Police officers are recognized as first responders for individuals who are experiencing a mental illness crisis (
1,
2,
3,
4). In the absence of specialized training in mental illness and knowledge about the local treatment system, such crises may end in arrest and incarceration when referral and treatment might be more appropriate (
5,
6). The absence of collaboration between law enforcement and mental health systems has been posited as one factor in the emergence of the complex phenomenon known as the criminalization of persons with mental illness (
7,
8,
9).
Partnerships between law enforcement and mental health systems may address this problem. One such collaboration is the crisis intervention team (CIT) model, started in 1988 by the Memphis Police Department (
10). The CIT program provides intensive training about mental illness and the local system of care to patrol officers, who then are available to respond to mental disturbance calls. The idea has spread nationwide, and approximately 70 departments have formed their own CIT programs (personal communication, Cochran S, October 9, 2004).
Although clearly intended to increase officers' skills in deescalation of crises among persons with mental illness, CIT partners may seek different—although complementary—outcomes. Law enforcement may be most interested in improving the safety of both officers and consumers during potentially dangerous encounters, whereas mental health may focus more on decreasing inappropriate arrests of persons with mental illness.
In this article, we examine disposition of mental disturbance calls before and after implementation of one city's CIT program. The purpose of the study reported here was to determine whether CIT-trained officers were more likely than non-CIT-trained officers to respond to calls involving individuals with mental illness who were experiencing a crisis by transporting the person to a health care facility and less likely to either arrest the person or leave the person at the scene. Furthermore, for cases in which an officer determined that transportation to a treatment facility was necessary, we examined whether the transportation to treatment was voluntary or involuntary, by officers' CIT training status.
The program in Akron, Ohio, began in May 2000 with the collaboration of the Akron Police Department; the Summit County Alcohol, Drug Addiction, and Mental Health Services Board and its provider agencies; the National Alliance for the Mentally Ill (NAMI) of Summit County; the Summit County Recovery Project; and the Northeastern Ohio Universities College of Medicine (NEOUCOM). Two major modifications were made to the Memphis program to account for differences in services available. Akron, unlike Memphis, has a freestanding psychiatric emergency service, which means that individuals who have a comorbid nonpsychiatric medical condition may be referred to a general hospital emergency department instead of or before going to psychiatric emergency services. In addition, Akron's emergency medical services dispatch a paramedic unit to emergency calls identified as involving persons with mental illness. In general, emergency medical services are in charge of nonpsychiatric medical calls, and the police are in charge if a call is due primarily to manifestations of mental illness without comorbid medical complications. As a result, paramedic lieutenants from the Akron Fire Department were included in initial training.
The first weeklong training occurred in late May 2000 with 20 Akron police officers and three paramedic lieutenants from the Akron Fire Department. All officers were volunteers and were screened by the training director to determine their appropriateness for this team of officers who were most likely to encounter individuals experiencing mental illness crises. Communication skills and being self-motivated to improve skills and knowledge about mental illness were the prime selection criteria for the program. Officers received a 40-hour introduction to mental health and mental illness with an intensive overview of the local mental health system and its points of access. Officers visited psychiatric emergency services, went into the community with case managers, and visited a consumer-directed social center. They received extensive training in verbal deescalation skills and engaged in realistic role playing to practice these skills in simulated crises at the NEOUCOM Center for the Study of Clinical Performance. Officers were encouraged to consider, when appropriate, linkage and referral for care to the mental health system as a preferable alternative to arrest.
CIT-trained officers began patrolling in the Akron community on May 27, 2000. Training was provided annually for new team members. Excluding officers who have been promoted or have retired, currently 66 of 243 active patrol officers (27 percent) are CIT trained (personal communication, Yohe M, July 29, 2004). In addition to training for officers as detailed above, refresher training sessions have been held annually since 2003. These sessions are for supplementary mental health training and to identify areas in program implementation where difficulties exist for officers and the people they serve. Modified annually, the two-day refresher course has included updates on legal and medical issues, research results, advanced techniques in negotiation and suicide prevention, and taser techniques, procedures, and qualification.
