Clinical and Physiological Effects of Stereotaxic Bilateral Amygdalotomy for Intractable Aggression
Abstract
CASE DESCRIPTIONS
Amygdalotomy Case 1 (R.L.). At the time of surgery in the late 1980s, R.L. was a 19-year-old right-handed white male who was the product of a normal pregnancy and birth and showed normal growth, development, and school performance until the age of 10 years, when he contracted viral encephalitis thought to be caused by herpes simplex. One month later, R.L. developed complex partial seizures with secondary generalization that have been well controlled with antiepileptic drugs. In the months subsequent to his initial illness, R.L. showed profound behavioral changes characterized chiefly by severe disinhibition of affect and impulsivity as evidenced by outbursts of aggressive rage. Because of the severity of his behavioral disturbance, R.L. was unable to continue his education, and he stopped attending school in the fifth grade. There were multiple psychiatric hospitalizations for violent outbursts until he was permanently institutionalized at age 13 years. Pharmacological therapy by many different psychiatrists and neurologists over 9 years (ages 10–19) did not control the aggressive outbursts.Repeated preoperative neurological examinations were normal, the patient showing no sensory, motor, cranial nerve, reflex, or cerebellar abnormalities. Multiple EEGs were normal with the exception of one that showed spike and sharp wave activity over the right temporal region. Preoperative CT scan of the head revealed a small, low-density lesion in the left dorsomedial thalamic region but was otherwise normal. This patient has been the subject of several previous reports.9,29,43 The patient and his family were fully informed about the risks and possible benefits of the surgery, and written informed consent was obtained.
Amygdalotomy Case 2 (D.B.B.). At the time of surgery in the late 1980s, D.B.B. was a 21-year-old right-handed white male who was the product of a normal pregnancy and birth. He showed normal growth and development until he was 8 months old, when he contracted chickenpox encephalitis. Approximately one year later, he developed partial complex seizures that were well controlled with antiepileptic drugs. School performance and behavior were reportedly normal until age 12 years. At that time uncontrollable episodes of rage directed