Outpatient commitment is a civil court procedure mandating adherence to outpatient mental health treatment in an attempt to prevent relapse, hospital readmission, homelessness, and incarceration. Forty-two states and the District of Columbia have explicit outpatient commitment statutes. All but a few of these laws use the more stringent criteria for involuntary hospitalization as the standard for outpatient commitment (
1,
2,
3,
4,
5,
6,
7). Statutorily defined outpatient commitment typically requires compliance with recommended outpatient treatment but stops short of permitting forced medication of legally competent individuals. When a person under outpatient commitment fails to comply with treatment, outpatient commitment statutes typically permit the responsible clinician to request that law enforcement officers transport the individual to an outpatient facility, where clinicians will attempt to persuade him or her to accept treatment or undertake an evaluation for inpatient commitment (
2).
In addition to statutorily defined outpatient commitment, a number of related civil judicial mechanisms may be used to compel outpatient treatment, including conditional hospital release under involuntary hospitalization, treatment under guardianship, or judicial treatment directives during inpatient commitment proceedings. Under conditional release from a hospital, an involuntarily committed patient is released to community care under the ongoing supervision of a hospital, with the threat of return to the hospital to avert relapse (
8). For an incompetent patient under guardianship, a court-appointed guardian may consent to compulsory outpatient treatment (
9).
Even in the eight states without an explicit outpatient commitment statute, judges may mandate outpatient treatment and order consumers to comply with outpatient treatment during inpatient commitment proceedings. As a result, outpatient commitment may be viewed as a subset of a broader set of civil legal procedures that include both statutorily explicit and permissive forms of compulsory outpatient treatment. In this study, we examined the self-reported frequency of outpatient commitment or functionally similar civil court-ordered treatment.
Monahan and colleagues (
10) reported that among persons in treatment for mental illness in five U.S. cities, 12 to 20 percent had experienced some form of outpatient commitment or related court order. A much larger proportion—44 to 59 percent—had experienced at least some form of "leveraged" outpatient treatment, defined as including outpatient commitment or a related civil court order, criminal justice system mandates, and social welfare system leverage, such as the use of representative payees or subsidized housing to induce treatment adherence. The findings reported in this paper build on those of Monahan and colleagues (
10) by showing a specific association between demographic and clinical variables and receipt of outpatient commitment or related civil court orders.
Our conceptual approach assumes that no single variable "explains" who receives outpatient commitment or related civil court orders. Rather, we understand that behaviors leading to a court order occur within a social-ecological system. We assessed risk of being committed as a set of conditional probabilities across a matrix of domains, including dispositional factors, such as demographic and social environmental characteristics; clinical factors, such as current symptoms, impairment, and functioning; and treatment factors, such as service utilization and contact with institutions. In our analyses, variables from each domain had the potential to contribute, independently or in combination, to the risk of receiving an outpatient commitment or related civil court order. Within this multivariate framework, however, we focused most specifically on clinical factors and their relationship to treatment utilization. We hypothesized that individuals who reported outpatient commitment or related civil court treatment orders would evidence poor clinical functioning in combination with multiple indicators of extensive and problematic service system encounters.
Methods
Consumer sample
A total of 1,011 adult outpatients were recruited from sites that provide public psychiatric services in five cities across the United States, including Chicago; Durham, North Carolina; San Francisco; Tampa; and Worcester, Massachusetts. The methods used in the study are described in detail by Monahan and colleagues (
10). Recruitment criteria specified that participants had to be aged 18 to 65 years, English or Spanish speaking, and in treatment during the past six months for a mental disorder, excluding those with only a substance use disorder.
Because of the different requirements of local institutional review boards, recruitment methods differed somewhat across study sites. At the Worcester, Tampa, and San Francisco sites, consumers were recruited sequentially in the waiting rooms of outpatient clinics of community mental health centers. In Durham, data from the health clinic's management information system were used to randomly select consumers to be approached. At the Chicago site, half the sample was obtained by using the waiting room approach and the remaining half was obtained by using the eligibility list approach with data from the mental health clinic's management information system. Refusal rates varied from 2 to 13 percent across sites.
After receiving a complete description of the study, participants provided written informed consent and were enrolled. Consumers were interviewed in person by trained interviewers and were paid $25 for an interview. Interviews lasted on average 90 minutes.
