For the past ten years the use and misuse of physical restraint has received tremendous attention within and outside of psychiatry (
1). Regulatory agencies and professional groups agree that restrictive interventions should be used in only the most extreme situations, those in which patients pose a danger to themselves or others (
2,
3). The standards set by regulatory agencies and the growing awareness of the potential dangers of restraint use (
4) place increasing pressure on child and adolescent psychiatric units to reduce the use of locked seclusion and restraint (
5).
It is ironic that for an issue that is discussed with such tremendous urgency, we know very little about the use of restraint during the brief inpatient hospitalization of youths, what type of youth is most likely to be restrained, how often youths are restrained, and why they are restrained.
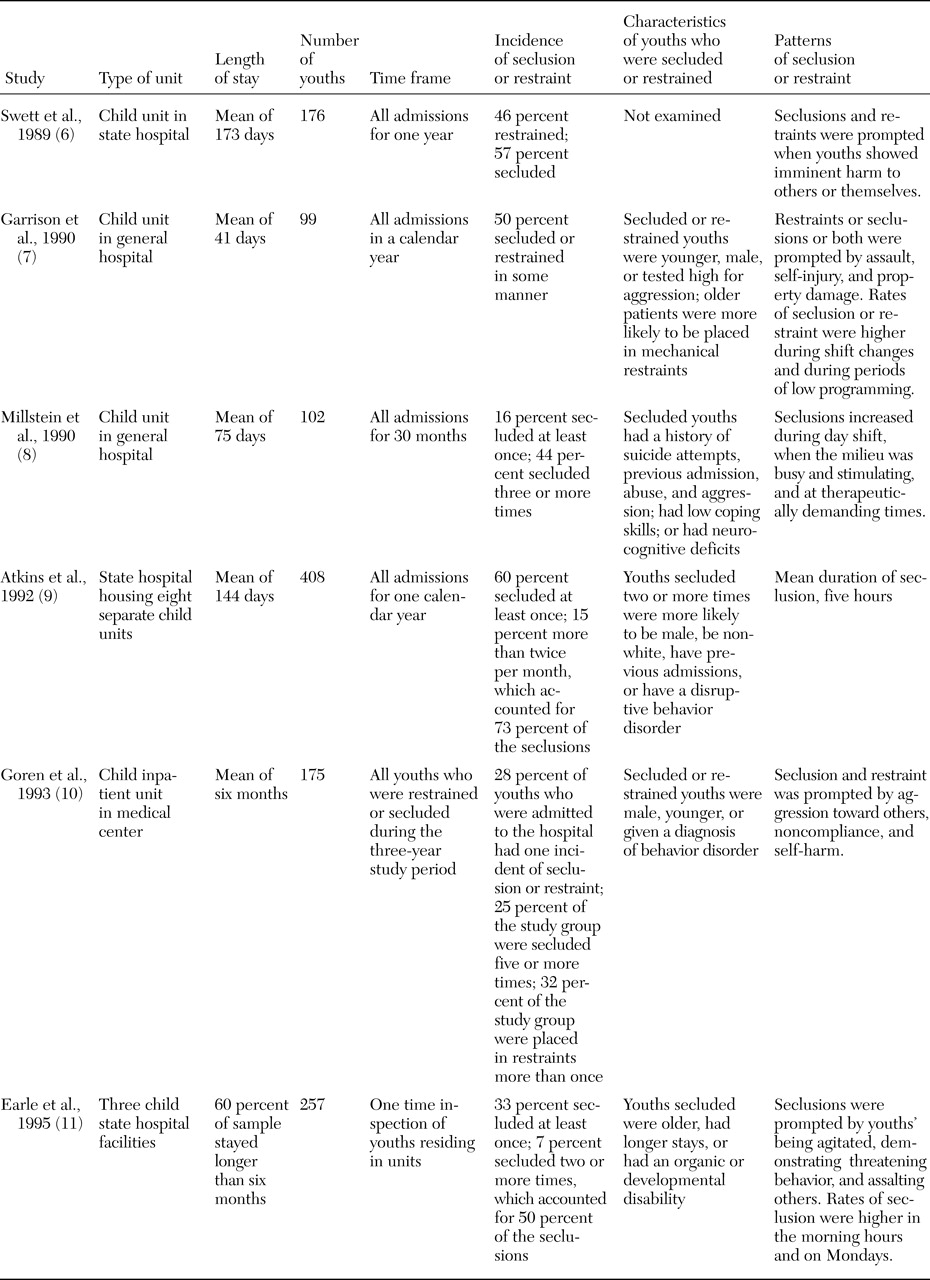
Table 1 lists past studies of seclusion and restraint among youths in brief psychiatric treatment (
6,
7,
8,
9,
10,
11). The rates and patterns of locked seclusion and restraint among these youths have not been examined in U.S. institutions in the past ten years. Yet much has changed in the past decade. Ten years ago the use of seclusion and restraint for behavioral control was a more accepted practice (
12). In 1990 Millstein and Cotton (
8) reported that 60 percent of all children who were admitted to their hospital were placed at least once in locked seclusion. In a subsequent publication Cotton (
13) endorsed the therapeutic benefits of this practice. Today there is almost zero tolerance for the use of restraint and locked seclusion (
14,
15). New guidelines have been developed for handling aggressive youths (
3,
16), all in adherence with federal regulatory restraint policies (
17).
Without recent data it is not possible to determine whether restraints are being used in line with current regulations, that is, to prevent dangerous behavior and serious property damage when other less coercive interventions have failed (
17). In the past studies cited above, length of stay averaged 75 days; now it hovers at about 11 days (
18). With the dramatic shift in length of stay, it is questionable whether the ten-year-old timing and setting patterns apply—for example, that seclusion or restraint occurs more often at the beginning and end of a youth's hospitalization. Finally, it is unclear what kind of situations prompt restraint use in brief psychiatric treatment or whether there is a type of youth at risk of being restrained, either once or multiple times.