against people and objects began during puberty and gradually became more frequent and serious until he was institutionalized at age 13 years. D.B.B.'s outbursts of rage resulted in an inability to attend school beyond the ninth grade. Pharmacologic management by many different physicians over 9 years (ages 12–21) did not adequately control the aggressive outbursts.Neurological examinations conducted over a 20-year period were generally within normal limits. One week prior to surgery, there was moderate nystagmus on vertical and horizontal gaze and slight instability during tandem walking. CT and MRI scans 2 months before surgery were normal. An EEG 2 months before surgery was abnormal due to diffuse slowing. The patient and his family were fully informed about the risks and possible benefits of the surgery, and written informed consent was obtained.
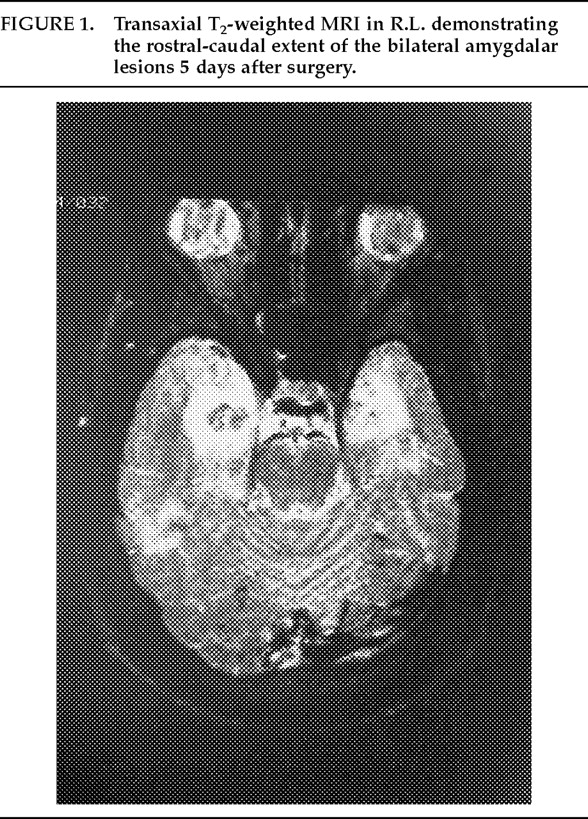
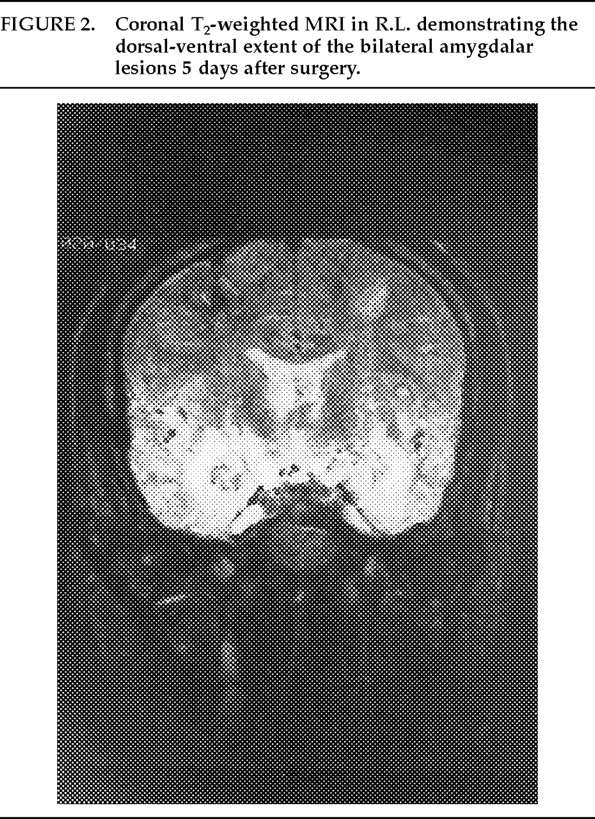
Description of Surgery. Bilateral amygdalotomies were performed on R.L. and D.B.B. under general endotracheal anesthesia with a modified Todd-Wells stereotaxic apparatus. Quarter-inch (0.64 cm) twist drill holes were placed 3 cm to either side of midline on a plane with the coronal suture. Target points were derived from examination of preoperative MRI scans, a standard stereotaxic brain atlas,44 and lateral skull X-rays obtained after the patients' heads had been fixed in the stereotaxic apparatus. Left amygdalar targets were located 18 mm and 23 mm to the left of midline. Right amygdalar targets were located 20 mm and 25 mm to the right of midline.The deepest lesions on both sides were located at the level of the base of the dorsum sellae. A temperature-monitoring electrode with a 2.1 mm×5 mm uninsulated tip (Radionics, Cambridge, MA) was used at a temperature of 80° C for 90 seconds in all lesioning. Deep, intermediate, and superficial lesions were made at 4-mm intervals for each of the target sites. The estimated size of the completed lesions was 15 mm in diameter in both patients, and this was verified by postoperative MRI scans. This lesion size ensured complete, or nearly complete, destruction of the amygdalar complex in both patients (Figures 1, 2, and 3).
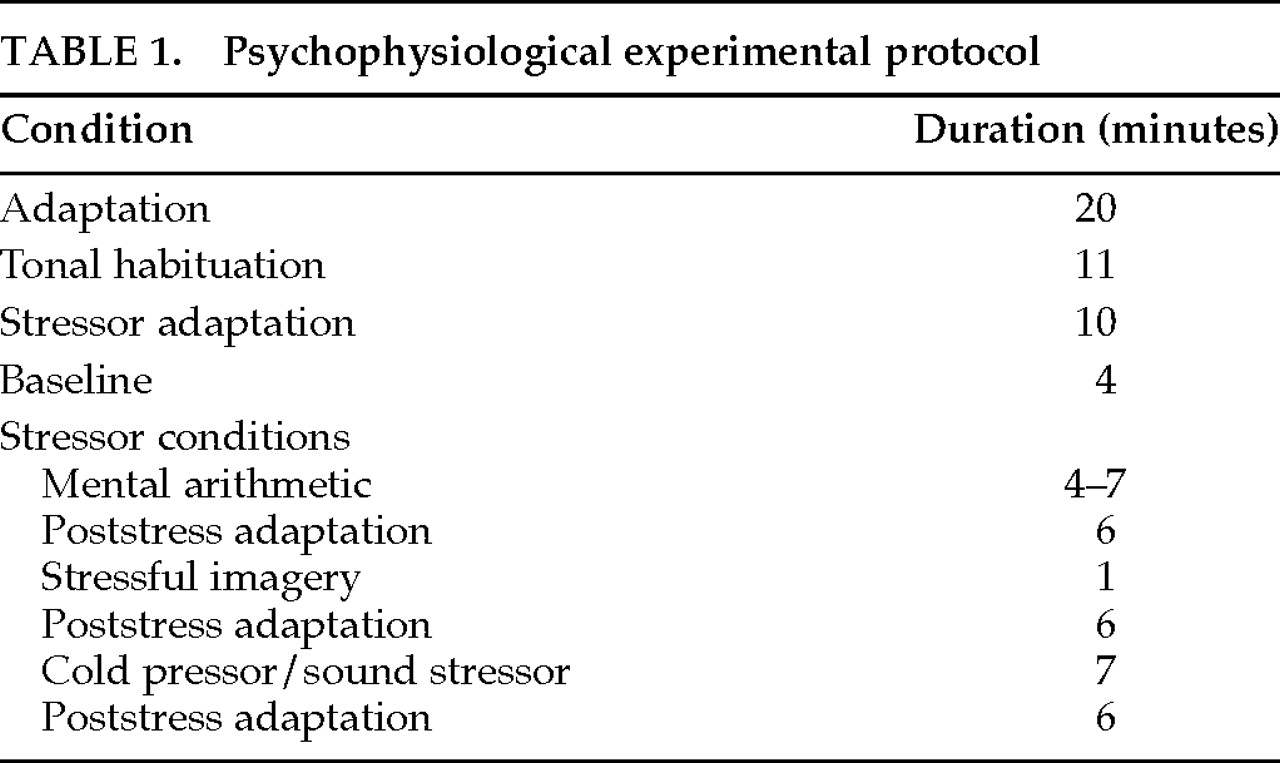