CIT officers handle situations they encounter on patrol or through dispatch. Dispatchers evaluate emergency calls and have two codes for mental disturbance calls: suspicion of mental illness and suicide attempt in progress. Once on the scene, responders may determine that the call does not involve a person with mental illness. Conversely, other codes—for example, fights—may involve a person with mental illness but may not be coded by dispatchers as a call related to a mental disturbance.
Methods
We obtained institutional review board approval from all applicable agencies before beginning the project. Data were analyzed for the two years before and the four years after implementation of the CIT program by using SPSS, version 12.0. The Akron Police Department provided data on the number of calls for assistance. All calls that were coded as mental disturbance calls by police department dispatchers from May 1998 through April 2004 were made available to the research team. These calls included the call date, the time, whether CIT team members were present, police code corresponding to disposition of the call, and notes from the Akron Police Department and emergency medical services. Notes were evaluated to determine disposition location and information about which agency was in charge of the call (the Akron Police Department, emergency medical services, or another agency, such as the coroner, the local jail, or a mental health agency). Notes were consulted to determine whether the officer who transported the individual to a treatment facility initiated an involuntary commitment process.
The number of calls for assistance per month and the number of calls related to a mental disturbance per month were summed per year (May through April), and the rate of mental disturbance calls per 1,000 Akron police department calls per month was calculated. Analysis of variance (ANOVA) statistics were calculated. If the means were significantly different at the p<.05 level, one-way ANOVA Scheffé's post hoc tests were run to identify categories of difference. Compared with other tests, Scheffe's is a conservative estimate, because larger differences in means are required for significance.
Percentages and chi square statistics were calculated for the dispositions of calls by time and training. Time was dichotomized as either the two years before implementation of the program (May 1998 through April 2000) or the four years after (May 2000 through April 2004). Training was dichotomized as either CIT-trained or non-CIT-trained. Analysis of variance was calculated on the basis of disposition proportions. If the means were significantly different at the p<.05 level, Scheffé's post hoc tests were run to identify categories of difference.
Results
Proportion of mental disturbance calls
From May 1998 through April 2004, the Akron Police Department received 1,527,281 calls for service, of which 10,004 were related to mental disturbances. The average number of calls per month (21,212) was stable over the six-year study period (data not shown). The total number of calls per year increased slightly over the six years, although not significantly. The two years before implementation of the program and the year of implementation were significantly different from the last two years studied (p<.006). There was an absolute increase in the number of calls identified as mental disturbance calls and in the rate of calls related to mental disturbances per 1,000 calls for assistance (F=9.39, df=5, p≤.001) as well as a proportional increase (F=15.86, df=5, 66, p≤.001).
Disposition of calls for mental disturbances
Initially there were seven disposition categories: transport to psychiatric emergency services; transport to another treatment location, such as an area hospital or detoxification facility; transport to a jail; police interaction with no need for transport (for example, giving advice, assisting, or talking to the person); other transportation (including to a shelter or residence); no police interaction (for example, the officer was unable to locate the individual); and disposition unknown. Over the six-year period, almost 25 percent of the 10,004 mental disturbance calls resulted in transportation to psychiatric emergency services, and 31 percent resulted in transportation to local hospitals or another treatment facility. Thirty-two percent of the calls involved police interaction with no need for transport. Almost 3 percent of the calls resulted in an arrest. Slightly fewer than 8 percent resulted in no police interaction, and 2 percent involved some nontreatment transport; in less than .5 percent of the calls the disposition was undetermined.
We continued our analyses with four disposition categories: transport to psychiatric emergency services, transport to another treatment location, transport to jail, and police interaction with no transport. The other three categories were not analyzed, because these three disposition categories do not appear relevant to understanding police interaction with individuals who are mentally disturbed. Eliminating these categories decreased the sample size by about 10 percent to 8,985.