The purpose of this retrospective study was to examine the current practice of restraint use among youths in brief psychiatric treatment. To this end, 100 charts of hospitalized youths were reviewed. Demographic and clinical characteristics in three groups of youths were compared: those who were never restrained, those who were restrained one or two times, and those who were restrained three or more times during their hospitalization. Also examined were the setting (time of day, day of week, place, and programming) and incidents related to restraint use.
Methods
Study site
The study was conducted at a free-standing psychiatric hospital that operates four psychiatric units that were designed for the brief hospitalization of children and adolescents. The hospital is located in a large metropolitan area and admits youths from the inner city and surrounding areas. During the year before the study period, the average length of stay on each unit was approximately 12 days, after scattered outliers were corrected for (length of stay longer than 45 days). The units operate with a neurobehavioral view of youths' maladaptive behaviors.
The hospital is located in a state that continues to allow the seclusion and restraint of youths in accordance with federal regulation. At the time of the study, the facility was undertaking a rigorous restraint reduction program that examined the root causes and patterns of restraint use throughout the facility. As part of the program, staff members from each of the four units were trained in deescalation strategies. Finally, all the units operated under the management philosophy of using restraint only in situations that posed a serious danger to the patient or others and when other less restrictive measures had failed.
Procedure
Approval of Rush University Medical Center's institutional review board was obtained before initiating the study. This study examined the charts of youths who were hospitalized at the study site between December 1998 and January 2000, so that select variables—age, race or ethnicity, caretaker history, aggression six months before admission, and psychiatric history—could be compared. First, a list was compiled of every youth who was restrained during this period at the study site. A total of 69 youths had been restrained during this period. Among these 69 youths, 12 had been restrained three or more times. Next, a group of 31 youths were randomly selected from a list of patients who were hospitalized during this period but were never restrained. Excluded from our study were youths who were hospitalized less than 48 hours. The charts of each patient selected for the study were reviewed, and additional information was collected for each restraint incident. For participants with multiple admissions during the study period, data for the first admission was used to determine the basic demographic characteristics, psychiatric history, education placement, and previous aggression. The procedure called for notation of any change in guardianship or living arrangements between admissions, but none occurred.
