New brain imaging technologies are yielding information about structural or functional abnormalities in patients with various psychiatric disorders. These imaging modalities include magnetic resonance imaging; positron emission tomography of regional cerebral metabolic rate, regional cerebral blood flow, and radioligand binding to receptors of neurotransmitters; single-photon emission computed tomography; functional magnetic resonance imaging; magnetoencephalography; quantitative electroencephalography (QEEG) and event-related potentials (ERP); topographic QEEG and statistical probability mapping; and low-resolution electromagnetic tomography. Evidence from these brain imaging methods has unequivocally established that “mental illness” has definite correlates with brain dysfunction. QEEG and ERP methods afford the psychiatric practitioner a set of noninvasive tools that are capable of quantitatively assessing resting and evoked activity of the brain with sensitivity and temporal resolution superior to those of any other imaging method.
Conditions such as anxiety disorder, depression, dementia, obsessive-compulsive disorder, schizophrenia, learning disabilities, and attention deficit disorder with and without hyperactivity are now understood to involve interactions between brain dysfunctions or altered neuroanatomical structure and environmental influences. Medications that profoundly alter the availability of neurotransmitters and affect a hypothesized pathophysiology are routinely prescribed by psychiatric practitioners. Nonetheless, little or no attempt is made in most cases, even in the treatment-resistant patient, to use biological assessment methods to select a treatment, to evaluate its physiological effect, and to demonstrate its efficacy objectively. Relevant biological measurements may become invaluable adjuncts for the selection and evaluation of treatment and may minimize false starts, decrease severity and shorten duration of symptoms, and markedly reduce costs. In this era, it will become increasingly essential to demonstrate the need for treatment and to substantiate its efficacy.
EEG AND QEEG
Of all the imaging modalities, the greatest body of replicated evidence regarding pathophysiological concomitants of psychiatric and developmental disorders has been provided by EEG and QEEG studies. Electrophysiological assessment is also the most practical of these methods, using relatively simple, inexpensive, compact equipment readily accommodated by clinics, hospitals, or private offices. QEEG analytical algorithms are widely available from commercial sources, and workshops with continuing medical education accreditation in collection, analysis, and interpretation of data are now regularly presented by professional societies as well as equipment manufacturers. However, despite extensive evidence of sensitivity and specificity, the adoption of QEEG by the psychiatric community has been slow. Two major factors may account for this.
First, the numerous reports of abnormalities found in psychiatric patients by visual inspection of the conventional EEG have been regarded as too nonspecific and are usually not included in increasingly compressed curricula. Further, the great majority of recent papers reporting the results of EEG, QEEG, and ERP studies of psychiatric patients have appeared not in psychiatric journals, but rather in specialized electrophysiological or brain research publications.
Second, there has been considerable controversy about the clinical utility of QEEG in position papers published by various professional organizations over the past decade,
1–4 concluding, in the words of one such statement, that “the clinical application of Quantitative EEG is considered to be limited and adjunctive…clinical use…must be an extension of routine EEG.”
1 These statements cited only a very few published findings in psychiatric disorders, which were frequently grouped with “other disorders” (including tumors, multiple sclerosis, migraine, solvent exposure, and radiation exposure).
During the last decade, more than 500 EEG and QEEG papers have reported well-designed studies, concurring that EEG and QEEG abnormalities are found in a high proportion of psychiatric patients. Individual studies usually include a substantial number of psychiatric patients and normal control subjects, and across all studies within any particular disorder, the overall sample size is very large. An overview of the findings reveals numerous consistent and concordant conventional EEG and QEEG findings among studies within the same DSM diagnoses. Many of these studies have been on never-medicated or unmedicated patients who have been medication free for substantial periods. Statistical significance, specificity, and sensitivity have been high. No comprehensive review of this large body of psychiatrically relevant literature has yet appeared.
This article provides a comprehensive, updated review of how conventional EEG and QEEG can be useful in present clinical psychiatric practice. Other relevant reviews have appeared.
5–8Basic QEEG Definitions
In QEEG, multichannel recording (usually 19 electrodes at standardized positions) of eyes-closed, resting or “background” EEG are visually edited and a sample of artifact-free data, usually 1 to 2 minutes, is analyzed, using the Fast Fourier Transform (FFT) to quantify the power at each frequency of the EEG averaged across the entire sample, known as the power spectrum. The test-retest replicability of power spectra thus computed has been shown to be highly reproducible in works cited below. The power spectrum of clinical interest is usually considered to extend from about 1 Hz to 20 Hz.
This frequency range has traditionally been separated into 4 wide frequency bands, typically defined as delta (1.5–3.5 Hz), theta (3.5–7.5 Hz), alpha (7.5–12.5 Hz), and beta (12.5–20 Hz). Results from each electrode can be represented as absolute power in each band (total μV2), relative power in each band (percentage of total power in each channel), coherence (a measure of synchronization between activity in two channels), or symmetry (the ratio of power in each band between a symmetrical pair of electrodes).
Neurophysiological Basis of EEG
Research on the origins of rhythmic brain electrical activity in the various frequency bands indicates that anatomically complex homeostatic systems regulate the EEG power spectrum. Brainstem, thalamic, and cortical processes involving large neuronal populations mediate this regulation, using all the major neurotransmitters.
