Religiosity is a widespread and important influence on human behavior and well-being. In a recent national poll, 95 percent of Americans professed a belief in God, and 67 to 75 percent of respondents reported that they pray on a daily basis (
1). Thus it is likely that religiosity has an impact on the experience of caregiving. Indeed, multiple lines of research have found that people caring for an ill family member turn to religion for support. Studies have found that caregivers of patients with Alzheimer's disease (
2,
3), those caring for elderly persons with disabilities (
4), and spouses of patients with lung cancer (
5) frequently use religion to cope with caregiving demands.
Research that has examined the outcomes of religious coping has generally found that religiosity among caregivers is linked to enhanced adjustment. For example, in a longitudinal study of 62 caregivers of persons with Alzheimer's disease or cancer, Rabins and colleagues (
6) found that strength of religious belief at baseline was associated with better emotional adjustment among caregivers at two-year follow-up, even when personality variables, family functioning, and levels of anger and guilt were controlled for. In another study of 127 caregivers of elderly persons with disabilities, Chang and colleagues (
4) found that caregivers who used religious or spiritual beliefs to cope with caregiving stresses had a better relationship with care recipients, lower levels of depression, and better self-care—for example, less "submersion" in the caregiving role.
Although previous research underscores the important role of religiosity among caregivers, little attention has been devoted to family caregivers of persons with serious mental illness. Only one published study has quantitatively assessed and examined the correlates of religiosity among such family members (
7). In that study, 60 Hindu family members of patients with schizophrenia were recruited through a public hospital in India. These individuals completed measures of their caregiving burden, coping activities, religious beliefs and practices, and adjustment. The results of the study highlight the prevalence of religious coping—90 percent of participants reported praying to God, and 50 percent viewed religion as a source of solace, strength, and guidance in coping with caregiving demands. In multiple regression analyses, the authors found that strength of religious belief was linked to greater well-being among caregivers, with other types of coping and demographic characteristics controlled for. Although the generalizability of these results is limited by cultural context, these findings highlight the prevalence and potential benefits of religiosity among caregivers of persons with serious mental illness.
Naturalistic interview studies concur. Johnson (
8) interviewed a sample of 180 family members about their understanding of their relative's illness, sources of support, and ways of coping and found that family members often turn to religion to cope with the stress of caring for an ill family member. Summarizing these findings, Johnson observed, "Family members who felt supported by a religious community, by their own sense of faith, or by other family members were much more positive in their outlook." Bland and Darlington (
9) echoed these results in their study of hope among family members of persons with serious mental illness. Five of the 16 participants spontaneously identified religious beliefs and participation as a significant source of hope.
Thus previous research points to the important role of religiosity among family caregivers of persons with serious mental illness. Moreover, these preliminary studies, along with work in other caregiving populations, suggests that religiosity may have salutary effects on caregiver adjustment. The study reported here examined religiosity, dimensions of adjustment, self-care, and caregiving burden in a sample of participants in the National Alliance on Mental Illness (NAMI) Family to Family Education program. The aims of the study were to characterize the nature of religiosity and sources of spiritual support in a sample of family caregivers of persons with serious mental illness and to test hypotheses that religiosity would be associated with greater mastery, self-esteem, and self-care and less depression, worry, and displeasure.
Methods
Participants and procedures
The study used data from a larger study of the effectiveness of the Family to Family Education program. Further details about the sample and the larger study evaluating the Family to Family program are provided elsewhere (
10). Eighty-five participants in Family to Family courses that were offered between February and November 2000 completed baseline interviews that assessed religiosity and adjustment variables. Because data on key variables were missing for two participants, 83 participants were included in the analyses.
The mean±SD age of participants was 52.2±12.9 years. Sixty participants (72 percent) were women, and 23 participants (27 percent) were men; 61 participants (73 percent) were white, 16 (19 percent) were African American, three (4 percent) were Asian, two (3 percent) were Hispanic, and one (1 percent) was of another ethnic background.