Disposition by officers' CIT training status
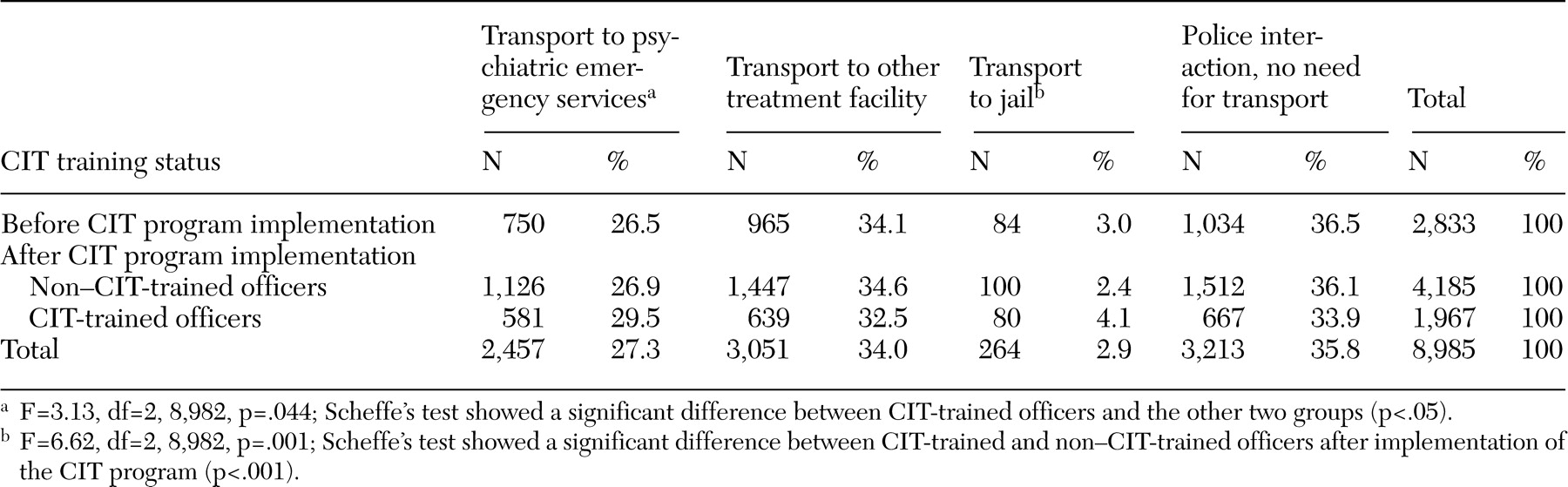
Table 1 is a cross-tabulation of the four disposition categories by time and training: before the CIT program, non-CIT-trained officers after implementation of the CIT program, and CIT-trained officers after implementation of the CIT program (χ
2=21.58, df=6, p=.001). After implementation of the program, the overall rate of transport to jail decreased slightly, from 3.0 percent to 2.9 percent. When we compared the two groups of officers after implementation of the program, CIT-trained officers were more likely than non-CIT-trained officers to have transported persons with mental disturbances to jail (4.1 percent compared with 2.4 percent), although the difference was not significant. When CIT-trained officers' interactions were compared with those of the other two groups, CIT-trained officers were also more likely to have transported persons with mental disturbances to psychiatric emergency services and less likely (although not significantly less) to have transported them to other treatment facilities. CIT-trained officers were also less likely to have interactions involving no need for transport than were other officers, either before or after implementation of the CIT program, but, again, the difference was not significant.
The fact that emergency medical services were in charge in the case of some of the calls may have masked the effects of training, because there may not be opportunities to use deescalation techniques in emergency settings.