Procedures. Psychophysiological measures included electromyography (EMG) of facial muscles and skin conductance response (SCR) measured from the hands. A Grass model 7400 physiological recorder was used. For facial EMG recording, the physiological recorder was connected to a high-performance AC signal conditioner. For SCR recording, the physiological recorder was connected to an AC/DC transducer signal conditioner, interfaced with an SCA1 skin conductance adapter. The physiological recorder was equipped with a built-in computer for data analysis and storage.Tonal habituation apparatus, to measure SCR habituation, consisted of a Macintosh PowerBook computer with a software program that delivers a 1-second, 60-db tone bilaterally through stereo earphones. There was at least a 10-second interval between the delivery of two consecutive stimuli. A change in skin conductance ≥0.5 microSiemens (μS) was considered to be a tonal response. Habituation was defined as an absence of response for six consecutive trials with no consistent series of responses occurring for the remaining trials.SCR was measured in microSiemens with disposable Ag-Cl electrodes attached to the thenar and hypothenar eminence over the palm of the left hand. SCR was time sampled every 60 seconds during the stressor conditions by recentering the pen and noting the value. During the tonal habituation condition, SCR was monitored constantly.Facial EMG measurements were obtained from the frontalis muscle by attaching two disposable Ag-Cl electrodes to the forehead, approximately 2.5 cm above the left eyebrow. One was an active electrode that was placed in line with the pupils and another was a ground electrode that was attached to the middle of the forehead in order to minimize 50-Hz artifact. Following electrode attachment, electrode impedance was checked; an acceptable criterion was 10 kΩ or less. EMG was determined by integrating amplitude in μV across each second and averaging every 10 seconds. Bandpass was set at 100–200 Hz.Psychophysiological assessments were performed 1 day before and 5 days after surgery on patient R.L., and 2 days before and at both 5 months and 8 years after surgery on patient D.B.B. Informed consent was obtained from both patients after the procedures had been fully explained. Autonomic measurement and stressor condition procedures differed slightly at the 8-year assessment. Sessions lasted approximately 75 minutes and consisted of an adaptation and several stressor conditions listed in Table 1.