Instruments
Two data collection instruments were used in this study: a chart audit form and a scale that rated aggression in the six months before hospitalization. The chart audit form was designed to collect history of maltreatment, history of aggressive behavior six months before admission, and diagnostic and demographic data. Also categorized on the form were the restraint incident, the behavior or incident that prompted restraint, and the interventions that were attempted before using restraint. Restraint was defined as involuntary restriction of the patient's movement by the use of mechanical devices on four limbs of the patient's body. The 17 patient-specific categories (demographic characteristics and history) and incident-specific categories (place, time, and restraint episode descriptors) listed on the chart audit form were modeled after a form described by Way (
19) for restraint studies in the New York State psychiatric hospital system and used in subsequent large-scale studies of restraint on child and adolescent units (
7,
20).
The youth's preadmission aggression was scaled with a tool that categorizes a youth's aggression on the basis of his or her behavior six months before hospitalization (
21). Possible ratings range from 1 to 6, with higher ratings indicating more severe aggression that resulted in the victim's serious injury (level 5) or death (level 6). The anchors for each aggression level include a description of the behavior as well as its potential lethal consequences.
Results
As shown in
Table 2, the sample of 100 youths was predominately male (66 percent) and African American (77 percent). The mean±SD age was 13.9±2.39 years, ranging from seven to 19 years. Most youths in the sample were insured through Medicaid (77 percent). Approximately half (49 percent) lived with at least one biological parent, and a majority (51 percent) lived in nontraditional or custodial living situations. A majority (53 percent) had previous psychiatric hospitalizations, and 29 percent had multiple admissions during the study period. At the time of discharge, 83 percent of youths were taking some form of medication for their mental health problem.
More than a third of the sample (41 percent) had several diagnoses, typically either a dual diagnosis of a substance use disorder and another mental illness or a combination of mood and behavior disorders. This group of youths had a significant history of abuse and aggression in the six months before hospitalization. Almost three-quarters of the sample (74 percent) had a history of abuse, that is, physical or sexual abuse, neglect, or exposure to domestic violence. Sixty-five percent of the youths displayed significant aggression within the six months before hospitalization: 49 percent had level 4 aggression (contained incidents of mild assault, that is, hitting, pushing, and scratching) and 16 percent had level 5 aggression (incident resulted in an injury in which the victim required medical care).