Across the five sites, the mean age of the study participants ranged from 41 to 47 years, the percentage of male participants ranged from 32 to 65, the percentage of Caucasian participants varied from 35 to 69, and the percentage of chart diagnoses of schizophrenia, bipolar disorder, and major depression varied from 42 to 50, from 14 to 18, and from 28 to 31, respectively. Diagnoses of anxiety spectrum disorders and other disorders ranged from 2 to 8 and 2 to 6 percent, respectively.
Measures
Legal bases for the use of civil court-ordered treatment. Each of the five jurisdictions in this study has a somewhat different legal base for civil court-ordered outpatient treatment, and none forbade outpatient treatment mandates. North Carolina has explicit outpatient commitment criteria that are less stringent than those for inpatient commitment. Illinois does not have separate outpatient commitment criteria, but the court is directed to order the "least restrictive alternative for treatment which is appropriate" for an individual found to meet statutory criteria for involuntary hospitalization, "including but not limited to hospitalization" (
11). Massachusetts does not have a statutory base for civil court-mandated outpatient treatment. However, at least in western Massachusetts, a de facto system of judicially ordered care has been created through use of the state's guardianship law (
9).
At the time of this study, Florida law provided that a court considering involuntary inpatient placement could do so only after finding that "all available less restrictive treatment alternatives which would offer an opportunity for improvement of his or her condition have been judged to be inappropriate" (
12). However, courts lacked the authority to rehospitalize a person who had been noncompliant with an order for care in the community without a new petition and hearing for involuntary placement (
13). California permitted a person who had been civilly committed to be placed on outpatient treatment status if certain conditions were met, including the availability of appropriate treatment (
14). Since collection of the data reported here, both California and Florida have enacted some form of outpatient commitment. At the time of data collection, all five states had statutes that either explicitly or implicitly permitted some form of civil judicially mandated outpatient treatment.
Persons' lifetime experience with leverage. We assessed individuals' lifetime experiences of four tools to leverage treatment adherence: use of representative payeeship and housing supports contingent on treatment adherence, criminal court sanctions requiring treatment, and civil court-based orders such as outpatient commitment. Individuals were asked whether a judge had ever ordered outpatient commitment for them and ordered them to accept outpatient treatment for a mental health or substance use problem. Interviewers were instructed to help consumers distinguish between treatment mandates under criminal sanctions and outpatient commitment in the context of civil court proceedings. No court records were reviewed; reports of legal and other leverage experiences are based entirely on self-report.
Social support and treatment assistance. We used items from the Duke Social Support Scale (
15) to assess subjective social support. To assess assistance with treatment, participants were also asked whether they had someone who routinely helped them adhere to mental health treatment during the past six months.
Clinical characteristics. Objective diagnostic information was obtained by chart review. In addition, the anchored version of the Brief Psychiatric Rating Scale (
16) and the Global Assessment of Functioning (
17) were used to assess current psychiatric symptoms and functioning, respectively. Insight into mental illness was assessed with the Insight and Treatment Attitudes Questionnaire (
18). Consumers were asked about their alcohol and drug use during the past 30 days by using the adapted Michigan Alcoholism Screening Test (
19) and the Drug Abuse Screening Test (
20). Finally, participants were asked detailed questions about service use and hospitalization.
Other measures. Treatment compliance was assessed by self-rated attendance at scheduled mental health appointments in the past six months on a 5-point Likert scale from "never missed an appointment" to "avoided keeping appointments altogether." Medication compliance was assessed on a similar 6-point scale. The Drug Attitude Inventory (
21) was used to assess participants' attitudes toward taking psychotropic medications. Treatment satisfaction was assessed with use of an adapted version of the Mental Health Statistics Improvement Program Consumer Survey (
22). Perceived coercion was measured with the MacArthur Perceived Coercion Scale (
23), adapted for reference to outpatient treatment. We used a set of six Likert-scaled items to assess participants' experience of personal autonomy in everyday life. Examples include "How much say did you have about what you would do during the day?" "How much say did you have about how much of your money you could spend?" and "How much say did you have about who you would spend time with during the day?" Self-report of any specific violent behavior directed at another person in the past six months was assessed with the MacArthur Community Violence Interview (
24).
Interviewers at each site were trained in the reliable administration of the structured interview. Training techniques included observation and parallel coding of interviews as well as ratings of standard videotaped interviews. The proportion of agreement between interviewers and an experienced psychiatrist for total scores on the BPRS was 91 percent across the five sites.