Family members were deeply involved in caregiving for relatives—76 (92 percent) reported that they were "very" or "somewhat" involved. Forty participants (44 percent) reported having a relative with schizophrenia, 46 (50 percent) had a relative with a major affective disorder, and the remaining six (6 percent) had a relative with another diagnosis. Fifty-six participants (60 percent) were parents of the ill relative, 14 (15 percent) were siblings, seven (8 percent) were spouses, seven (8 percent) were children, nine (9 percent) were another type of family member, and one (1 percent) was a friend who was not related.
Written informed consent was obtained from all study participants in full accordance with the standards of the University of Maryland's institutional review board.
Assessments
Religiosity. In addition to background questions that assessed religious affiliation for descriptive purposes, religiosity was measured with three items. One question assessed the importance of religious and spiritual beliefs on a scale ranging from 1, not important at all, to 4, very important. Frequency of attendance at religious services was assessed on a scale ranging from 1, never, to 8, nearly every day. A third question assessed the degree to which participants believed that God was a source of strength and comfort, measured on a scale from 1, not at all, to 4, a great deal.
Receipt of spiritual support. To collect descriptive data on specific types of spiritual support received in coping with the mental illness of a family member, we asked participants, "Have you received any religious or spiritual support in dealing with [the patient's] illness in the past three months?" If the response was yes, the participant was then asked the frequency with which he or she practiced the following activities in coping with the relative's illness: praying or meditating, watching or listening to religious programs on television or the radio, seeking spiritual direction on the Internet, reading the Bible or other religious literature, and seeking support from clergy or from other members of the individual's spiritual community.
Depression, mastery, and self-esteem. We used modified versions of the Center for Epidemiologic Studies Depression Scale (CES-D) to assess depression (
11) and self-esteem and mastery scales (from the Family Impact Survey) developed by Pearlin (
12). The depression scale comprises 14 items assessing the extent to which respondents experienced depressive symptoms during the previous week, with lower scores indicating less depression. The self-esteem scale is made up of ten items assessing positive and negative self-feelings. Respondents rate the items on a scale of 1 to 4, with higher scores indicating greater self-esteem. The mastery scale is a 7-item scale with two items measuring sense of mastery and five items tapping pessimism or lack of control. Respondents rated the items on a scale of 1 to 4, with higher scores indicating a greater sense of mastery.
Subjective caregiving burden: worry and displeasure. Worry and displeasure were assessed with modules from the Family Experience Interview Schedule (
13), which has well-established reliability and validity. The worry subscale consists of seven items that assess respondents' level of concern about different aspects of their ill relative's life. All items are rated on a scale of 0 to 7, with lower scores indicating less worry. The displeasure subscale has seven items that measure emotional distress or displeasure on a scale of 1 to 4, with lower scores indicating less displeasure.
Self-care. Self-care refers to the degree to which family members engage in positive and supportive activities that help lessen their distress in coping with their relative's illness. This variable was measured with a six-item self-care measure created by Joyce Burland, Ph.D., creator of the Family to Family program, and which has been used in evaluations of the program. One example item is "I take time for myself to take care of myself and do things I enjoy." This face-valid scale displayed high internal consistency in our study sample (alpha=.87).
Analysis
Bivariate correlations were calculated with the Pearson r product-moment correlation coefficient to explore intercorrelations between the religiosity items. Personal importance of religion was highly correlated with finding comfort and strength from God (r=.83, p<.001). These two variables were therefore combined in subsequent analyses to form a composite of "personal religiosity." Because attendance at services was correlated only moderately with both importance of religiosity (r=.48, p<.001) and finding comfort and strength from God (r=.49, p<.001), and is also conceptually distinct from personal religiosity, this variable was kept separate for subsequent analyses. Previous work also supports this distinction between service attendance and personal religiosity, on both conceptual and empirical grounds (
14). In subsequent analyses, the two dimensions of religiosity were labeled personal religiosity and service attendance.