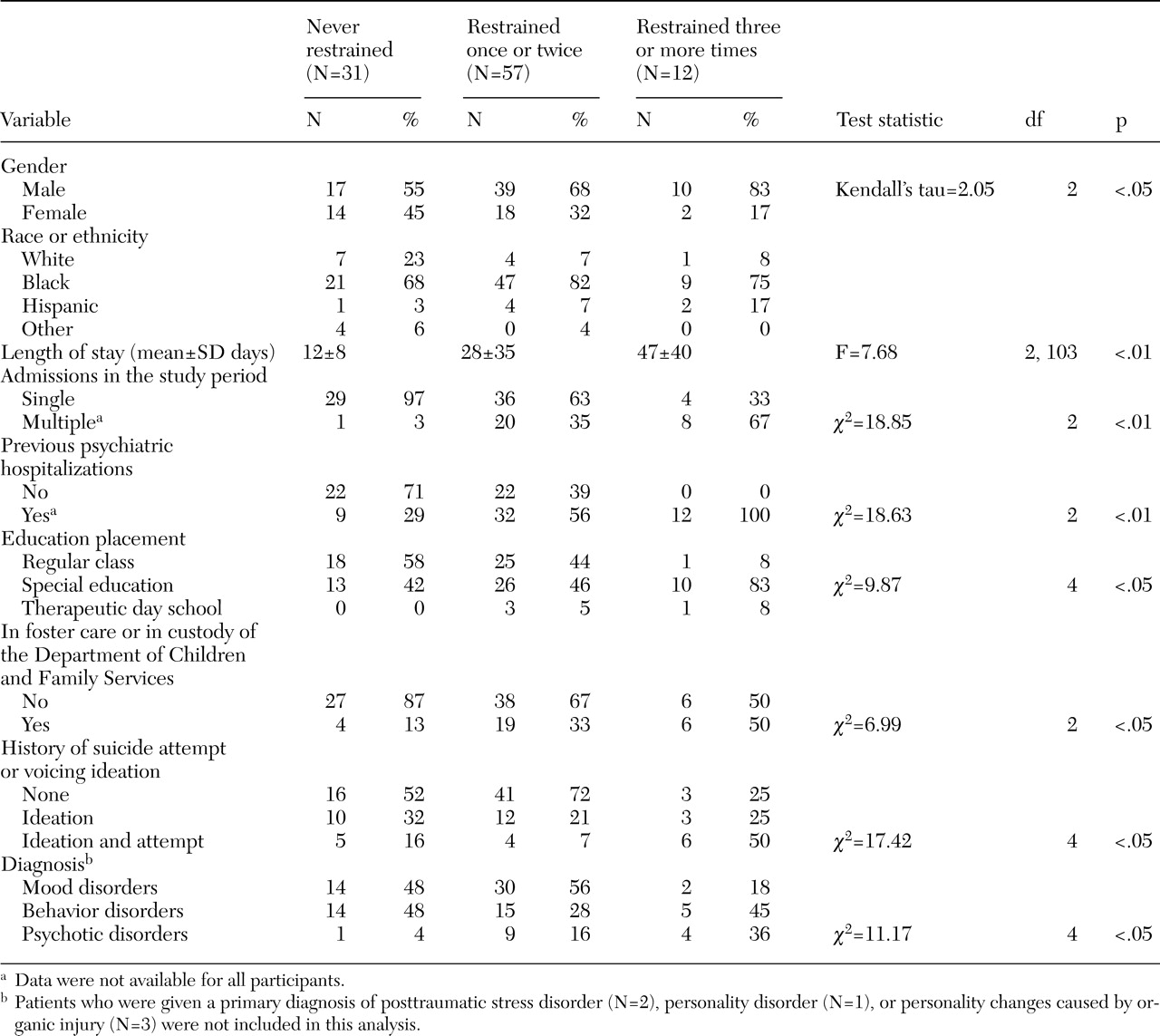
Cross-group analysis was conducted to examine the relationship between the use of restraint and characteristics of the youths. As displayed in
Table 2, several significant relationships were found. The rate of restraint was significantly higher for males than for females. Youths with a longer stay or with multiple admissions to the facility during the study period were significantly more likely to be restrained. A significant relationship was found between being restrained and having voiced suicide ideation and attempted suicide. Youths who had been restrained were more likely to attend a special education program or to be in foster care or in custody of the Department of Children and Family Services (DCFS).
To examine trends in diagnosis, three categories of primary diagnoses were created: psychotic disorders, mood disorders, and disruptive behavior disorders. The psychotic disorders category included youths with psychosis, schizophrenia, and schizoaffective disorders. The mood disorder category included youths with bipolar disorder and depressive illness. The disruptive behavior disorders category included youths with intermittent explosive, impulse control, attention-deficit, and oppositional defiant disorders. Three diagnostic categories were not included in the analysis of primary diagnosis because of the small number of youths in each category: posttraumatic stress disorder (two youths), personality changes caused by organic injury (three youths), and personality disorder (one youth). Youths who had been given a diagnosis of a psychotic disorder were significantly more likely to be restrained. In fact, 93 percent of these patients (13 of 14 youths with a psychotic disorder) were restrained during hospitalization. Characteristics that were not significantly related to restraint included age, history of abuse, aggression before hospitalization, race or ethnicity, payment type, and the family configuration in which the youth resided.
The 12 youths who had been restrained three or more times shared a particular profile. Eight of these youths (67 percent) had multiple psychiatric admissions during the study period. All 12 had a previous psychiatric hospitalization. Eleven of the youths who had been restrained three or more times (91 percent) received special education, compared with 13 youths who had not been restrained (42 percent). Finally, compared with youths who had not been restrained, those who had been restrained three or more times were more likely to be in foster care or in DCFS custody (six youths, or 50 percent, compared with four youths, or 12 percent) and more likely to have history of voicing suicide ideation and attempting suicide (six youths, or 50 percent, compared with five youths, or 16 percent). This group of 12 youths, just 17 percent of the restraint group, accounted for 44 percent of the restraint incidents.