Statistical analysis. We first examined bivariate associations between outpatient commitment or related civil court orders and a range of salient variables. Continuous variables were recoded into high and low categories (above and below the median) to better capture nonlinear associations and to allow a common, efficient test of whether the five sites differed in the relationship of each characteristic to the receipt of court orders.
Specifically, we used Zelen's test of the homogeneity of odds ratios (
25) to accept or reject the null hypothesis that the relative risk for judicial orders across sites did not differ but represented a sampling distribution from a common population. If Zelen's test showed that the sites' odds ratios for a given variable were homogeneous, we used logistic regression procedures to calculate a common odds ratio across sites, with a confidence interval and p value corrected for the clustered nature of the data.
Results
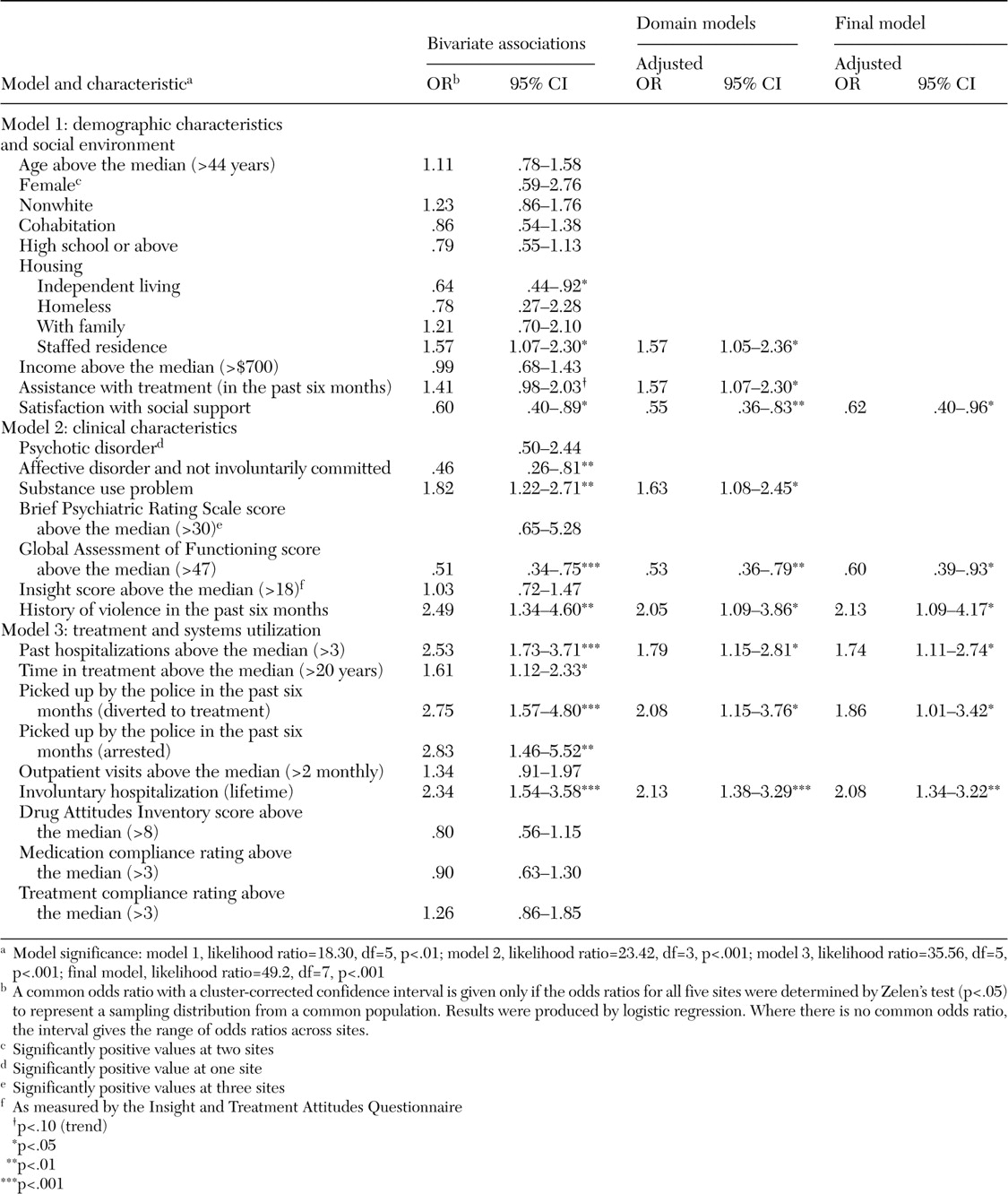
The bivariate associations between reported civil court-ordered treatment and a range of demographic and clinical characteristics are presented in
Table 1. Following our conceptual model, we grouped the independent variables into three content domains: demographic characteristics and social environment; clinical characteristics; and treatment and systems utilization. Bivariate relationships between individual predictors and civil court-ordered care are presented in the common odds ratios shown in the first column of
Table 1. Significance tests are presented only for instances in which Zelen's test confirmed the homogeneity of odds ratios across study sites. Otherwise, as noted, the table presents the range of odds ratios across sites. The second column in
Table 1 displays adjusted common odds ratios for the variables within each domain, resulting from site-controlled multivariate logistic regression analysis (
26). As with the bivariate analyses, all the variables included in these multivariate domain models were first shown by Zelen's test to be homogeneous in relation to outpatient commitment or related orders across the five sites. Each domain model—models 1, 2, and 3—was initially tested independently, and then significant predictors from each domain were entered into a final model.