9–12Pacemaker neurons distributed throughout the thalamus normally oscillate synchronously in the 7.5–12.5-Hz frequency range. Efferent projections globally distributed across the cortex produce the rhythmic electrical activity known as the alpha rhythm, which dominates the EEG of an alert healthy person at rest. Nucleus reticularis can hyperpolarize the cell membranes of thalamic neurons by gamma-aminobutyric acid (GABA) release, slowing the dominant alpha rhythm into the lower theta range (3.5–7.5 Hz) and diminishing sensory throughput to the cortex. Slow delta activity (1.5–3.5 Hz) is believed to originate in oscillator neurons in deep cortical layers and in the thalamus, normally inhibited by input from the ascending reticular activating system in the midbrain. The faster activity in the beta band (12.5–20 Hz) is believed to reflect corticocortical and thalamocortical transactions related to specific information processing.
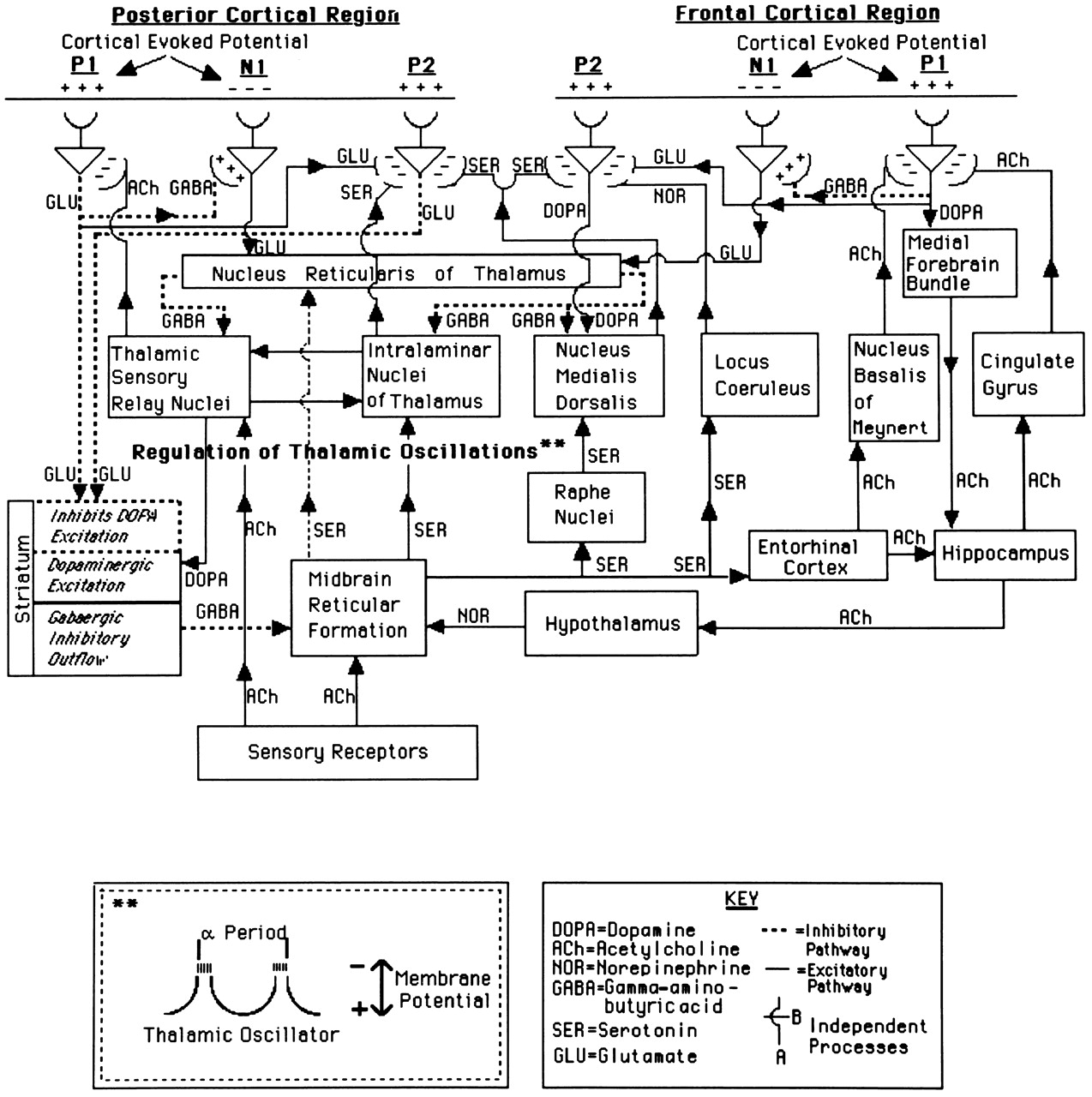
The changes characteristically seen in the disorders reviewed in this paper may be understood by referring to
Figure 1. Activation of the mesencephalic reticular formation (MRF) causes inhibition of the nucleus reticularis by cholinergic and serotonergic mediation, which releases the thalamic cells from inhibition by the
n. reticularis. The dominant activity of the EEG power spectrum becomes more rapid, with the return of alpha activity and the higher frequency beta activity, and the flow of information through the thalamus to the cortex is facilitated.
The cortex can activate n. reticularis directly by glutamatergic pathways to suppress the arrival of information to the cortical level and, by striatal projections, dopamine can inhibit the MRF. Such inhibition of the MRF enables inhibition of thalamic neurons to occur and blocks the flow of sensory information through the thalamus to the cortex.