We next examined relationships between sociodemographic characteristics—gender, age, race, and education—and the religiosity and criterion variables used in the study. Level of education was negatively associated with personal religiosity (r=-.22, p=.04), and a statistical trend indicated that participants who were not white reported higher personal religiosity than white participants (F=3.66, df=1, 81, p=.059). Age was negatively associated with mastery (r=-.28, p=.009), and education was positively associated with self-esteem (r=.30; p=.005).
To test our primary hypotheses, we ran hierarchical multiple regression models with each of the adjustment variables as the dependent variable. In the first step, we entered age, gender, education, and race. In the second step, we entered the two religiosity variables. An alpha level of .05 was used to determine statistical significance for all analyses.
Results
Descriptive results on religiosity and spiritual support
The religious affiliations of participants were as follows: 35 (42 percent) were Protestant, 27 (32 percent) were Catholic, eight (9 percent) were Jewish, ten (13 percent) identified an "other" religious preference, and three (4 percent) reported no religious affiliation. Religious affiliation was not related to any of the criterion variables. Thirty participants (36 percent) reported that they attended religious services at least once a week, and 26 participants (31 percent) reported attending services at least once a month. These rates of service attendance are comparable with those found in national Gallup polls, which indicate that 40 percent of the U.S. population regularly attends religious services (
1). The mean rating of importance of religion and spirituality, on a scale of 1 to 4, was 3.43±.83—halfway between "fairly important and "very important." The mean rating of whether participants considered God to be a source of comfort and strength, on a scale of 1 to 4, was 3.26±1.03, falling between "quite a bit" and "a great deal." Overall, this was a moderately religious and spiritual sample, comparable to the general population on service attendance and personal religiosity.
Thirty-one participants (37 percent) reported that they had received religious or spiritual support in coping with their relative's illness in the past three months. The most frequent types of spiritual support were praying or meditating, reading the Bible or other religious literature, and watching or listening to religious programs on television or the radio. Notably, 19 participants (23 percent) reported that they contacted clergy or a religious leader to talk about problems or concerns related to their relative's illness, with seven (8 percent) reporting that they did this "very often or fairly often." Twenty-three participants (28 percent) reported relying on members of their congregation for support in coping with their relatives' illness during the previous three months.