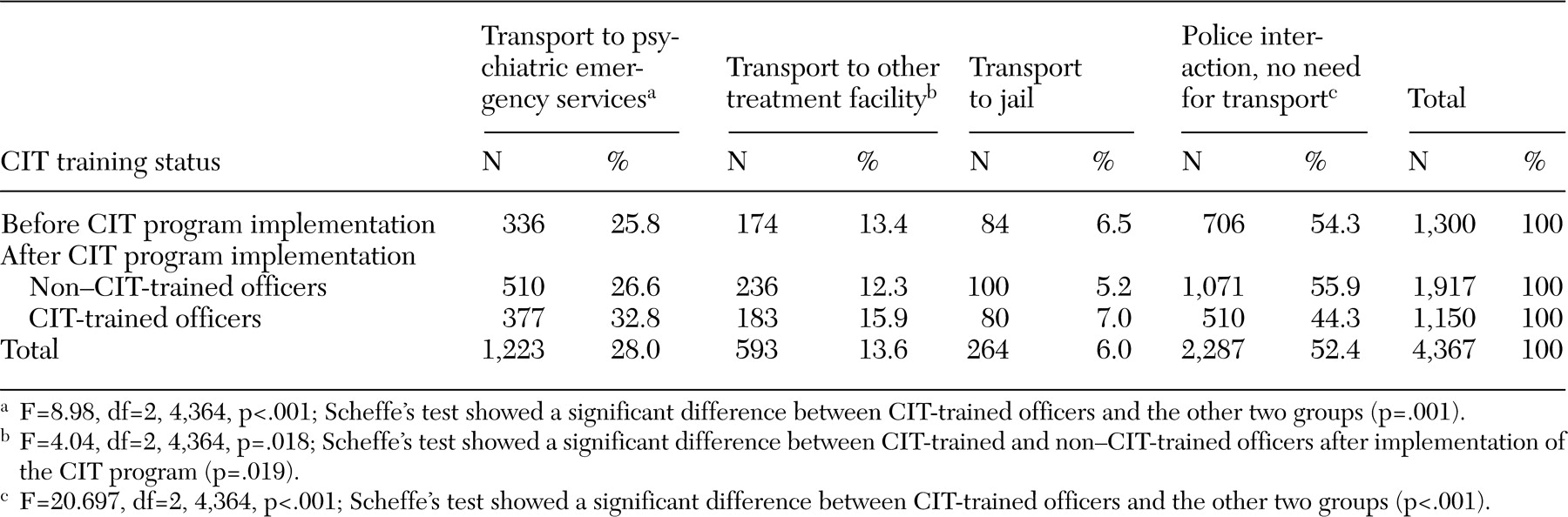
Table 2 shows dispositions by officers' CIT training status after removal of these nonpsychiatric medical calls (N=4,367). With these calls excluded, there was no longer a significant difference in arrest rates between the three groups, which suggests that training status did not affect arrests. However, CIT-trained officers were significantly more likely than either of the other two groups to take mentally disturbed persons to psychiatric emergency services and less likely to be involved in calls for which there was no need for transport. Compared with non-CIT-trained officers for the period May 2000 through April 2004, CIT-trained officers were significantly less likely to be involved in calls for which there was no need to transport the individual.
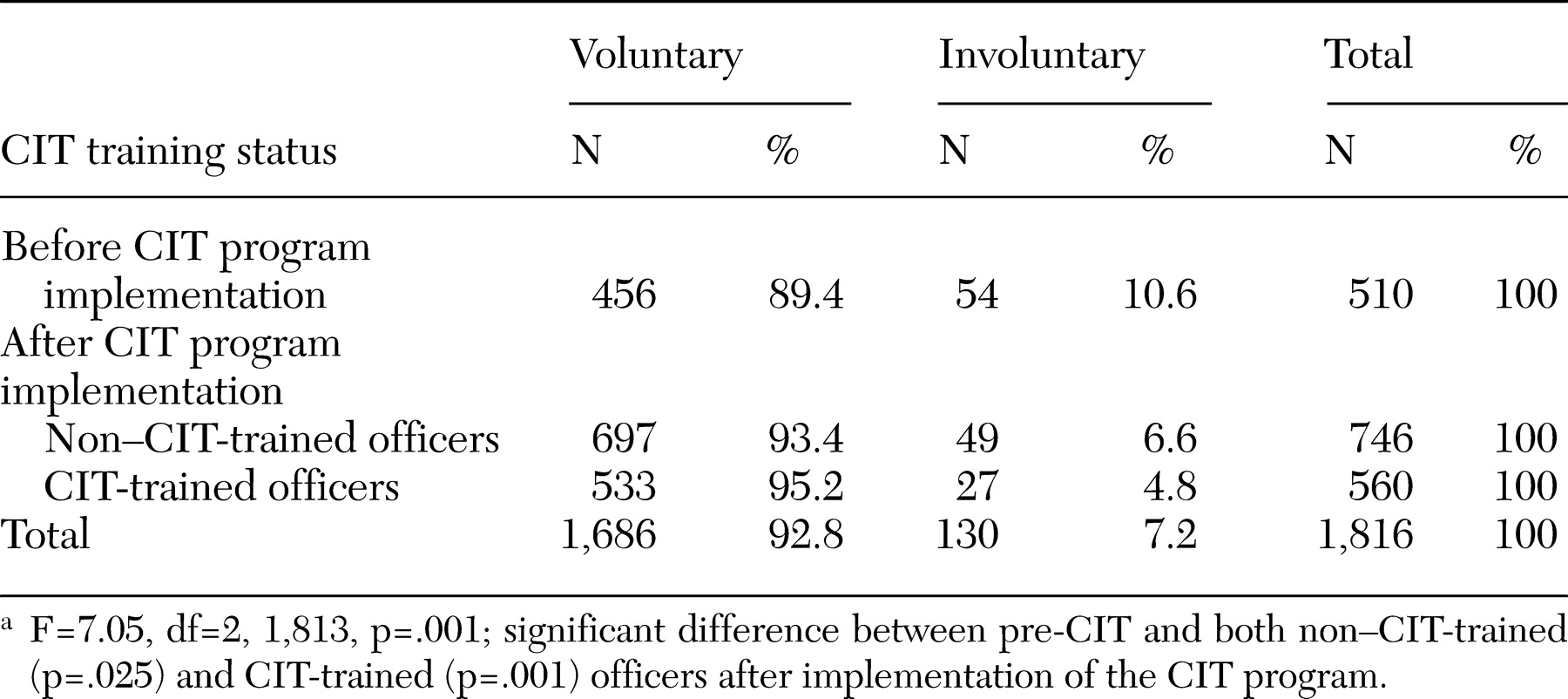
Before implementation of the CIT program, 10.6 percent of people who were transported for treatment were transported on an involuntary legal status. There was a significant decrease in the involuntariness of transport after implementation of the program for both non-CIT- and CIT-trained officers, as can be seen from
Table 3.
Discussion
Since the CIT program began, there has not been an increase in the volume of all calls, but the absolute number of mental disturbance calls and the proportion of such calls have increased. We suspect at least two possible explanations for this increase in the number of calls related to mental disturbances after implementation of the CIT program. First, the dispatchers may have been more aware and better prepared to assess a call as involving a person with mental illness. Second, with the community's knowledge of the CIT program and the participation of NAMI, callers may have been more likely to acknowledge the involvement of a person with mental illness. Since the program began, family members have reported that they are more comfortable calling the police to request help for a loved one, and consumers of mental health services have reported calling the police to request help for themselves or their peers.