This model suggests that deficiencies or excesses of any of the neurotransmitters should produce marked departure from the homeostatistically regulated normative EEG spectrum. Such neurotransmitter perturbations are widely believed to make decisive contributions to much psychiatric pathophysiology.
The EEG power spectrum can be reasonably expected to be stable and characteristic for healthy human beings, as a result of homeostatic regulation by these processes, with high specificity probably reflecting our common genetic heritage. It is also reasonable to expect sensitivity in these measures to many dysfunctions believed to be abnormal in some psychiatric disorders. The data support these expectations.
Stability and Specificity of the EEG Power Spectrum as the Basis of QEEG
During the period when the origins of the EEG were being illuminated by studies such as those cited above, the resting EEG power spectra of large samples of healthy, functioning individuals across a wide age range were being studied quantitatively. Initial studies of this sort, using analog methods, showed systematic changes from ages 17 to 64,
13 and then from ages 1 to 21,
14 in the average power in the delta, theta, alpha, and beta frequency bands. These normative data were soon replicated by use of general-purpose digital computing equipment. Age regression is necessary to correct for maturational effects. Not only were the systematic changes with age confirmed, but no significant differences were found between the EEGs of normally functioning Swedish children and white or black U.S. children.
15 Soon thereafter, normally functioning black children in Barbados were found to display the same values of the EEG power spectrum as the U.S. and Swedish groups.
Since then, numerous studies have confirmed the high specificity of normative distributions of power in the delta, theta, alpha, and beta bands. Positive findings different from the normative database in healthy, normally functioning individuals have repeatedly been shown to be within the chance levels, with very high test-retest reliability.
16,17 Normative data have been extended to cover the age range from 1 to 95 years for each electrode in the standardized International 10-20 System and have been broadened to include measures of absolute power, relative power, mean frequency, coherence, and symmetry, as well as covariance matrices that quantify normal brain relationships.
18–20 These multivariate composite measures are unique to QEEG; psychiatric disorders rarely entail focal abnormalities.
The independence of the normative QEEG descriptors from cultural and ethnic factors enables objective assessment of brain integrity in persons of any age, origin, or background. This independence and specificity, as well as high replicability, has been established in studies from Barbados, China, Cuba, Germany, Holland, Japan, Korea, Mexico, Netherlands, Sweden, the United States, and Venezuela.
17,21–33 If normative distributions of QEEG measures are made gaussian,
15,22 then the incidence of false positive QEEG findings obtained from visually edited, artifact-free resting EEG recordings is at or below the level expected by chance. If one were to require that the QEEG evaluation be performed on two separate samples and that any significant finding deviant at the
P≤0.05 level be replicated in each of these two samples, the probability that this would occur by chance would be approximately
P×
P, or 0.05×0.05, or 0.0025. If such a replication were required, false positives would seem rather unlikely. Such a high level of specificity is beyond the confidence level achieved by many routinely used clinical tests, such as mammograms, cervical screenings, or CT brain scans.
34Why Should Psychiatric Patients Have EEG Studies?
In psychiatric diagnostics, physical or neurological conditions must be ruled out before a psychiatric disorder can be diagnosed.
35 As many as 64% to 68%
2,3 of EEGs in psychiatric patients provide evidence of pathophysiology, and these results have additional utility beyond simply ruling out “organic brain lesions.”
3 Such electroencephalographic studies may also aid in differential diagnosis, treatment selection, and evaluation. Some longitudinal studies show that initial quantitative EEG profiles may distinguish among patients with the same DSM diagnosis who will respond preferentially to different medications or who will display different evolution of illness.
CONVENTIONAL AND QUANTITATIVE EEG STUDIES
A voluminous literature attests to the robustness of conventional EEG studies and their clinical utility in disorders of brain function. This approach has contributed valuable information for the clinical psychiatrist. This method is essentially based on visual pattern recognition. Over the past 20 years, algorithms for computer pattern recognition, the computer's unsurpassed capacity to measure and calculate, and the availability of normative databases across the human life span have enhanced electroencephalography, supplementing the electroencephalographer's trained eye with a quantitative and objective description of a patient's EEG record (QEEG). Even more powerful are statistical comparisons between numerous measures from the individual patient and those of age-matched normal subjects or of patient subjects having different diagnoses.
These two EEG approaches complement each other: conventional EEG provides reliable diagnostic information, especially sensitive to “organic” or neurological disorders, detecting features of waveshapes, frequency relationships, and transitions of state seldom encountered in the healthy individual. QEEG enables precise comparison of the individual patient's record with normative and psychopathologic patient databases. Across both EEG and QEEG studies, a broad consensus exists on the high proportion of abnormalities found in different psychiatric disorders and often on their electrophysiological profiles. In most of these studies, patients were without psychotropic medication, except for some of the reports evaluating patients with mood disorders or schizophrenia. Most of the chronic patients in those studies had been drug free for some period before evaluation.
Dementias
Electroencephalography is particularly effective but generally underutilized in the evaluation of the confused or delirious patient. The hallmark of delirium usually is the slowing of the background EEG rhythm, to an extent that is positively correlated with the degree of severity of the condition. The one exception is in delirium tremens (DT), which usually shows a normal EEG record with fast rhythms.
2,36 If abnormal slow activity is found in the DT condition, consideration should be given to a Wernicke encephalopathy or to a hepatic disorder.