Depression, self-esteem, mastery, self-care, and subjective burden
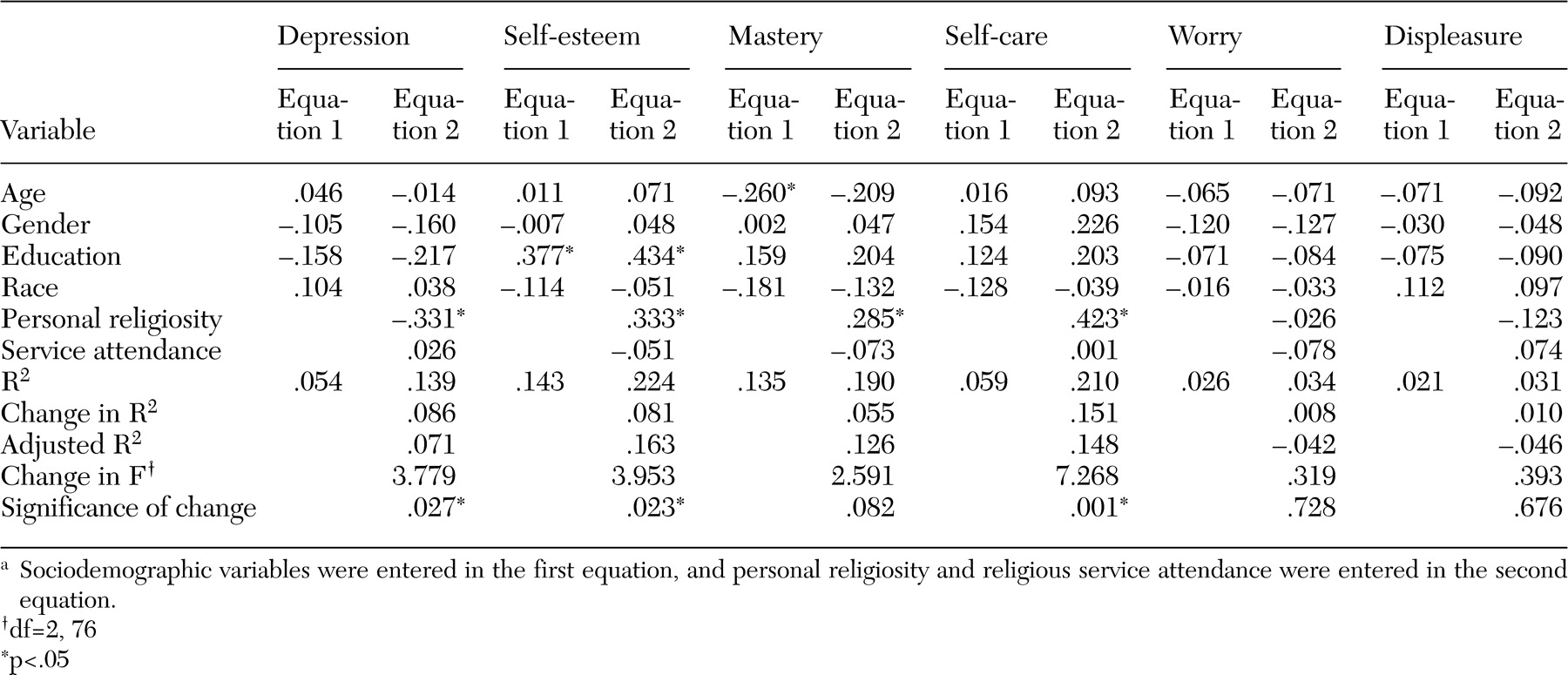
Bivariate Pearson product-moment correlations indicated that personal religiosity was positively associated with level of mastery (r=.26, p=.017) and self-care (r=.33, p=.003) and negatively associated with level of depression (r=-.25; p=.025). Results of the regression analyses are reported in
Table 1. Sociodemographic variables were entered in the first equation. Personal religiosity and service attendance were entered in the second equation, with the significance of the change in R
2 as the statistical test of each hypothesis. Religiosity was incrementally associated with caregivers' level of depression, self-esteem, and self-care. However, religiosity was not significantly associated with unique variance in mastery, worry, or displeasure. As indicated by the strength of the regression coefficients in
Table 1, personal religiosity was a stronger predictor of family member adjustment than service attendance.
Discussion
The major findings of this study are twofold. First, we found that a substantial proportion of family members of persons with serious mental illness mobilize religious and spiritual resources to cope with their situation as caregivers. Second, consistent with our hypotheses, we found that religiosity was associated with greater self-esteem and self-care and less depression among family caregivers. However, religiosity was unrelated to subjective burden, and correlations with mastery were equivocal. Most broadly, this pattern suggests that religiosity may bolster the internal coping resources of family members who are caring for people with serious mental illness.
Our finding that religiosity is associated with enhanced self-esteem is consistent with previous research that indicated positive associations between personal religiosity and self-esteem in medical and community samples (
14). However, ours is the first study to establish such a link in a sample of caregivers of persons with serious mental illness. Religiosity may enhance self-esteem through fostering personal belief in an intrinsic spiritual worth—for example, "God cares for me and accepts me"—a common belief within the Judeo-Christian tradition and in other world religions. Religiosity may also provide opportunities to enhance self-esteem through participation in the activities of a faith community and its shared traditions or through positive regard received from others in that community.
