The study was conducted at the outpatient treatment program for borderline personality disorder at the department of psychiatry at the University of Geneva. The program began in 1998. The study ran from the beginning of January 2000 until the end of December 2001. Fully informed, written consent was obtained from all participants. Helsinki principles were followed.
Participants
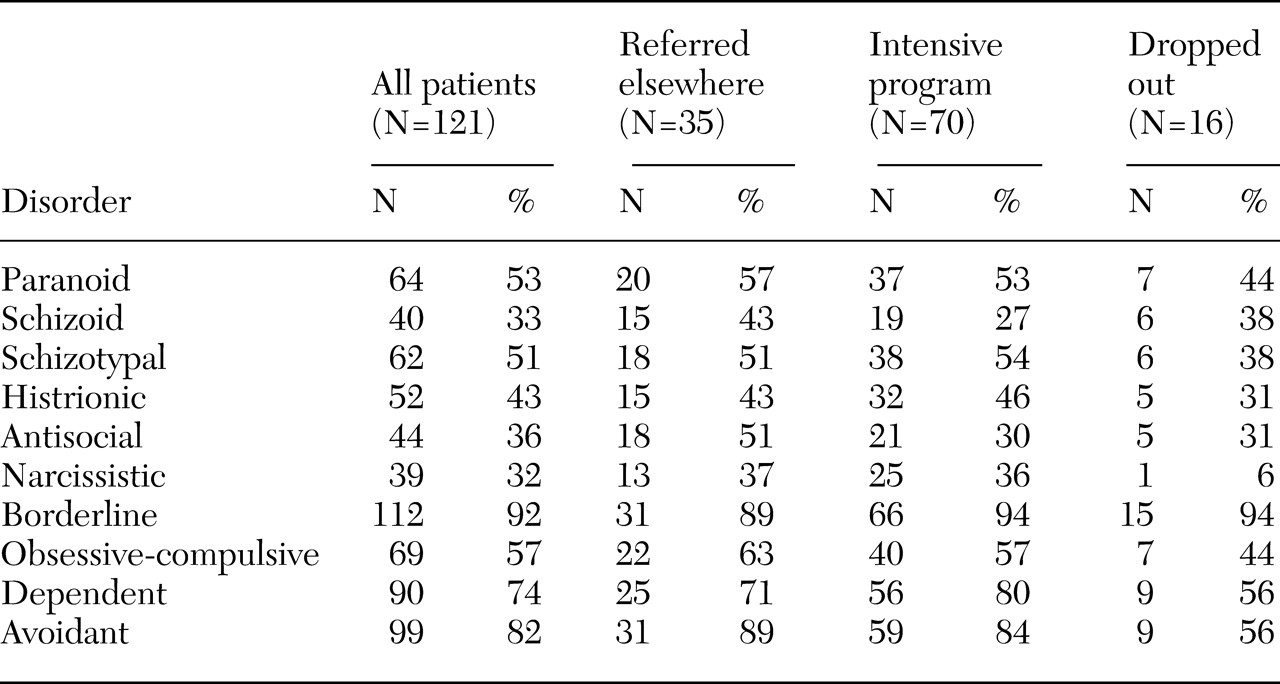
Data for all patients who were referred to our treatment program during the study period are included in this report. During the study period, 127 patients were referred to the intensive program—103 women (81 percent) and 24 men (19 percent). The patients were between the ages of 18 and 52 years (mean±SD= 30.7±8.1). Their mean educational level was equivalent to 12 years of study (mean=11.6±2.1), which comprised nine years of obligatory schooling followed by an apprenticeship, vocational training, or college. Sixty-four patients (50 percent) were single, and 41 (32 percent) had a professional activity. The number of lifetime hospitalizations ranged from 0 to 44 (mean=3.3±6), and the total number of days hospitalized ranged from 0 to 431 (mean=54±92.4). The mean age of first admission for the sample was 29±7.6 years. All patients had had previous psychiatric treatment, often in emergency services.