37 In the delirium accompanying the neuroleptic malignant syndrome, only a mild diffuse slow wave usually appears.
38 When delusional manifestations are prominent, as in organic delusional states, one typically finds increased slow-wave activity over both temporal lobes. Delirium can be differentiated from dementia, and the significant factors are an increased theta activity and increase in delta relative power.
39In organic syndromes showing cognitive deficits such as memory dysfunction, the prevalence of EEG abnormalities is directly related to the degree of cognitive impairment. If clinical impairment is equivocal, the incidence of EEG abnormalities is usually slightly over 40%; with a mild-to-moderate impairment, a 65% incidence is expected.
40 The EEG is a moderately sensitive, nonspecific indication of brain dysfunction, clearly useful in the diagnosis of Alzheimer's disease
41 and also AIDS dementia,
42 with general agreement in the literature that increased slow activity and decreased mean frequency are correlated with cognitive impairment and measures of clinical severity of Alzheimer's dementia.
3,43–45EEG frequency analysis allows confident detection of excessive slowing, more readily measured and quantified than conventional EEG. QEEG studies in dementia patients are in agreement with conventional EEG findings, reporting increased delta and/or theta power,
46–68 decreased mean frequency,
44,61,69,70 decreased beta power,
71,72 and decreased occipital dominant frequency.
53,58Many workers regard increased slow activity prior to reduction of alpha power as the earliest electrophysiological indicator appearing in Alzheimer's disease.
30,32,47,52,58,63,68,73 The amount of theta activity shows the best correlation with cognitive deterioration
11,14,29,31,74–77 and with clinical outcome in longitudinal follow-up,
59,63,68,73,78–80 although one report found no predictive utility.
81 Increased delta appears to be a correlate of severe advanced dementia, occurring subsequent to increased theta.
45,60,74,77In cerebrovascular disease, several EEG frequency parameters are highly correlated with regional blood flow or metabolism. Sensitivity and specificity are high for detection of ischemia-related diffuse or focal impairment.
23,82–88 These studies show sensitivity generally greater than 80%, false-positive rates below 5% to 10%, and correlations of
r>0.7 between EEG and blood flow in ischemic and nonischemic regions. EEG slowing is highly correlated with decreased regional cerebral blood flow
23,89–92 or metabolism.
10,38,54 QEEG can detect reliable focal features that are missed in the routine EEG and can be quite abnormal even when the CT is still normal, such as in the first 1 to 3 days after stroke or when the degree of ischemia is mild enough to cause dysfunction without infarction.
Alzheimer's dementia and multi-infarct dementia (MID) have been differentiated by evaluating asymmetry of slow activity
33,93 and coherence.
19,48,94 Multiple studies report accurate discrimination of Alzheimer patients from depressed patients or from normal subjects by use of EEG or QEEG measures of slow activity.
37,40,41,44,46,95 Accurate separation of Alzheimer's from frontotemporal dementia (Pick's disease) by use of QEEG has been reported.
96Conclusion:
Routine EEG has long been used to evaluate dementia and encephalopathy unresolved after initial clinical evaluation. There is excellent agreement between conventional and quantitative EEG studies of the dementias. QEEG may be useful in evaluating dementia or encephalopathy if routine EEG studies are not conclusive or if neuroimaging studies are inconclusive or unavailable, as well as in differentiating between Alzheimer's dementia, multi-infarct dementia, depression, and normal aging.
A broad consensus exists across a very large number of EEG and QEEG studies of dementia patients: Both kinds of studies report a diffuse increased delta and/or theta power, with decreased beta power and mean frequency. These features are absent in depression and are focal in multi-infarct dementia, enabling these disorders to be differentiated from Alzheimer's dementia. A good correlation exists between severity of cognitive impairment, clinical outcome, and amount of EEG slowing.
Schizophrenia
Numerous qualitative studies indicate abnormal conventional EEG findings in 20% to 60% of schizophrenic patients.
2,97,98 A more specific finding in schizophrenia is a relatively low mean alpha frequency,
98,99 although some patients may show a fast alpha rhythm.
100 Catatonic patients often present with paroxysmal activity.
101Numerous EEG and QEEG studies of background activity have been performed on carefully evaluated groups of unmedicated as well as medicated schizophrenic patients. Substantial agreement emerges from this body of literature. Deficient alpha power is consistently reported,
19,102–107 as well as altered alpha mean frequency or diminished alpha responsiveness.
98,108,109 Numerous studies have reported increased beta activity in schizophrenia.
105,110–113 Neuroleptics typically increase alpha power
113–115 and reduce beta power,
116,117 suggesting possible normalization of deviant features by medication.
Increased delta and/or theta activity has also been reported in a large number of studies.
101,102,105,106,118–125 Increased slow activity can apparently result from neuroleptic treatment,
126,127 although there are reports of increased delta in patients off medication for several weeks
102,105,128 and reduction of delta or theta when medication is resumed.
114,125,129 In the elderly schizophrenic patient, an increase in fast theta activity (7–7.5 Hz) is seen. A decrease in fast alpha (10–12 Hz) noted on the frontal areas has been called “hypofrontality.”
100Clinical relationships reported include 1) correlation between negative symptoms and delta waves in the temporal areas;
100 2) positive correlation between degree of QEEG abnormality and degree of clinical improvement,
130 raising the question of whether this “degradation” of the EEG is a necessary condition for a clinical improvement with clozapine; and 3) correlation between blink rates, alpha power, and smoking.