A number of findings suggest that the program is meeting the desired outcomes for both sides of the partnership. Compared with nontrained officers, trained officers are more likely to transport a person for treatment than they were before the program was implemented. Training effects may explain this difference, given that recognition of symptoms of mental illness and knowledge of options for treatment are part of CIT training.
The study showed that trained officers are less likely to end calls without arranging for transport of the person involved. This issue is complex. Police officers on the scene have considerable discretion (
1,
11). For officers in general, the less time-consuming course is to rule out an emergency and resolve the call without arranging transport. CIT-trained officers presumably appreciate the fact that timely intervention in the treatment system may prevent future emergencies, even if the situation at hand does not mandate transport. On the other hand, CIT-trained officers may use their training to deescalate and counsel individuals so that no further emergency intervention is needed. As CIT has evolved in Akron, the police and mental health systems have been developing outreach programs so that people who may not need emergency mental health intervention receive appropriate mental health follow-up. The effects of such programs on the rate of calls that do not involve the arrangement of transport remain to be seen. At this point, however, it appears that the significant difference in the rate of calls that did not involve transport between CIT-trained and non-CIT-trained officers reflects a desired outcome.
We cannot explain with certainty the observation that after implementation of the CIT program there was a decrease in involuntary transports for both CIT- and non-CIT-trained officers. It may be that the emphasis during training on use of verbal deescalation techniques to avoid escalation of crises filtered throughout the department, or it may be that CIT-trained officers are referred the more challenging cases, which could mask the effects of training. In any case, all stakeholders perceive this outcome as a positive one.
