rated independently by the three investigators (a consultant psychiatrist, the head pharmacist, and a senior nurse), who then met and reached a consensus on whether the incident met the study's definition of an administration error, its type, and its severity.
Narrative information about factors reported as contributing to administration errors was extracted from reporting forms and was subjected to content analysis. Contributing factors were categorized into broadly defined themes.
Data on the nature and number of medication doses administered during the study period were not available, because they are not routinely collected. Thus, to estimate the frequency of administration error reports relative to the number of doses administered, we examined 50 random prescription charts (ten per division) and counted the number of doses administered in a one-week period as follows: number of doses of psychotropic as opposed to nonpsychotropic medications, number of doses administered by the intramuscular route as opposed to doses administered by all other routes, number of doses of long-acting intramuscular antipsychotics administered as opposed to doses administered by all other routes, number of doses administered at each of the four routine daily drug rounds as opposed to the number of as-needed doses, and number of doses administered by day nursing staff as opposed to the number administered by night staff.
Chi square tests with Yates' correction and Fisher's exact tests were used to compare the frequency of various types of administration errors with the relative frequency of administration.
Results
During the study period, 123 administration error reports were received. Of these, 108 (88 percent) met the study's definition of an administration error, and a further four (3 percent) were categorized as near misses, for a total of 112 errors (11 reports were not considered to describe administration errors). Reporting frequency remained fairly constant, at an average of four error reports per three-month period between October 2000 and March 2003. After that there was an increase in reporting frequency to nearly 18 reports per three-month period for the remaining 12 months studied.
Large differences were noted in the numbers of errors reported by the hospital's divisions. More than half the errors (59 of 112, or 53 percent) originated from the adolescent division, and very few errors were reported among elderly patients (three of 112, or 3 percent) or in the brain injury rehabilitation division (five of 112, or 4 percent). Errors were not concentrated on any particular ward.
Psychotropic medications were involved in 85 percent of errors and nonpsychotropics in 15 percent. By comparison, data from examination of the 50 prescription charts showed that 50 percent of the doses administered during a one-week period were of psychotropic medications. Psychotropic medications were significantly more likely than expected to be involved in administration errors (85 percent compared with 50 percent; χ2=50.1, df=1, p<.001). Short- and long-acting intramuscularly administered medications were significantly more likely than medications administered by all other routes to be involved in administration errors (12 percent compared with 3 percent; Fisher's exact test, two-tailed p<.001, df=1). Long-acting intramuscular antipsychotics were significantly more likely than other medications to be involved in administration errors (7 percent compared with .1 percent; Fisher's exact test, two-tailed p<.001, df=1). Most errors (87 percent) involved regularly administered medications administered at one of the four daily drug rounds. However, significantly more errors than expected involved as-needed medication (13 percent compared with 4 percent; Fisher's exact two-tailed p<.001, df=1). Errors were no more likely than expected to be administered by day nursing staff than by night nursing staff.
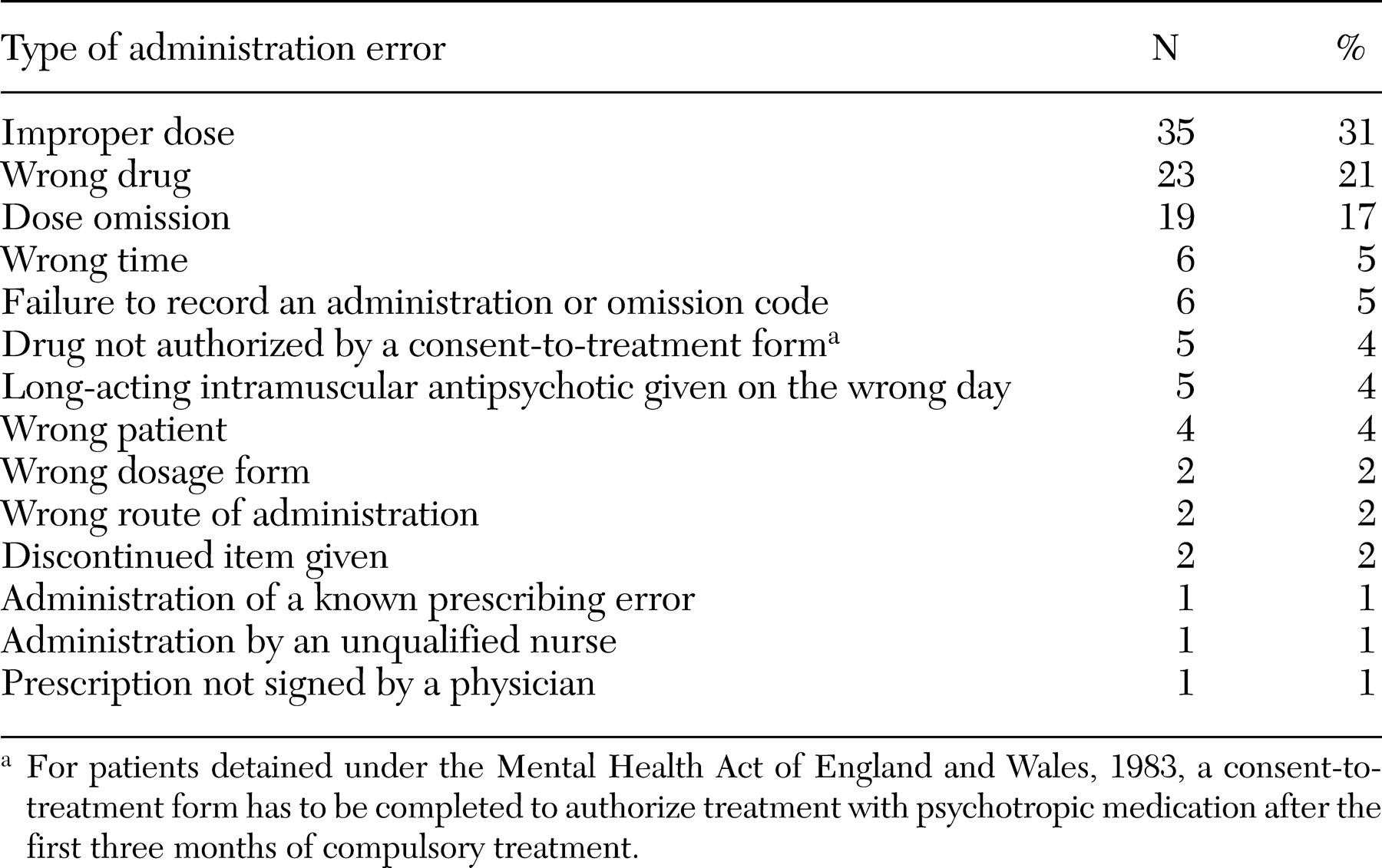
The most frequent types of errors were administration of an improper dose, wrong drug, and dose omission (
Table 1).