131 In sleep, a decrease has been found in stages III, IV, and REM, and also in REM latency and sleep continuity.
132–135Results from a small number of studies are inconsistent with this consensus of a QEEG profile, showing increased delta or theta, decreased alpha, and increased beta in schizophrenia. For example, increased slow activity has not been found by some workers,
136,137 and increased alpha
100 and decreased beta
106,120 have occasionally been reported. Not all of the studies reporting the increased slow activity/decreased alpha/increased beta profile found all of the indicated deviations. This inconsistency plausibly might arise from the coexistence of several subtypes with different QEEG profiles within the population of schizophrenic patients. Observations might depend on the mixture of subtypes within the relatively small samples collected for a particular study.
This heterogeneity has been recently documented in a large sample of medicated, nonmedicated, and never-medicated schizophrenic patients, using cluster analysis based on QEEG variables. Five subtypes were detected, with their QEEG profiles characterized by delta plus theta excess, theta excess, theta plus alpha excess with beta deficit, theta excess, and alpha excess with beta excess.
138 Never-medicated patients were classified into three of these subtypes. Schizophrenic patients with QEEG profiles corresponding to some of the groups identified by this cluster analysis have been reported to display differential responses to treatment with haloperidol
139or risperidone.
140 Additional evidence of heterogeneity in the schizophrenic population has been provided in QEEG studies by other groups.
141,142Findings of asymmetry in schizophrenia have been inconsistent. However, these findings depend upon whether measurements were made over anterior or posterior regions. When the electrode array covered both regions, power was highest over the right hemisphere in anterior regions, but over the left hemisphere in posterior regions.
20,120,142 This conclusion was supported by the cluster analysis just cited, in which this asymmetry pattern was found in every frequency band for all five subtypes.
138 However, increased amounts of delta activity in the left anterior temporal area
100 have been reported to discriminate schizophrenic patients from control subjects.
Increased interhemispheric coherence in anterior regions has been consistently found.
121,138,143–145 In view of the decreased frontal coherence in depressive illness cited below, QEEG separation of schizophrenic patients from bipolar depressed patients may be possible.
Conclusion:
Evaluation of EEG and QEEG literature on schizophrenia is complicated by the evident heterogeneity of the illness and the diversity of medication histories and dosage levels at the time of examination. In spite of these potential sources of difference among findings, considerable agreement nonetheless appears.
Across a large number of EEG and QEEG studies, there is a broad consensus that schizophrenia shows a high incidence of EEG and QEEG abnormalities. Most often, the reported abnormalities have been delta and/or theta excesses in frontal areas, a decreased mean frequency and lower power in the alpha band, and increased beta power. Increased anterior coherence also has often been reported. Coherence measures may contribute to distinguishing bipolar disorder from schizophrenia.
Mood Disorders: Unipolar and Bipolar Depression
The incidence of abnormal conventional EEG findings in mood disorders appears to be substantial, ranging from 20% to 40%
2,97,146–148 higher in 1) manic than depressed patients, 2) female than male bipolar patients, and 3) nonfamilial cases with late-age onset. Whether an “abnormal” EEG is a necessary correlate of a clinically effective series of ECT treatment is controversial. This suggestion, like that made above regarding clozapine in schizophrenia, will require further study.
Specific patterns noted in mood-disordered patients include the controversial small sharp spikes (SSS), 6/s spike and wave complexes, and positive spikes, seen especially in patients with suicidal ideation.
2,149,150 The SSS pattern appears often in bipolar patients and also in their first-degree relatives.
151Numerous QEEG studies have found increased alpha and/or theta power in a high percentage of depressed patients.
8,19,152–157 Antidepressants reduce alpha activity,
153,158–161 suggesting normalization of these deviant QEEG features (in contrast to the increased alpha caused by neuroleptics).
113–115 Interhemispheric asymmetry, especially in anterior regions, has been reported repeatedly,
162–166 as has decreased coherence.
19,121,167 In bipolar illness, in contrast to unipolar depression, alpha activity is reduced
155,168 and beta activity increased.
5,19 This difference may serve to separate unipolar from bipolar patients presenting in a state of depression without prior history of mania.
5,167Current treatment of bipolar disorder often includes the use of the anticonvulsant medications carbamazepine and sodium valproate. The successful use of these agents suggests overlap between convulsive disorders and bipolar illness. Ruling out convulsive illness with EEG studies prior to initiation of anticonvulsant treatment in bipolar patients may be prudent.
Conclusion:
Both EEG and QEEG studies report that a high proportion of patients with mood disorders display abnormal brain electrical activity. EEG studies report that small sharp spikes and paroxysmal events are often found, especially on the right hemisphere, and that abnormal sleep studies are common.
There is broad consensus in QEEG studies that increases in alpha or theta power, as well as asymmetry and hypocoherence in anterior regions, appear most often in unipolar depressed patients. Bipolar patients often display decreased alpha but increased beta activity.
Mood Disorders: Anxiety, Panic, Obsessive-Compulsive, and Eating Disorders
Several studies suggest a high incidence of EEG abnormalities in patients with anxiety disorders, panic disorders, and obsessive-compulsive disorder (OCD).
2,169–172 Diminished alpha activity has been found in anxiety disorder by using QEEG,
173,174 and increased theta activity has been reported in OCD.
175,176 Two subtypes of OCD patients have been described. One, with increased alpha relative power, responded positively (82%) to serotonergic antidepressants, while the second, with increased theta relative power, failed to improve (80%).