Model 1 examines the individual bivariate relationships within this set of predictors and demonstrates that a history of civil court-ordered treatment was significantly more common among individuals who were living in staffed residential programs (and conversely not living independently) and those who reported low social support from family and friends. These analyses also demonstrate a trend toward outpatient commitment or civil court orders among those who received assistance to comply with treatment. When these predictors were examined together in a multivariate model, these significant relationships persisted and the relationship with assistance was significant.
Model 2 examines the bivariate relationships within this domain and demonstrates that these orders were less common among individuals with affective disorders who had never been involuntarily hospitalized and were also more common among participants with comorbid substance use problems, greater functional impairment, and a history of violent behavior. When examined together in a multivariate domain model, these significant relationships persisted, except for the relationship with individuals with affective disorders who had never been involuntarily hospitalized, which was nonsignificant.
Model 3 shows that court-ordered community care was more common among participants with a history of multiple hospitalizations, more years in treatment, recent police intervention during a mental health crisis, recent arrests, and a history of involuntary hospitalization. When examined together in a multivariate model, these significant relationships persisted, except for the relationships with years in treatment and recent arrests, which were nonsignificant.
As shown in
Table 1, all significant variables from the domain models were included in the final logistic regression model, which controlled for site differences. In this final model, participants who reported lower levels of social support, lower levels of psychosocial functioning, recent violent behavior, more frequent hospitalizations, recent police involvement during mental health crises, and a history of involuntary hospitalization were significantly more likely to report that a court had ordered them to comply with community treatment.
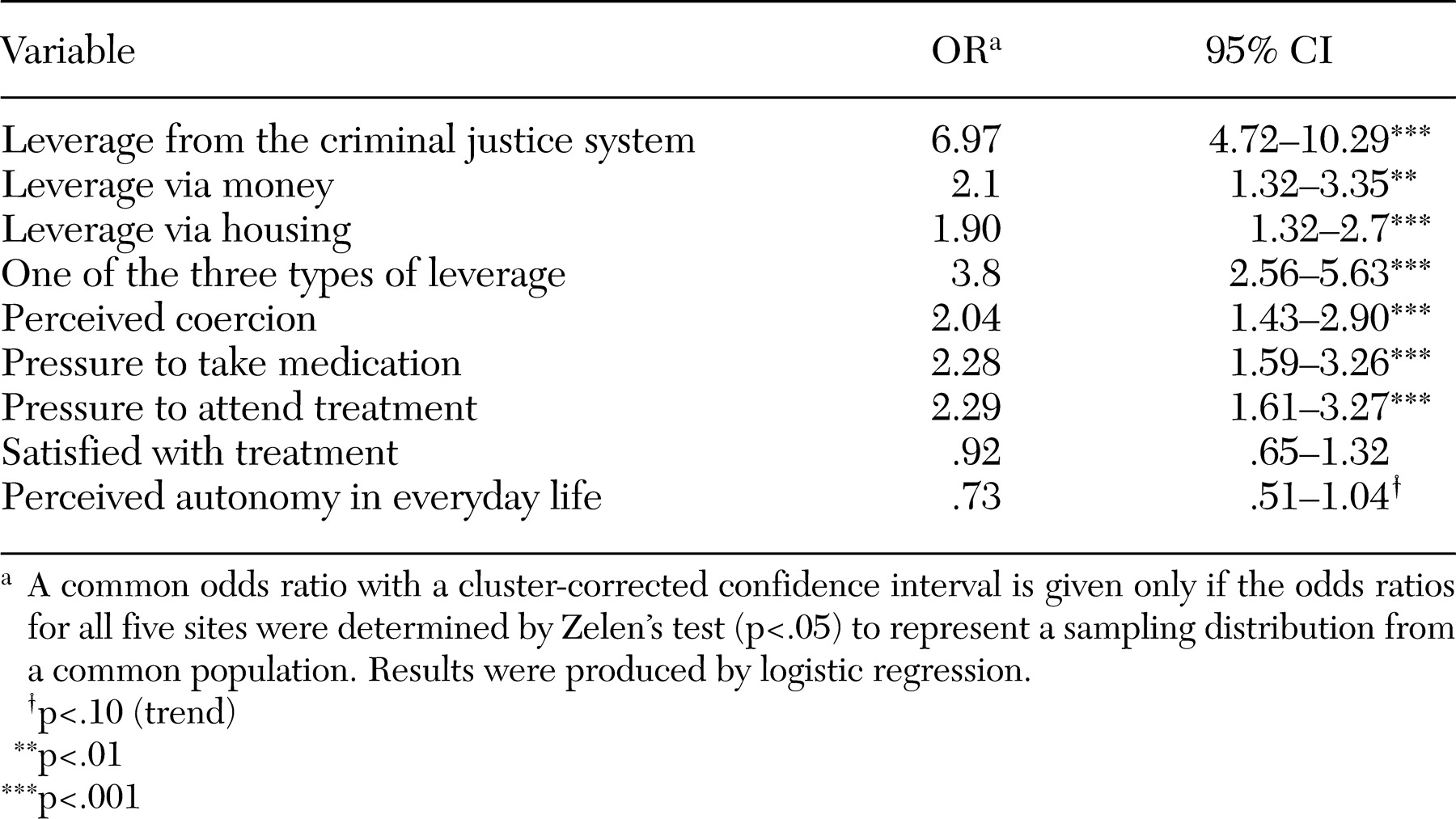
Bivariate relationships between outpatient commitment or civil court-ordered treatment and other leverage experiences are presented in
Table 2. Persons with a history of civil court treatment were more likely to have also experienced criminal justice sanctions in which a judge directed the consumer to seek treatment. In addition, persons reporting a history of outpatient commitment or related orders were more likely to have been directed to participate in treatment as a condition of receiving their money from a representative payee or other third-party money manager and were more likely to have lived in subsidized housing in which mental health treatment was required. Persons reporting a history of civil treatment mandates also reported more pressures from treatment personnel and family to adhere to prescribed medications and treatment and also reported more perceived coercion to attend treatment. In these bivariate relationships, a history of outpatient commitment or similar civil court-ordered treatment was not significantly associated with satisfaction with mental health treatment or perceived sense of autonomy in everyday affairs.