For 103 of 112 errors (92 percent), sufficient information was available to rate error severity. Although 86 errors (77 percent) were rated as grade 1 or 2 (of doubtful importance or having the potential to cause minor adverse effects), 16 (14 percent) were rated as grade 3 (having the potential to cause moderate adverse effects), and one (1 percent) was rated as grade 4 (having the potential to cause serious adverse effects). Of the 17 grade 3 and grade 4 errors, 13 (76 percent) involved antipsychotic drugs (clozapine [four patients], other oral antipsychotics [four patients], and long-acting intramuscular antipsychotics [five patients]). A somewhat greater proportion of minor errors (grade 1 or 2) were reported by the adolescent service than were reported in the rest of the hospital (91 percent compared with 76 percent), but the difference was not statistically significant (p=.06).
On 70 forms (63 percent) the nurse had recorded information about factors believed to have contributed to the error (some gave multiple reasons). Busy, noisy ward environments or being short of staff were cited on 19 occasions, and difficulty reading or understanding physicians' instructions were reported on ten occasions. Nurses cited physician-related factors as contributing to 11 errors. Other themes were failure in communication (nine instances), confusion over similar-sounding drug names or patient names (eight instances), and problems with the physical layout of the drug administration area or storage of medications (six instances). Nurses described personal factors as contributing to errors in 19 instances, including tiredness, poor concentration, inadequate supervision, and lack of support.
Discussion and conclusions
Given that very little has been reported in the literature about medication administration errors in psychiatry, this small study of error reports has provided some descriptive information about such errors. We found that the most frequent types of administration error reported were administration of a wrong drug, improper dose, and dose omission. Psychotropic, intramuscular, and, in particular, long-acting intramuscular antipsychotics and as-needed drugs were all overrepresented. Fifteen percent of errors were rated as having the potential to cause moderate or severe harm to patients. A greater proportion of errors were reported by the adolescent service, but we suspect that this finding is an artifact of differential reporting of errors rather than a true difference in the number of errors occurring. Clinicians and managers in the adolescent service have deliberately fostered a "no blame" culture surrounding medication errors to encourage reporting of errors. The increased frequency of reporting after April 2003 coincided with changes in the hospital's senior nursing staff, an increase in patient numbers, and a trend to report less serious errors.
The study had limitations. It was a retrospective review of incident reports completed by nursing staff. However, it is well known that incident reports detect only a very small number of errors compared with chart review and observational studies (
7). Reasons for this gross underreporting include lack of awareness that an error has occurred, belief that the patient has not been harmed, and reluctance to report because of fear of disciplinary action (
8). The number of error reports completed was also relatively small. The study hospital is a tertiary referral center that has many long-stay patients with specialist needs. These patients frequently have complex medication regimens. Thus the study center cannot be regarded as typical of U.K. psychiatric units. However, despite these limitations, the study has provided a description of commonly reported administration error types and some insights into nurses' perceptions of the causes of these errors.
Prospective observational studies of medication administration are needed to more accurately determine the frequency of administration errors in psychiatry. Studies involving structured interviews with nurses shortly after errors have occurred could systematically examine factors that have been implicated in error causation. To conduct such research, it is necessary for staff to feel supported by an open, "no blame" culture surrounding errors.
Nurses cited a variety of factors as contributing to errors, but the two most common factors related to the fact that drugs were administered in a busy, noisy environment to difficult, disturbed patients, sometimes with less than optimal staffing levels, as well as personal factors, such as feeling tired, upset, or unsupported. These factors have been identified as relevant to error causation in general hospital settings (
9). In our study a number of nurses implicated physicians in errors, mainly citing unclear or ambiguous medication orders, particularly when a new order had been written. This finding suggests that physicians can reduce the risk of administration errors by writing clear and unambiguous prescriptions and by informing the in-charge nurse of major changes in patients' drug therapy. One surprising finding was that nursing staff did not report a lack of training as contributing to errors, although some spoke of inexperience and inadequate supervision. In general hospital settings, lack of knowledge has been found to underlie a substantial proportion of errors (
9,
10).
Following this study and another study of prescribing errors, our hospital is introducing a computerized reporting system to facilitate reporting of all types of medication errors. We are aware that many errors go unreported with the current paper reporting system. We are planning an observational study to better assess the nature and frequency of administration errors. Staff are also being encouraged to report all errors and near misses, however trivial. One division of the hospital is piloting a system whereby the nurse who administers the medication is observed by a health care assistant who has been specially trained to detect medication administration errors. In the next few years electronic prescribing connected with a patient administration and computerized pharmacy system are to be introduced. All these actions are aimed at increasing medication safety for patients.