177 Epileptiform activity can occasionally be found in patients with tics (or stuttering), in addition to nonspecific diffuse slow activity.
178,179 In patients with panic disorder, paroxysmal activity was four times more common than in depressed patients.
180 Temporal lobe abnormalities, in particular, have been emphasized in QEEG studies in this type of patient.
In anorexia nervosa, abnormal background activity in the EEG can be seen in nearly 60% of patients, possibly related to the effect of starvation on cerebral metabolism. Paroxysmal abnormalities are seen in about 12% of these patients.
181 In intractable binge eating, “soft” neurological and EEG signs can appear. Both anticonvulsant and antidepressant drugs have been helpful in some of these patients.
182–184 Patients with eating disorders frequently give a history of physical or sexual abuse as children, so the increase in EEG abnormalities in this group may be related to their abuse history. Alternatively, dietary and nutritional deficiencies may contribute to altered brain function.
Conclusion:
Although abnormalities have been reported repeatedly in EEG and QEEG studies of patients in the above categories, consistent patterns have not yet been discerned.
Developmental Learning Disorders, Attention Deficit Disorders, and Autism
Specific developmental learning disorders (SDLD) are estimated to affect 4% to 6% of all school-age children.
21,185 Attention deficit disorders with or without hyperactivity (ADHD or ADD) have a prevalence of 6% to 9% in school-age children.
186,187 Although ADD/ADHD and SDLD are believed to be distinct neuropsychiatric entities, there is considerable comorbidity between the two disorders. Precise and accurate determination of the presence of ADD/ADHD versus SDLD can be of critical importance in avoiding the potentially devastating impact of these disorders on children and their families. EEG and QEEG can contribute usefully to this distinction as well as to separating children with social or motivational factors underlying school problems from those with organic dysfunction.
The conventional EEG has been reported to be abnormal in 30% to 60% of children with ADHD or with specific learning disability (SDLD or LD), as reviewed by several authors.
2,16,186,188–191 Reported abnormalities have often included diffuse slowing and decreased alpha activity.
In QEEG studies, a high incidence of excess theta or decreased alpha and/or beta activity has been reported in SDLD children,
18,21,33,192,186,187,193–197 with theta or alpha excess often seen in children with ADD or ADHD. The types of QEEG abnormality found in SDLD children are related to academic performance.
198 A large percentage of children with attention deficit problems (more than 90%) show QEEG signs of cortical dysfunction, the majority displaying frontal theta or alpha excess, hypercoherence, and a high incidence of abnormal interhemispheric asymmetry.
197,199 Using QEEG measures, it has been possible to discriminate replicably ADD/ADHD versus normal children, with a specificity of 88% and a sensitivity of 94%,
200 and ADD versus SDLD children, with a sensitivity of 97% and a specificity of 84.2%.
200The EEG is frequently abnormal in autism. In 14 studies encompassing approximately 800 patients, the mean incidence of abnormal EEGs was 50% (median 47%), but the range of values for the incidence of abnormalities was considerable (10%–83%). This large range undoubtedly arose from differences both in the populations under study and, more important, the criteria used for abnormality. EEG abnormality can help predict a poorer outcome with regard to intelligence, speech, and educational achievement.
151 Although clinical seizures are uncommon in autism, epileptiform activity sometimes occurs.
Conclusion:
Numerous EEG as well as QEEG reports agree that a high proportion of children with developmental disorders—among which learning disabilities and attention-deficit hyperactivity have received the most attention—display abnormal brain electrical activity.
There is a wide consensus that delta or theta excess and alpha and beta deficits are commonly encountered in children with learning disorders and that theta or alpha excesses are often seen in children with ADD/ADHD.
Alcohol and Substance Abuse
The changes during acute alcoholic intoxication include the slowing of the EEG, seen in the form of decreased alpha frequency and abundance, an increased amount of theta, and even some generalized delta rhythms.
201 These slow waves have a relationship with the degree of intoxication. The extent of the disturbance of consciousness is related to the amount of slow activity.
202For chronic alcoholism, as in the acute stage, an increase in slow activity is often seen. This change appears as a decrease in alpha frequency and abundance, related to the typical blood alcohol level of a given patient, and also an increase in the theta rhythm, especially on the temporal areas.
203,204 Temporal and frontal areas may also display an increase in fast activity related to the neuropsychological impairment, which must be distinguished from muscle artifact and often characterizes these records.
128,203 Family history of alcoholism plays a prominent role in the risk of the disease.
204–208 In the subacute encephalopathy associated with alcoholism, not only are slow waves noted, but epileptiform activity can also be seen, even as periodic lateralized epileptiform discharges (PLEDS).
209Recent studies of substance abuse have largely relied on QEEG. Replicated reports have appeared of an increased beta (relative power) in alcohol dependence.
19,128,203,204,207 Increased alpha power, especially in anterior regions, has been reported in withdrawal, as well as after acute exposure to cannabis.
210,211 Increased alpha and decreased delta and theta have been reported in crack cocaine users in withdrawal.
212–216Conclusion:
There is a broad consensus that both EEG and QEEG reveal marked abnormalities in alcoholics and substance abusers. The effects vary depending on the drug. Either increased slow activity with lower alpha and beta or the converse have been reported; this reflects the diversity of substances or states focused upon.
However, among numerous QEEG studies, there is a consensus of increased beta relative power in alcoholism and increased alpha in cannabis or crack cocaine users.