One of the questions explored in the study was whether setting was associated with the use of restraint. To this end we examined the 120 restraint incidents for any trends in the time of day, day of the week, place, or programming. The mean time that the youths were in restraint was 4.1±2.1 hours. No setting variable surfaced as being related to restraint. Nearly a third of the restraint incidents were initiated in the day area (42 incidents, or 35 percent), but they were initiated almost equally in the child's bedroom (36 incidents, or 30 percent). Restraint incidents occurred almost equally during programming (47 incidents, or 39 percent) and during quiet time in the patient's room (37 incidents, or 31 percent). Of the four units studied about half the patients who were restrained (29 youths, or 42 percent) were admitted to one of the adolescent units, which treated youths aged 12 to 17 years old.
No trends were found in the day of the week that restraint incidents occurred, but we did find some clustering of restraint incidents during particular times of the day. Seventy-nine of the restraint incidences occurred in the early afternoon (27 incidents, or 23 percent), in the midafternoon (26 incidents, or 22 percent), and in the early evening (26 incidents, or 22 percent), whereas restraint incidents rarely occurred in the early morning (eight incidents, or 7 percent) or during sleeping hours (two incidents, or 2 percent). Incidents occurred almost equally midmorning (15 incidents, or 13 percent) and midevening (16 incidents, or 13 percent). Twelve of the restraint incidents (10 percent) occurred when the day and evening staff members were changing shifts (3 p.m. to 4 p.m.). Approximately one-quarter of the restraints (32 incidents or 27 percent) occurred within the first three days of a patient's hospitalization; 15 of these occurred on the day of admission.
The three behaviors, often occurring in concert, that were the most prevalent impetus to restraint were patient's agitation (75 incidents, or 63 percent), threats (88 incidents, or 73 percent), and assault (75 incidents, or 63 percent). Included in the chart audit were brief descriptions of the incidents that prompted restraint. For the most part these altercations had an extremely violent character, including combative behavior, striking out at staff, attempting to escape, hitting peers, and kicking doors and windows. Also noted as an impetus to restraint use were instances in which the patient was observed to be paranoid and delusional.
We examined the interventions that were attempted before restraint use. Staff documented that they attempted several interventions with each patient before the restraint; verbal intervention and therapeutic holding (37 incidences, or 31 percent) was the most likely combination. Therapeutic holding, a form of nonviolent physical intervention that lasts for short periods of time, was used before 93 instances of restraint (78 percent). Open seclusion was used before 48 incidents (40 percent), and PRN (as needed) medications were given in 45 instances before restraint (38 percent) and 26 times during restraint incidents (22 percent).
Discussion
One aim of this study was to determine whether a particular group of youths was at risk of restraint and how this risk profile has changed over the past ten to 15 years. Our findings indicate that several characteristics of at-risk youths have not changed. Specifically, youths who are restrained are still more likely to be male, have a longer hospital stay, or have previous psychiatric admissions. Because a critical factor in staff members' decision to restrain is their perception of the dangerousness of a situation (
22), one explanation for the greater restraint of males is that inpatient males are generally more aggressive (
21,
23), which may make their behaviors more threatening. However, this finding should be considered with some reservation. In a recent study of hospitalized youths, males and females demonstrated similar levels of aggression (
24). Also, in two recent studies of restraint procedures, no significant difference was found in the rates at which males and females were restrained (
25,
26).
Our findings also align with inpatient studies that reported that youths with previous psychiatric treatment, multiple admissions, or longer stays were more likely to be restrained (
8,
9,
11). It is possible that the youths who were restrained had more serious emotional difficulties that required more frequent and lengthier hospital stays. Unfortunately, we did not collect data on severity of illness, which makes it difficult to support this interpretation. An alternate explanation is that most youths in our study were from a racial or ethnic minority group (80 percent) or received public assistance (77 percent). These youths may have required more frequent and lengthier inpatient services because of a lack of outpatient resources. Nationwide, youths from racial or ethnic minority groups have less access to outpatient services and demonstrate greater use of inpatient services (
27). Also, a recently completed analysis of rehospitalization rates of youths in DCFS custody in Illinois found that those who were readmitted to hospitals received fewer services after being discharged (
28).