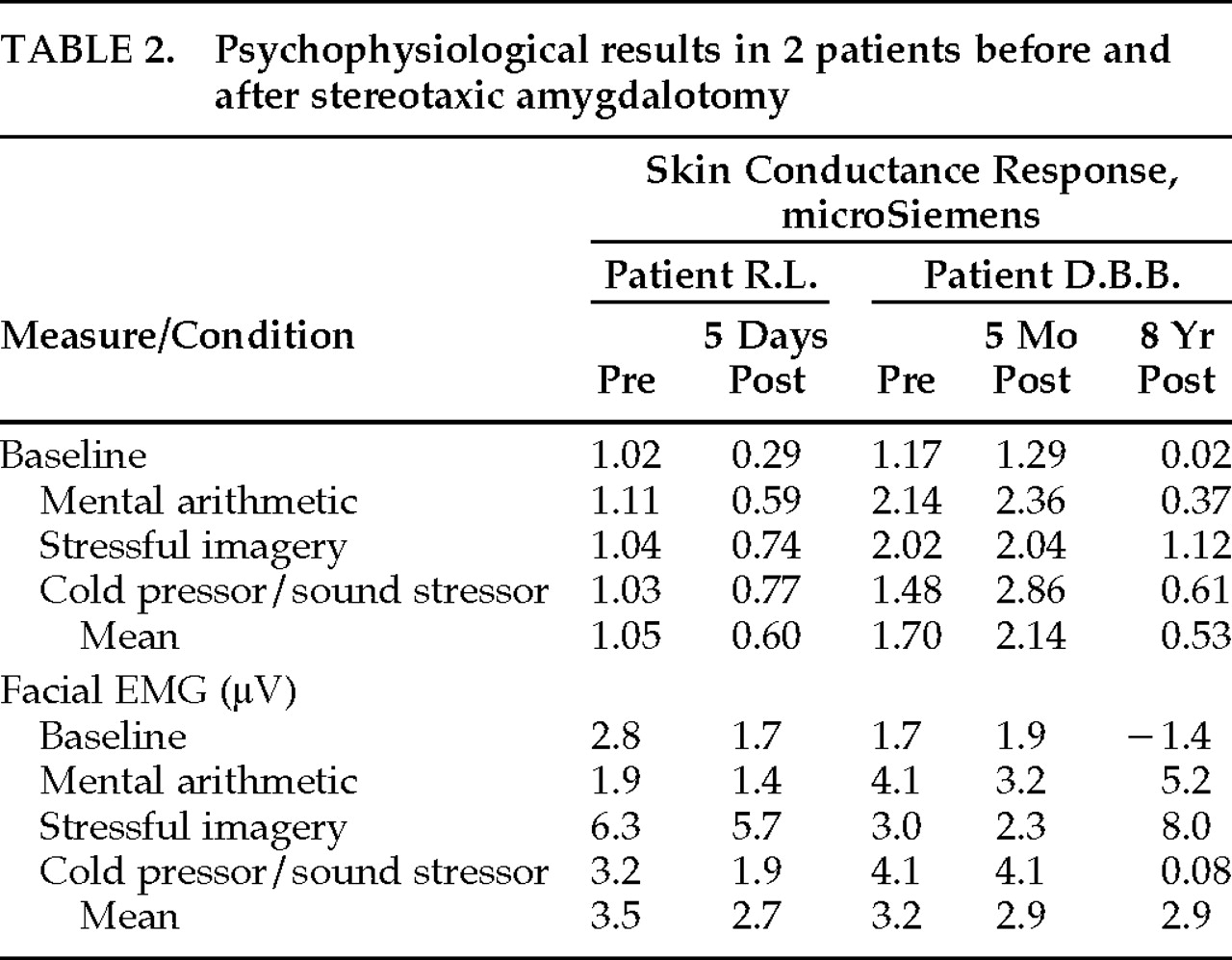
Physiological Results. Skin conductance response habituation to the tonal stimulus did not occur after 60 trials in patient R.L. before amygdalotomy, whereas after surgery patient R.L. showed normal tonal habituation (within 14 trials). Patient D.B.B. displayed no SCR to the tonal stimuli either before or 5 months after amygdalotomy, but he displayed normal SCR tonal habituation (within 13 trials) at the 8-year assessment.Table 2 provides SCR and facial EMG results before and after amygdalotomy for each of the four experimental conditions (baseline and three stressor conditions). As shown in Table 2, the physiological assessment revealed marked autonomic hyperarousal in both patients before surgery. The preoperative mean SCRs were 1.05 and 1.70 μS in our patients—considerably more than reported in normal control subjects, where it typically ranges between 0.115 and 0.626 mean μS.38,45As may also be seen in Table 2, there were statistically significant reductions in SCR following amygdalotomy in both R.L. (F=17.3, df=3,37, P=0.02) and D.B.B. (pre vs. 5 mos. post vs. 8 yrs. post, F=17.3, df=3,58, P=0.003). Follow-up analyses in D.B.B. revealed no statistically significant differences between the preoperative and 5-month postoperative SCR results (Scheffé F=1.18, P>0.05), however, both preoperative SCR (Scheffé F=8.59, P<0.05) and 5-month postoperative SCR (Scheffé F=16.15, P<0.05) differed from the 8-year postoperative SCR results to a statistically significant degree.There was a statistically significant facial EMG reduction in R.L. after surgery (F=20.53, df=3,4, P=0.02), but a similar statistically significant reduction was not seen in D.B.B. (F=0.02, df=3,8 P>0.05). None of the follow-up analyses between each of D.B.B.'s three facial EMG assessments achieved statistical significance.
