The role of psychodynamic psychotherapy in psychiatric education and practice is evolving. In popular media, patients receiving this treatment are sometimes stigmatized as “the worried well.” In contrast, large descriptive surveys of patients receiving psychoanalysis and long-term psychodynamic psychotherapy have found high rates of comorbid psychiatric conditions and a history of failed treatments (
1). It is not known whether psychiatric trainees practicing this modality treat patients with similar challenges.
Training in psychodynamic psychotherapy is required by North American credentialing bodies for postgraduate psychiatry education (
2). Psychodynamic psychotherapy focuses on patients’ emotions, inner subjective experiences, relationships, and problematic behavioral patterns (
3). Beyond the value of learning this modality itself, this training confers skills in the common factors shared by all effective psychotherapies: communicating empathically, forming and maintaining therapeutic alliances, and attending to in-session emotions (
4). Meta-analyses of process research have demonstrated that these therapeutic elements improve outcomes achieved with numerous treatment modalities (
5,
6). Acquiring expertise in psychodynamic psychotherapy during residency also enhances a psychiatrist’s capacity to use biopsychosocial formulations in assessment and treatment planning, to motivate patients to engage in treatment and healthful behaviors, and to ethically manage the complicated dynamics of clinician-patient relationships.
In stepped-care models (
7), more intensive, long-term care is indicated for individuals with chronic, complex mental disorders who remain symptomatic and functionally impaired after less intensive treatments, such as pharmacotherapy and brief structured therapies. Psychodynamic psychotherapy is such a treatment and has empirical support in treating many psychiatric disorders, including chronic depression, anxiety, and personality disorders (
8–
13).
Thus, psychodynamic psychotherapy training teaches widely generalizable skills and a modality that is especially valuable for patients with chronic and comorbid conditions who have not received adequate benefit from less intensive treatments. However, little is known about patients who are treated with psychodynamic psychotherapy by trainees and, in particular, whether these patients are representative of psychiatric patients who require and may benefit from longer-term intensive treatment. In this study, we sought to characterize the diagnoses, histories, and treatment profiles of patients receiving psychodynamic psychotherapy from psychiatry residents in hospital-based outpatient clinical training settings.
Methods
The Department of Psychiatry at the University of Toronto is the largest postgraduate psychiatric residency training program in the world, with about 200 trainees across all years. Resident trainees are required to conduct clinically supervised psychodynamic psychotherapy for two patients during postgraduate years (PGY) 2–5. Patients are primarily drawn from local outpatient hospital clinics, where psychodynamic psychotherapy is recommended for individuals with anxiety, depression, and personality disorders who are able and willing to participate in long-term outpatient treatment at a frequency of at least once weekly for 1 or more years.
During their training, residents are required to present and receive feedback on two case reports, one toward the end of PGY2 and one at the beginning of PGY4, to foster skills in patient-centered biopsychosocial case formulation, reflective and observational capacities, and narrative competence—synthesizing and describing clinical experiences that demonstrate application of principles to practice. Core components of case reports include the patient’s identifying data, reason for accessing treatment, history (psychiatric, forensic, family psychiatric, medical, and personal), developmental experiences (e.g., early childhood adversity that may have contributed to the current problems), psychiatric diagnosis, mental status examination, and major themes that have emerged during therapy. Residents are expected to discuss transference, countertransference, the doctor-patient relationship, and illustrative examples of therapeutic processes. Case reports conclude with a formulation of the resident’s understanding of the patient as a person with difficulties and a provisional synthesis of the various elements manifested by the patient (and evoked in the therapist) to generate etiological hypotheses about the patient's diagnosis and experience of him- or herself and others. Case reports are discussed with each resident’s clinical supervisor, and the resident receives written feedback from another independent supervisor. The data for the current study came from these case reports.
We conducted the study with descriptive methods. We examined 204 case reports of the patients of 184 PGY2 and PGY4 psychiatry residents from 2011 to 2015, extracting demographic information, DSM diagnoses, history, past psychiatric treatments, and other characteristics, including trauma or insecure attachment. DSM-IV-TR was applied to case reports from 2011 to 2013, and DSM-5 for reports from 2013 to 2015. If the resident reported on different patients for the PGY2 and PGY4 case presentations, we included both reports. If both case reports were from the same patient, however, we included only the PGY4 report. Two trained research assistants (T.K. and M.H.) coded the data, and a proportion of the data from the case reports was independently extracted and coded by both to ensure reliability. When there was uncertainty or disagreement regarding coding, the case report was read and coded by a senior psychiatrist (L.R.K.). The study was approved by the Mt. Sinai Hospital Research Ethics Board in Toronto. Descriptive statistics were analyzed by using SPSS Statistics, version 24.