Mild Head Injury or Postconcussion Syndrome
Patients with complaints of cognitive memory or attentional deficit after mild head injury without loss of consciousness frequently present for psychiatric evaluation for worker's compensation and disability benefits. Objective evidence of brain dysfunction in such cases is critical in the endeavor to separate the truly dysfunctional patient from the malingerer. EEG/QEEG evidence can play a critical role in such cases. Although the absence of abnormal brain electrical activity cannot definitively exclude the possibility of brain dysfunction, the presence of abnormalities, especially those most frequently associated with unequivocal traumatic brain insult, must be considered supportive of such claims.
There is a high incidence of diffuse axonal injury, about 50%, in the 50,000 patients per year with head injury who recover; these patients characteristically do not display structural lesions on CT or even on MRI scans early after injury.
217,218 Among those who recover after moderate head injury, 90% have cognitive or neuropsychological deficits.
219 Among such patients, studies involving many hundreds of cases have reported normal neurologic examinations but abnormal EEG.
220–226 Numerous EEG and QEEG studies of severe head injury (Glasgow Coma Scale [GCS] 4–8) and moderate injury (GCS 9–12), using samples of 50 to 200 patients, have agreed that increased theta and decreased alpha power and/or decreased coherence and asymmetry often characterize such patients. Changes in these measures provide the best predictors of long-term outcome.
219,227–229The studies cited above generally concur that the most characteristic QEEG or EEG abnormalities persisting after mild or moderate head injury are similar in type to those found after severe head injury, namely increased power in the theta band, decreased alpha, low coherence, and increased asymmetry. It is noteworthy that similar EEG abnormalities have been reported in boxers,
230 correlated with the numbers of bouts or knockouts, and in professional soccer players who were “headers.”
231 These observations lend further credibility to the multiple reports of discriminant functions based on QEEG variables that successfully separated normal individuals from patients with a history of mild to moderate head injury years after apparent clinical recovery.
232,233Conclusion:
The consistency of these EEG and QEEG findings is high across the range from mild to moderate head injury as well as in sports-related head impacts, and similar types of abnormalities are observed in patients with severe head injury as they recover.
There is a broad consensus that increased focal or diffuse theta, decreased alpha, decreased coherence, and increased asymmetry are common EEG indicators of the postconcussion syndrome.
Three-Dimensional Statistical Probability Images: Source Localization and QEEG Tomography
In the last decade, the problem of three-dimensional localization of the sources of voltage fields detected on the scalp has been energetically attacked by mathematicians and physicists as well as neurophysiologists. Basic early approaches have been reviewed by Lütkenhöner et al.
234 and Buckner et al.
235The initial success in applying these new source localization techniques to electrophysiological signals was achieved by brain electrical source analysis, or BESA.
236–238 This method has received widespread acceptance for the separation and identification of highly localized dipole generators, such as focal epileptic discharges or spikes, and some neurosurgical centers have begun to use the method to pinpoint surgical targets in patients with intractable seizures.
Attention was directed next to localization of multiple sources, and then to the related problem of distributed sources, by the use of deblurring techniques.
239,240 Approaches to the localization of distributed sources have been explored in simulations, in patients with space-occupying lesions, and in psychiatric patients. These approaches have included localization of the centroids of FFT power maps,
241 frequency domain localization,
234 linearly constrained minimum variance spatial filtering,
242,243 recursive minimum norms,
244 optimal resolution kernels and the resolution field,
245,246 a Bayesian approach using anatomofunctional constraints,
247 and combinatorial optimization applied to finite element models.
235 Maximum likelihood procedures have been used to search for equivalent dipoles in 36 patients with space-occupying lesions. In 75% of these cases, the origin of deviant delta activity was localized near the center of the lesion volume, even in deep subcortical regions.
248Perhaps the most promising approach to the inverse solution of distributed sources is low-resolution electromagnetic tomography (LORETA),
249 a generalized minimum norm technique that has been analytically compared with several different solutions to the inverse problem and shown to be optimal.
250 It has been applied to the localization of intracranial epileptiform activity, using subdural electrodes to confirm inferences from scalp,
251 and to localizing space-occupying lesions with known positions based on CT scans.
248,252 Locations defined by LORETA were found to correspond well to the actual position of the abnormalities.
Using LORETA, a group of 9 never-medicated first-break acute schizophrenic patients was compared voxel by voxel with a group of 36 normal control subjects, indicating stronger activity in the right frontal regions but weaker activity in posterior regions in the schizophrenic patients than in the normal subjects.
253 These findings were in agreement with reports of hyperfrontality in some schizophrenic patients.
Topographic mapping of quantitative electrophysiological data has recently been extended to quantitative electroencephalographic tomography, or QEEG-T, by Valdes-Sosa.
254 A standard probabilistic brain atlas in Talairach space, constructed from more than 300 MRIs of normal individuals,
255 was evaluated, voxel by voxel, to constrain the hypothetical generators of the distributed inverse solution to gray matter. Regression equations were then computed for the log spectra of sources in every voxel of gray matter (3,500 voxels). These voxel-normative data spanned the age range 5 to 97 years and were calculated over spectra ranging from 0.39 to 19 Hz, in 0.39 Hz increments. Statistical probability tomographic images (SPTI) were then obtained by
Z-transformation of each voxel of the raw LORETA image obtained from an individual with respect to the corresponding voxel-normative data. Spatial statistical methods evaluated deviations from the norms of regions of interest, and results were displayed on slices from the probabilistic atlas with each voxel color coded for statistical significance.