Clinical Results. With regard to the efficacy of the bilateral amygdalotomy, there was a decline in the number of aggressive outbursts in both patients, but they both have continuing difficulties controlling aggressive outbursts. Similar to the physiological results, the “taming effect” following surgery was immediate in R.L. and took place more gradually in D.B.B.Because R.L. remained in a psychiatric facility after the amygdalotomy until 1997, follow-up has been meticulously documented. Before surgery, R.L. averaged 7 assaultive outbursts each month. During the first year after surgery, R.L. had only 1 documented assaultive episode. In the second postoperative year, R.L.'s aggressive outbursts rebounded to an average of 5 assaults each month. Since that time these outbursts have again declined. R.L. has averaged approximately 1 assaultive episode every other month for the past 8 years. Aggressive outbursts have consisted of self-abuse (e.g., stabbing neck with pencil, slamming head against wall, drinking liquid laundry detergent), destruction of property (e.g., breaking windows, tearing clothing off himself, throwing and breaking ceramics, destroying furniture), and assaults (e.g., biting, kicking, hitting, and stabbing others, resulting in broken bones, teeth, dentures, and glasses). In 1997, R.L. was discharged after 16 years from a state hospital to a personal care home. He has lived there without an assaultive outburst for 7 months.Although the effects of the amygdalotomy are more difficult to establish in D.B.B. because of frequent changes in living circumstances, the surgery ultimately must be considered a failure. In the year before surgery, D.B.B. reportedly had daily episodes of aggressive outbursts consisting of throwing, kicking, and breaking objects, and he physically attacked others 1 to 2 times each week. According to his parents, there was no change in D.B.B.'s pattern of aggressive outbursts during the first 3 months after surgery (daily angry outbursts). Beginning in the fourth postoperative month, the temper tantrums began to diminish in frequency and severity. Over the past 8 years D.B.B. has lived in many different personal care homes because his parents became unable to take care of him. Telephone interviews with his caretakers revealed that physical assault on others was an exceedingly rare event. However, impulsive outbursts not involving aggression against others (e.g., running away, spending all his money immediately after receiving it, compulsive alcohol consumption) have been more common, occurring approximately once per week. In late 1996, D.B.B. assaulted the supervisor of his personal care home, causing the supervisor to suffer significant head injury (coma lasting several days), multiple broken bones, and loss of an eye. Bystanders reported that D.B.B. stopped this assault only after being restrained by other residents of the personal care home. The patient was arrested and imprisoned until the following summer, when he was found not guilty by reason of insanity and committed to the forensic unit of a state psychiatric hospital.With regard to cognitive outcome, repeated neuropsychological examinations over the years have shown no significant pre- to post-amygdalotomy changes in any area of cognitive functioning, including intellectual functions, new learning and memory, language, visual perceptual and visual spatial functions, sensorimotor abilities, and complex problem solving. Details of many of the cognitive examinations have been reported previously.43,46
DISCUSSION
ACKNOWLEDGMENTS

References
Information & Authors
Information
Published In
History
Authors
Metrics & Citations
Metrics
Citations
Export Citations
If you have the appropriate software installed, you can download article citation data to the citation manager of your choice. Simply select your manager software from the list below and click Download.
For more information or tips please see 'Downloading to a citation manager' in the Help menu.
View Options
View options
PDF/EPUB
View PDF/EPUBLogin options
Already a subscriber? Access your subscription through your login credentials or your institution for full access to this article.
Personal login Institutional Login Open Athens loginNot a subscriber?
PsychiatryOnline subscription options offer access to the DSM-5-TR® library, books, journals, CME, and patient resources. This all-in-one virtual library provides psychiatrists and mental health professionals with key resources for diagnosis, treatment, research, and professional development.
Need more help? PsychiatryOnline Customer Service may be reached by emailing [email protected] or by calling 800-368-5777 (in the U.S.) or 703-907-7322 (outside the U.S.).