Results
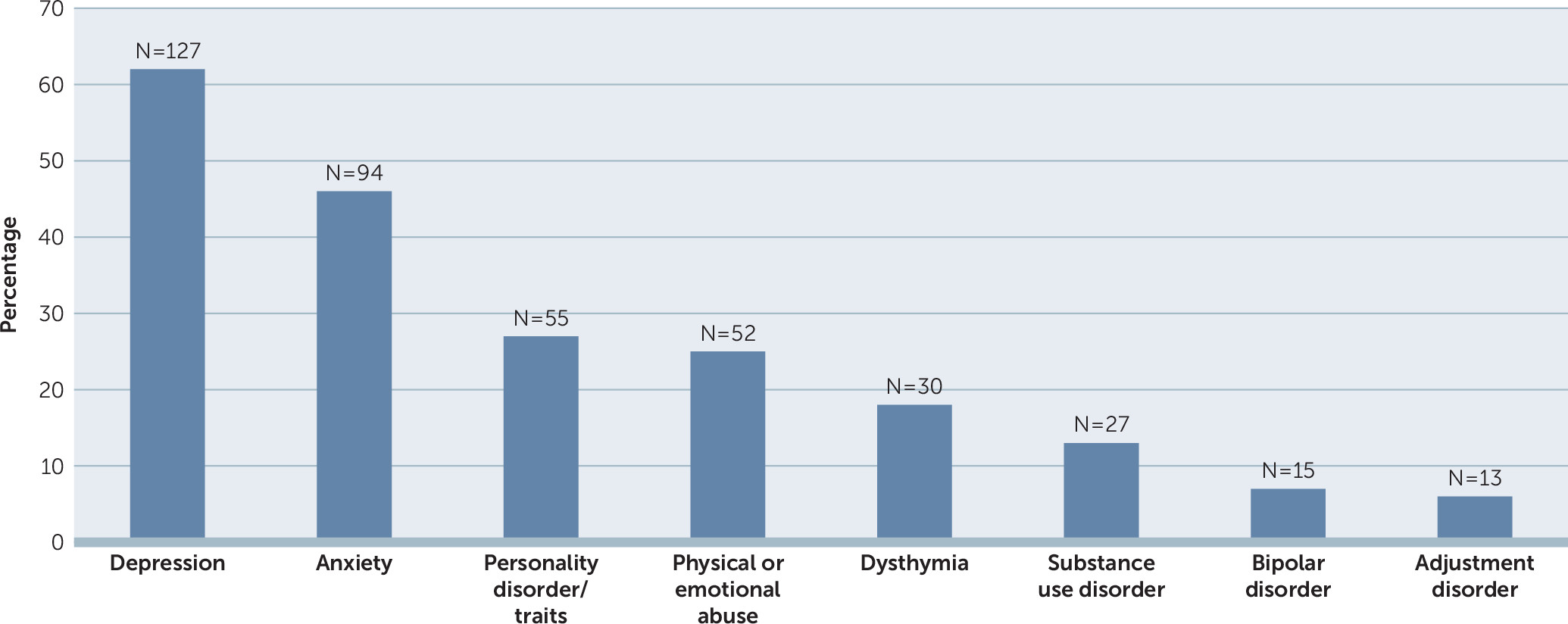
The case reports from 184 clinically supervised psychiatry residents providing treatment in university-affiliated teaching hospital sites described 204 patients receiving psychodynamic psychotherapy. The case reports included the age and gender of all patients. Most patients were female (N=130, 64%); average age was 37 years (range 14–79). Race-ethnicity and country of origin or religion were reported for 48% (N=98 of 204), and a majority of the case reports described patients as Caucasian (62%, N=61 of 98). In the 98 reports that included demographic information beyond gender or age, 37 (38%) mentioned religion (e.g., Muslim, Jewish) or countries of origin and family backgrounds (i.e., Argentina, Bosnia, Brazil, Canada, China, Columbia, Ecuador, India, Iran, Israel, Italy, Jamaica, Macedonia, Mexico, Pakistan, Philippines, Russia, Scotland, Sri Lanka, Trinidad, Uganda, Vietnam). The most common diagnoses (
Figure 1) were depression (N=127, 62%), anxiety disorders (N=94, 46%), and personality disorder or traits (N=55, 27%).