The program does not admit patients who present spontaneously; all patients must be referred by a physician. The program admits patients whose main problems are recent suicidal or parasuicidal behavior, severe impulsive disorders, anger problems, or multiple therapeutic failures in other treatment programs. The number of places in the program is limited. Patients who were considered to be the most suicidal were preferentially offered admission. The relative risk of suicide was determined by the receiving clinician. A total of 100 patients (79 percent) had made at least one suicide attempt (lifetime prevalence), and 112 (88 percent) had a history of at least one parasuicidal act, defined as intentional self-injury either with or without intent to die. Patients whose principal problem included a psychotic disorder, bipolar disorder, developmental disturbance, substance dependence, or an eating disorder were not considered for admission to the program. After assessment, 87 patients (69 percent) were admitted to the program. The other 40 patients (31 percent) were referred for treatment elsewhere.
Of the 87 patients who were admitted, 71 (82 percent) completed the program and 16 (18 percent) dropped out. The patients who completed the pre- and post-measures were considered to have completed the program.
At the end of the treatment period, all patients, including those who dropped out, were referred for further treatment. In some cases the recommendation was to repeat the intensive program. Only data for patients' initial participation in the program were included in the study.
Program description
The program is located in an outpatient unit that is a hybrid of a day hospital and a crisis center. The center is open 24 hours a day, 365 days a year. Patients may spend a maximum of two consecutive nights in the center, on a purely voluntary basis, and thus avoid hospitalization. After initial assessment, patients retained in the program may benefit immediately from crisis support, which is particularly useful at night and on weekends.
The intensive program is an adaptation of dialectical behavior therapy and offers individual and group therapy as well as a consultation team for therapists. All patients have an individual therapist who works with them to define one—or occasionally more—behavioral targets that will be the focus of treatment. These targets are selected within a strict dialectical behavior therapy framework, that is, suicidal behaviors are treated as a priority, followed by behaviors that interfere with therapy, and then by behaviors that interfere with quality of life. Given the short duration of the program, behavioral targets that are further downstream, such as decreasing behavior related to post-traumatic stress and increasing self-respect, are less frequently the focus of treatment.
The intensive program lasts for three weeks. Groups are organized on four of the five weekdays, for two to four hours each day, for three weeks. Most group work consists of behavioral skills training, which is taught intensively for a total of about six hours a week. The skills cover the four modules of dialectical behavior therapy—mindfulness, interpersonal effectiveness, emotion regulation, and distress tolerance, with a particular emphasis on mindfulness. In addition, groups are held before and after each weekend to deal with contingency management, skills generalization, and problem solving. A separate group teaches behavioral chain analysis, and another group helps patients to identify and name bodily sensations and emotional responses and to generalize mindfulness skills. All groups encourage behavioral rehearsal and, when appropriate, exposure.
Availability of limited telephone contact with therapists is another important feature of treatment. Patients participating in the program are given a special number to call. Between 8.30 a.m. and 6 p.m. a team member will route the call to their therapist if necessary, deal with crisis situations, encourage attendance, and help with skills generalization. Outside of these hours, patients may call the center for crisis support, but their call will be dealt with by the nurse on duty.
The primary therapist does not prescribe or manage psychotropic medications. All patients are evaluated for and offered medication as appropriate by one of the psychiatrists in the program.
Patients receive 13 hours of group therapy a week plus individual sessions. However, to maximize generalization to the natural environment, the program offers patients a very supportive environment but not occupational therapy. When patients are not actively in treatment they are encouraged to pursue their own lives, look for employment, and so forth.
The program therapists are two psychiatrists, one clinical psychologist, and five nurse clinicians. The psychiatrists and three of the nurse clinicians have received intensive training in dialectical behavior therapy. Training for the other team members is provided in ongoing weekly theoretical and case supervision sessions. In accordance with the principles of dialectical behavior therapy, all therapists are obliged to attend weekly team meetings, which include mindfulness practice.