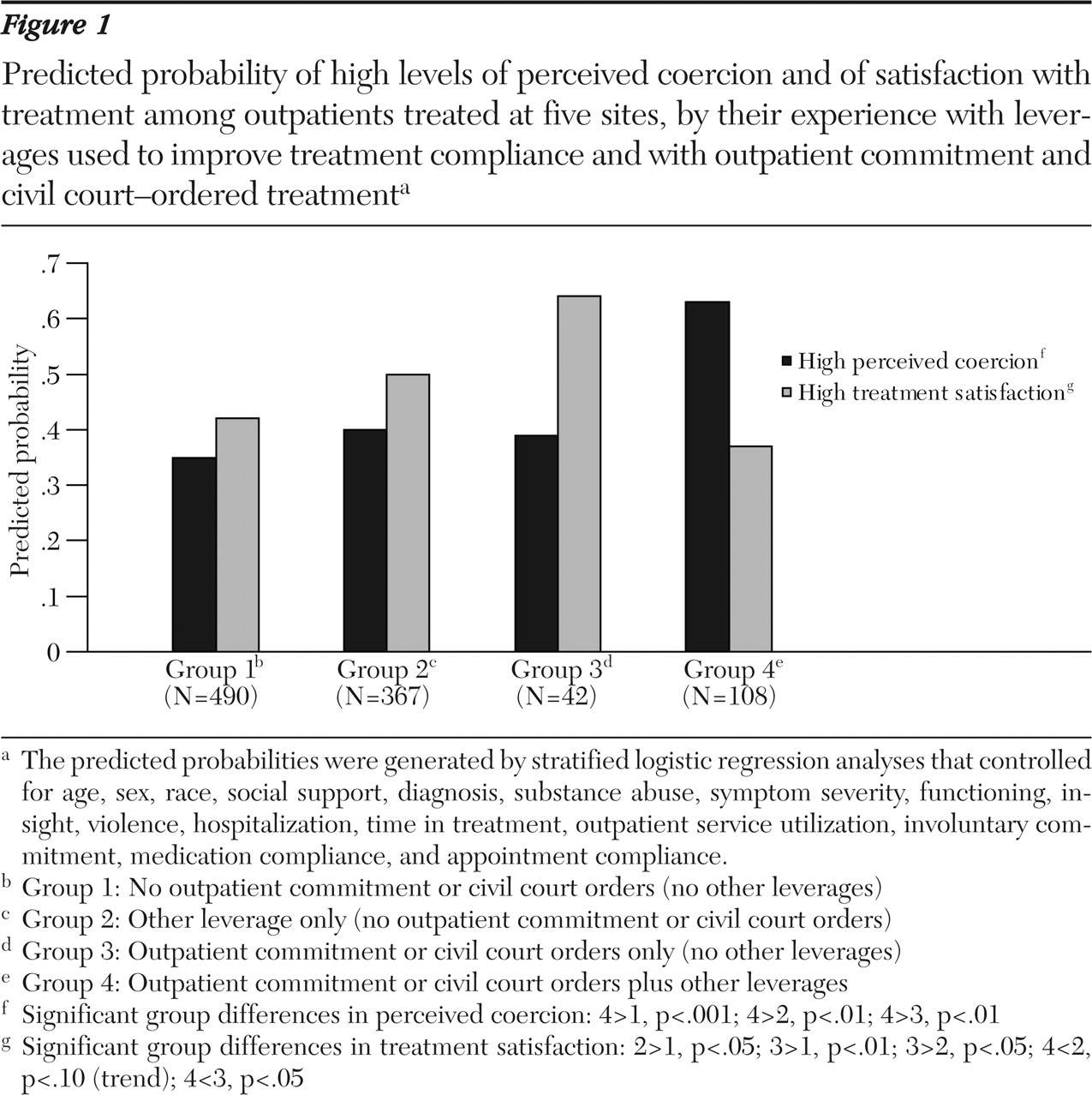
We next examined the relationship between lifetime outpatient commitment or civil court treatment mandates in combination with other leverage experiences and current perceptions of coercion in treatment and treatment satisfaction.
Figure 1 depicts the predicted probabilities of perceived coercion and treatment satisfaction estimated by using multiple logistic regression analyses (
26), which estimated the probability of experiencing high perceived coercion or high treatment satisfaction after relevant covariates were controlled for.
Figure 1 contrasts levels of perceived coercion and treatment satisfaction for four groups: individuals with no history of outpatient commitment or civil court mandates or other leverage attempts (group 1), those with leverage attempts other than outpatient commitment or related civil court orders (group 2), those with outpatient commitment or related orders only (group 3), and those with outpatient commitment or related orders plus other leverage attempts (group 4). These results show that individuals who had experienced multiple leverages—outpatient commitment or similar orders in combination with other leverages—were significantly more likely to perceive a high degree of coercion in mental health treatment and to report poor satisfaction with treatment. In contrast, participants who had experienced outpatient commitment or related orders alone (with no other types of leverages) were significantly less likely to report feeling coerced and more likely to report that they were satisfied with their mental health treatment. This group with outpatient commitment or related orders alone was represented fairly evenly across sites and was demographically similar to consumers with multiple leverages. As might be expected, these individuals were significantly less likely to have had frequent hospitalizations and episodes of violence and were less symptomatic.