Our findings on depression are consistent with previous research, which has found religiosity to be associated with reduced risk of depression in community samples (
15), persons with medical illness (
16), and caregivers (
7). The strongest relationship observed in our data was the link between religiosity and self-care. This finding suggests that there is a pathway whereby religiosity may contribute to enhanced well-being among caregivers, by expanding the capacity or motivation for self-care. However, it is also possible that the two are linked by some third variable that affects both. On the whole, our results are consistent with those of Rammohan and colleagues (
7), who found that strength of religious belief was associated with greater well-being among family members. Although religious variables were associated with better self-care and adjustment, it is noteworthy that religiosity did not diminish the amount of worry or displeasure that family members felt about their ill relative.
This study had several limitations that point to directions for future research. First, the generalizability of these findings is limited by the fact that we used a self-selected sample of family members who completed the Family to Family program. Second, for brevity we used relatively broad measures of religiosity. Although our findings begin to elucidate links between religiosity and caregiver well-being, a more nuanced assessment of the multidimensional construct of religiosity or spirituality is needed. For example, future studies could use more detailed assessments of religious coping strategies (
17) to determine pathways by which religiosity contributes to outcomes. Moreover, religiosity is not a homogeneous construct—it may vary considerably between various cultural and ethnic groups. Third, these data are cross-sectional, which limits any possible causal conclusions about the observed relationships. For example, it is possible that persons with higher self-esteem and less depression are more likely to be religious, or that the variables have some pattern of reciprocal influence on each other. Also, a third variable that was not measured or considered—for example, personality factors—could be responsible for the observed relationships.
A prospective cohort study that measured changes in religiosity and adjustment over time would help to clarify the directionality of these associations and would inform the development of a theoretical model as to how religiosity may relate to caregiver adjustment over time. More research is also needed on the role of religion and spirituality in the lives of patients with serious mental illness themselves. Initial studies indicate that a large percentage of patients use religion to cope with their illness (
18) and believe that spirituality is a positive influence in their recovery (
19). However, we have limited scientific knowledge about the specific ways in which patients use religion for support and the relationship between religious coping and recovery outcomes.
More than a third of the participants in this study reported that they had received spiritual support related to their relative's illness in the previous three months. Future studies and applied work should consider religious organizations as a community-based source of support that is used by persons with mental illness and their family caregivers. A recent survey of faith-based organizations in the Los Angeles area highlighted a high demand for mental health services in religious and spiritual communities but also identified significant barriers to the implementation of such services—for example, limited expertise and resources. In reporting these results, Dosset and colleagues (
20) emphasized that partnerships between mental health providers and faith-based communities may be a particularly effective strategy for meeting the mental health service needs of populations that are underserved by the mental health system, such as persons with low incomes, ethnically diverse communities, and recent immigrants. In one attempt to embed caregiver services within a religious congregation, Pickett-Schenk (
21) conducted a church-based support program for African-American families coping with the mental illness of a family member. In a study of 23 caregivers, participants reported that they were highly satisfied with the group and perceived gains in knowledge and morale. In another vein, NAMI provides support to faith-based communities that are attempting to address the needs of persons with serious mental illness through projects such as the Faith Communities Education Project and FaithNet (
22).
It is also critical for mental health professionals to appreciate the important role of religion and spirituality among persons with mental illness and their caregivers. Clinical interventions should include routine assessment of this important area, and interventions should be appropriately tailored to build on relevant religious and spiritual resources, while respecting the diversity of background and beliefs. It is also important for mental health professionals to effectively collaborate with clergy and other religious professionals in providing services to persons with serious mental illness and their caregivers.
Conclusions
Taken together, our findings indicate that family members often turn to spirituality for support and that religiosity may be an important part of how caregivers adapt to the fact that a family member has a serious mental illness. In particular, our data indicate that religiosity is negatively associated with symptoms of depression and is also related to how caregiving family members feel about and care for themselves. Collaborative partnerships between mental health professionals and religious and spiritual communities represent a powerful and culturally sensitive resource for meeting the needs of family caregivers of persons with serious mental illness.