We found that 42% (N=86) of patients had current prescriptions for psychiatric medication. In addition, 86% (N=175) had engaged in prior psychiatric treatment, including 52% (N=106) who had tried at least one psychiatric medication and 78% (N=159) who had been treated with some other form of psychotherapy. Sixty-three (31%) patients had previously engaged in three or more interventions or therapies, including a variety of short-term psychotherapies other than medications.
Only 15% (N=31) of patients had no previous diagnosis; 48% (N=97) had two or more previous diagnoses. Twenty-six percent (N=52) of case reports described a history of abuse (physical or emotional), and 34% (N=70) described patients as having insecure attachment.
Discussion
Psychodynamic psychotherapy is effective for a wide range of psychiatric disorders (
10,
11), and its elements, including case formulation, empathic engagement, and management of the dynamics of the therapeutic alliance, are generalizable to other psychiatric contexts. The results of this study indicated that patients who received psychodynamic psychotherapy from our psychiatry residents had complex psychiatric histories with comorbid conditions and chronic struggles that were comparable to patients described in studies of long-term psychotherapy in private practice (
1,
10). Compared with private practice patients, our sample had a smaller percentage of patients with personality disorders (27% vs. 66%–75%) (
1,
10), possibly because educators select more straightforward cases for trainees. Leichsenring and Rabung’s (
10) meta-analysis of patients receiving long-term psychodynamic psychotherapy found, similar to our results, that approximately 40% required a combination of medication and psychotherapy and had numerous comorbid psychiatric disorders, with a significant portion struggling chronically (e.g., with dysthymia/persistent depressive disorder).
A majority (64%) of the residents’ patients were women, possibly because the most frequent diagnosis was depression, which is more prevalent among women. Gender disparities may also have occurred in the prescribing, seeking, or acceptance of a talk therapy. Cultural factors, including race-ethnicity, country of origin, gender identity, and religion, are important in shaping one’s sense of identity. In this study, however, cultural factors were not reported for about half the patients. Similarly, a history of abuse was only reported for about 25% of the patients, a percentage lower than that found in another study (
14) of psychiatric patients from similar referral sources. These elements were either overlooked or not considered salient by the residents, or the sample was not representative of Toronto’s diverse population. Cultural considerations, the endemic and long-term sequelae of trauma, and equitable access to care are important, so these observations require further study.
Pejorative media characterizations of patients who access intensive psychotherapeutic care appear in the context of important public health concerns related to equitable treatment access. Although time-limited structured psychotherapies are effective in treating individuals with mild-to-moderate depression or anxiety, patients with chronic or severe symptoms, a history of trauma, and multiple psychiatric disorders require longer-term continuity of psychiatric care with medication and/or psychotherapy (
13). Access to longer-term psychotherapy is needed so as to not undertreat, disproportionately disadvantage, or stigmatize vulnerable patients with high-level mental health care needs (e.g., those with chronic or severe symptoms, a history of trauma, multiple psychiatric disorders) (
15). These are the kinds of patients the psychiatry residents of the current study treated with psychodynamic psychotherapy. As mental health specialists, psychiatrists need to be prepared to help patients who have experienced treatment failure; have chronic, complex, and/or comorbid mental health conditions; and who may need psychodynamic psychotherapy or other longer-term treatments, alone or in combination with medication.
Limitations to this study included its retrospective nature and the incomplete reporting of demographic characteristics, trauma history, and cultural factors in the residents’ case reports. Because the data were drawn from the patients of only one university’s psychiatric resident population, the findings may not be generalizable to other populations. However, the residency program studied was large and included patients treated at multiple university-affiliated teaching hospitals. Further research is needed in other educational settings, along with reporting of long-term patient outcomes, trauma histories, and expanded demographic information to include cultural factors. This descriptive study has expanded the literature by providing data on actual patients receiving psychodynamic psychotherapy. The validity of the results is strengthened by the fact that data were extracted from a large number of case reports, and diagnoses were made by psychiatry residents trained in diagnostic assessment and confirmed by clinical faculty.
Conclusions
Our results indicate that most of the patients treated by the resident trainees began psychodynamic psychotherapy with previous psychiatric diagnoses and treatment experiences suggestive of complexity, long illness duration, and past treatment attempts that did not achieve or sustain recovery. Consistent with community-based findings, this study defines the profile of an individual in long-term psychotherapy as a patient with a persistent psychiatric illness unresponsive to less intensive treatment.
Acknowledgments
The authors thank Dr. Robert Maunder; the residents, their patients, and the clinical faculty supervisors, Department of Psychiatry, University of Toronto; and the Morgan Firestone Psychotherapy Chair, Department of Psychiatry, Sinai Health System.