Our findings differed with previous studies that identified youths with disruptive behavior disorders as being at risk of restraint (
9,
10). In our study youths with a psychotic disorder were at greatest risk of restraint during inpatient treatment. Interestingly, this group of youths was also identified as being at risk of restraint in a recent study conducted in Finland (
25). The literature does not contain any research that indicates that these youths have increased their inpatient service use in the past ten years; the only recent study of pediatric inpatient hospitalization by diagnosis considered cost but not absolute numbers (
29). However, an increasing number of youths are using psychiatric emergency services (
30). Gutterman (
31) believes that youths who appear at emergency departments exhibiting psychotic symptoms are more apt to be hospitalized because they are viewed as less able to control their behavior and to be in need of medication initiation. The inpatient literature on aggression management has given little attention to youths with psychotic features; yet the management of their behavior can be complex (
32), and our study would indicate that their behavior puts them at risk of restraint.
Youths in foster care or in DCFS custody were identified as a new group that was at risk of restraint. Again, this finding was collaborated in a recent study of restraint among youths in Finland (
25). Why would this group of youths be at particular risk of restraint? Researchers have noted the significant aggression and emotional regulation difficulties of youths who have had multiple caretakers (
33,
34). Others suggest that the regulation problems of these youths reflect the additive effects of the stress, family turmoil, and sometimes maltreatment that make behavior management during inpatient treatment particular challenging (
15).
Data from this study also provide a unique look at the types of youths who are hospitalized on inner-city psychiatric units, the types of behaviors being handled, and the techniques being used to deescalate violence. This sample of youths is noteworthy in that 65 percent of the youths in our study displayed serious aggression six months before admission, 40 percent had a history of attempting suicide or having suicide ideation, and 75 percent had a history of maltreatment. The violent nature of the incidents that led to restraint was startling. More than 75 percent of the incidents involved some form of assault. Although deescalation techniques should be taught as a first-line approach for dealing with volatile incidents, as one aggression guideline suggested, interventions should be matched with the intensity of the presenting behavior (
16).
Two interventions are in particular need of further research: therapeutic holding and PRN medication. In this study, therapeutic holding was frequently used before restraint. How often are these holds instituted for brief periods before PRN medication is given? Does therapeutic holding sometimes prevent a restraint? Research is needed to understand how therapeutic holding is being used to control aggression and to what gain, because the physical risks of prolonged therapeutic holding mirror the physical risks involved in physical restraint (
35).
In this study PRN medication was used before 38 percent of restraint incidents. With the data available, it was impossible to determine why it was used in these particular situations or why it did not prevent the restraint incident. Wynn's (
36) findings suggest that physical restraint is used in more violent situations, in which there is a fear of injury, but that pharmacological restraint is used when staff members perceive that they have some time to allow the interventions to work. PRN medications should not be used as a chemical restraint; however, more research is needed to understand the potential of PRN medication to quell volatile situations and prevent seclusion and restraint (
37).
This was a small, single-site study, which limits any generalizations. Lack of associated data made several study variables difficult to interpret. The finding that youths in special education were more likely to be restrained was difficult to interpret because we did not have any data on the specific neurocognitive deficits of the youths; psychological and educational test scores was absent from many records.
Our data suggested that restraint was more likely to occur at the beginning of hospitalization and in the afternoon hours. Without data on ward organization or interaction patterns, it was difficult to interpret these findings. Finally without a severity of illness score our explanation was limited for why a youth would be restrained three or more times. Our only explanation is that these youths were more likely to be in special education, be in foster care or DCFS custody, and have a history of previous psychiatric treatment.
Conclusions
As the mental health professions continue to craft means to reduce restraint, researchers should not ignore the reality that staff members face in managing highly aggressive youths. Particular attention should be paid to youths who are at risk of restraint and the use and efficacy of techniques to reduce aggression, particularly PRN medications and therapeutic holding.
Acknowledgment
The authors are grateful for support from the research resource fund of Rush University, College of Nursing.