The apparently higher rate of arrest by CIT-trained officers was unanticipated. Mental health systems support CIT programs in part because they view the programs as prearrest diversion programs. Police agencies, on the other hand, embrace the CIT program as a means of enhancing officer and community safety. Through CIT training, officers may learn when referral to the mental health system is most effective and when arrest may be preferable. As noted above, it is possible that dispatchers are sending CIT officers to the most challenging mental disturbance calls, for which officers may have less discretion as to whether to arrest the individual. That this might be the case could be supported by the fact that the initially significantly higher arrest rate by CIT-trained officers disappeared and differences in significance between CIT-trained and other officer groups in both transport to other treatment and no need for transport appeared after calls handled by emergency medical services were excluded from the analyses. Emergency medical services handled 54 percent of calls attended by non-CIT-trained officers both before and after the CIT program was implemented but handled only 42 percent of calls attended by CIT-trained officers. Removal from the data of primarily nonpsychiatric medical calls, for which officers lack discretion about disposition, clarified the differences between the groups of officers. CIT-trained officers' arrest rates were not significantly different from those of the other officer groups, but the CIT-trained officers transported mentally disturbed individuals to treatment facilities more often.
Furthermore, it is likely that Akron arrest rates are influenced by officers' knowledge of the Mental Health Court postarrest diversion program. The Akron Mental Health Court began in January 2001, shortly after the start of the CIT program (
12,
13). This court is for misdemeanants with severe and persistent mental illness who receive intensive community-based treatment in lieu of incarceration. Court personnel participate in CIT training to explain the program and to encourage officers to refer the individuals they arrest to the mental health court. Knowledge of the program and the fact that it may help individuals who may otherwise be resistant to treatment to live successfully in the community may result in CIT-trained officers' choosing arrest in selected cases. The interaction of prearrest diversion programs such as the CIT program and postarrest programs such as the mental health court should be the subject of future research.
Given that these results are not based on experimental data, it is not possible to make causal assertions about the effects of police training on dispositions. That is, officers were not randomly assigned to training. Furthermore, officers were acting as their own controls by using the pre-CIT program as a comparison group. Ideally, we would have liked to have similar data from a community that did not have a CIT program as an additional comparison group. Despite these limitations, the findings are important.
In addition, future research should consider the effects of the circumstances surrounding the call. A complementary study that examined qualitative CIT-trained officers' field reports (manuscript in preparation) had similar findings, suggesting that although CIT programs may have a significant impact on police referral for treatment and decreased use of force and involuntary commitment, these programs may not reduce arrests of people with mental illness. Only a study of the circumstances of each arrested individual, the nature of the charges, and the officer's rationale for arrest will help explain these findings. Future examination of narrative reports on each CIT encounter will address these questions.
CIT programs require a partnership between law enforcement and mental health systems as well as consumers of mental health services and their families. Each stakeholder group may desire overlapping but somewhat different outcomes. It is likely that CIT programs will differ depending on the mental health and criminal justice systems' community resources. As data accumulate on the effectiveness of CIT programs, communities will need to decide whether the outcomes warrant the considerable investment in the program. If CIT enhances the safety of both officers and consumers but does not reduce the arrest rate, for example, will courts and jail administrators support it?
Conclusions
The implementation of a crisis intervention team (CIT) program for police officers has led to an increased number and proportion of calls recognized by police dispatch as potentially involving mental illness. Training has led to increased transport of persons who are experiencing a mental illness crisis to emergency evaluation and treatment facilities, and transport is more likely to be on a voluntary basis compared with officers who have not participated in the training. This finding suggests that the CIT partnership between the police department, the mental health system, consumers of services, and their family members can help in efforts to assist individuals who are experiencing a mental illness crisis and interacting with the criminal justice system to gain access to the treatment system, where such individuals most often are best served. The expected effects on arrest rates were not clearly demonstrated. Future research is needed to examine decisions to arrest and to understand the interactions between multiple programs such as CIT and mental health courts and to learn how different CIT program elements lead to desired outcomes.
Acknowledgments
This research was supported by the Ohio Department of Mental Health (grant 02.1176) and the Ohio Office of Criminal Justice Services (grant 2002-DG-C01-7068). The authors thank the following officers of the Akron Police Department for their assistance and patience: Lt. Michael Woody (Ret.), Sgt. Michael Yohe, Michael Carillon, Lt. Michael Prebonick, and Chief Michael T. Matulavich. The authors also thank the following students who assisted in data cleaning: Natalie Bonfine, Sue Drexel, Marcee Jones, Ashley Kilmer, Kris Kodzev, Marnie Salupo Rodriguez, Dana Sohmer, and Joyce Wall.