Discussion and conclusions
Between 12 and 20 percent of persons in treatment for mental illness in five U.S. communities reported lifetime rates of outpatient commitment or equivalent civil court-ordered treatment, and nearly three-quarters reported experiencing other kinds of leverage applied through the legal or social welfare system to improve their treatment adherence. Reports of experience with such orders were significantly more likely among participants with poor social support, poor psychosocial functioning, a recent history of violent behavior, multiple lifetime hospitalizations, a history of involuntary commitment, and recent police encounters in mental health crises. These orders were also more common among persons living in residential settings who received assistance with treatment and had co-occurring substance use problems, although in the final multivariate models these correlates were not significant.
Overall, the group "at risk" of civil court mandates clearly demonstrated complex ongoing difficulties in everyday functioning, with frequent problematic behavior leading to involvement with law enforcement and involuntary hospitalizations. However, our cross-sectional results are also consistent with a view that individuals under outpatient commitment or other civil court-ordered treatment were subjected to closer social control and more likely to receive other sanctions because they were under closer surveillance.
Interestingly, few persons (N=42) had experienced outpatient commitment or related civil court orders alone. More commonly, persons who had received outpatient commitment or related civil court orders had also experienced one or more other forms of leverage, and these consumers reported higher coercion and lower treatment satisfaction than those without multiple mandates. The small group who reported outpatient commitment or related court orders alone reported low perceived coercion and high treatment satisfaction, perhaps because their singular experiences with civil court treatment orders alone, without other types of leverage, identifies a group with a more benign course and a successful return to treatment adherence. Those with multiple leverage attempts likely had a more tumultuous course in which multiple agencies and actors attempted to ensure treatment adherence.
The study found similar rates of outpatient commitment or related civil court orders across the five sites, which included two states with explicit outpatient commitment statutes—North Carolina and Illinois—and three states that allow other civil court orders functionally similar to outpatient commitment—Florida, Massachusetts, and California. North Carolina, with an explicit statute, had the highest rate of outpatient commitment. It is possible that some consumers confused treatment mandates received from judges in commitment proceedings with criminal court mandates, inflating the outpatient commitment or other civil court-ordered treatment estimates. However, more than 80 percent of consumers who reported outpatient commitment also reported involuntary hospitalizations, during which outpatient civil court orders are often imposed. Self-reported lifetime rates of outpatient commitment or related orders may be affected by poor recall of respondents—and perhaps underestimated—but there is no reason to suspect that these findings are less reliable than other results that rely on self-report measures.
It is also possible that these findings may not generalize to other populations. Geographically and demographically diverse study sites were chosen to be broadly representative of the U.S. treatment system, but the sites were not randomly selected. In addition, because of constraints imposed by institutional review boards across sites, recruitment approaches differed, and therefore the samples may differ across sites. Because all participants were in treatment, these results may not accurately represent the views and experiences of individuals who are not in treatment. For example, persons from minority groups are less likely to receive needed mental health services and thus were probably underrepresented in this study. They are more likely to be treated in psychiatric hospitals and crisis settings and are more mistrustful of providers than persons who are not from minority groups (
27). As a result, the views of the consumers in treatment in this sample may be an underestimate of the extent to which consumers not in treatment feel coerced or dissatisfied with treatment under outpatient commitment or related civil court orders.
Although rates of use of outpatient commitment and civil court orders may differ across sites, we found strong consistency in the demographic and clinical correlates of outpatient commitment or related civil court orders across sites, suggesting that explicit and permissive statutory forms of mandated community treatment are applied to populations with a similar profile across diverse treatment systems. It is also interesting that in another study, conducted in Florida, in which respondents were asked whether they experienced the leverages explored in more detail in the MacArthur prevalence study (
10), 10.4 percent of 300 individuals enrolled in a study of Medicaid and 16.8 percent of 113 individuals enrolled in a study of the Broward County Mental Health Court, reported that they had experience with outpatient commitment (
28). These reports suggest that regardless of statutory law, a percentage of individuals who receive care have experience with some form of judicial order designed to improve treatment adherence.
Finally, a history of civil court-ordered outpatient treatment was most common among persons with mental illness who came into contact with multiple mental health, social welfare, and criminal justice agencies, many of which apply forms of leveraged treatment in attempts to improve adherence. Further research is needed to guide policy makers in implementing coordinated and effective responses to treatment nonadherence.
Acknowledgments
This work was supported by the John D. and Catherine T. MacArthur Foundation Research Network on Mandated Community Treatment and by grant K02-MH67864 to Dr. Swanson.