QEEG-T has been used to seek CNS signs of HIV infection.
256 Observed changes were of particular interest because of similarity to those found with increasing cognitive deterioration in aging. When LORETA was used to study 319 elderly patients staged by scores on the Global Deterioration Scale, systematic changes in certain brain regions were found with increasing cognitive impairment.
257Positive findings with different anatomical distributions were also found among five subtypes of schizophrenic patients identified by cluster analysis,
138 OCD patients who were responders or nonresponders to selective serotonin reuptake inhibitors,
77 and children with ADHD who were or were not clinical responders to stimulant therapy.
200Conclusion:
The combination of QEEG with the distributed inverse solution technology of LORETA, along with the projection of statistically evaluated voxel source values on a probabilistic MRI atlas, may extend the clinical relevance of QEEG, yield valuable insights into the pathophysiology underlying some psychiatric disorders, and provide clues useful for the rationalization of pharmacotherapy.
SUMMARY
Both conventional EEG and QEEG studies provide valuable information to the psychiatrist regarding diagnosis and treatment responsiveness.
Conventional EEG is most useful in the following:
1.
Identifying paroxysmal activity.
2.
Identifying gross alterations in the background frequencies of the EEG.
3.
Identifying intermixed slow activity that may be related to delirium or dementia.
4.
Evaluating sleep disorders.
Conventional EEG assessments should be included in the diagnostic workup for the following:
1.
An acute confusional state.
2.
The first presentation of schizophrenia.
3.
A major mood disorder or mania.
4.
Refractory behavioral problems such as obsessions, violence, or panic.
Quantitative EEG studies are particularly well suited to identifying subtle changes in the topographic distribution of background activity. They can aid difficult differential diagnoses, such as:
1.
Distinguishing between delirium or dementia and depression.
2.
Distinguishing between schizophrenia and mood disorders.
3.
Assessing cognitive, attentional, or developmental disorders.
4.
Distinguishing between environmentally induced and endogenously mediated behavioral disorders.
5.
Evaluating alcohol or substance abuse.
6.
Evaluating postconcussion syndrome.
In dementia, multiple articles appearing within the last 5 years strongly suggest that QEEG may enable early detection and prognosis of future cognitive impairment. Such information might aid in development of prophylactic rather than remedial pharmacotherapeutic interventions, intended to prevent or slow further progress of the illness.
Some QEEG studies show promise of predicting the likelihood of response to a particular pharmacologic treatment and of monitoring responsiveness to treatment. The potential clinical value of QEEG procedures for analytic selection of the treatment most likely to be efficacious would be enormous in learning and attentional disorders and in schizophrenia.
Considerable attention is currently being given to the correlation of EEG or QEEG brain mapping with other brain functional mapping methods such as PET, SPECT, and MRI. Methods have been developed for the estimation of three-dimensional electrical source distributions in the brain computed from scalp recordings. If these source localization methods can be validated by more direct brain imaging using functional and structural MRI, PET, and SPECT, low-resolution electrical tomography offers the possibility of readily available, low-cost functional 3D brain images computed from QEEG recordings.
CONCLUSIONS
We have adopted the general procedures and the “quality of evidence” and the “strength of recommendation” ratings used in the Report to the American Academy of Neurology and the American Clinical Neurophysiology Society
4 to evaluate conclusions drawn from the evidence cited above.
Procedures
The general procedures used in the special report required eight major categories to be considered in evaluating a procedure. Those issues are listed below and the body of relevant QEEG evidence summarized for each one:
1.
Disease studied is clearly defined. This criterion is definitively satisfied by the general use of DSM classification in the majority of recent studies cited herein.
2.
Criteria for test abnormality defined explicitly, clearly, and prospectively. The criteria for QEEG test abnormality are defined by parametric statistical methods and are satisfied in the majority of recent studies cited.
3.
Control groups not included in normative groups. Almost all of the recent studies cited compared patients with independent control groups.
4.
Same degree of severity in study as in probable use. Many of the studies cited used patients categorized as early onset or mildly impaired, compatible with probable clinical utilization of these methods.
5.
Test-retest reliability high. Numerous studies of large samples of normal or clinical groups attest to high test-retest reliability.
6.
Sensitivity, specificity, positive predictive value, negative predictive value demonstrated. Requirement of a replicated finding significant at the P<0.05 level provides an expected specificity of about 95%. Sensitivities range from 60% to 95% in the reports cited here, depending on the disorder.
7.
Validity compared with other tests for same difference diagnosis. No biological tests have been validated for the psychiatric disorders discussed herein. Although MRI and CT have high specificity, they are not definitively sensitive even in mild dementia or mild head injury.
8.
Medical efficacy tests reduce morbidity by clarifying best intervention, clarifying diagnosis, giving more accurate prognosis, and providing a less risky substitute for previous method. Present treatments of the conditions of major concern discussed herein are symptom-based, diagnoses are empirical, prognosis is probabilistic, and treatment is selected by trial and error. In view of the absence of existing methods that offer objective biological adjuncts to diagnosis, selection of treatment, or accurate predictive value, QEEG methods offer improved efficacy of patient management and decrease the risk of ineffectual treatment or misdiagnosis.
Quality of Evidence Ratings
Class I:
Evidence provided by one or more well-designed, prospective, blinded, controlled clinical studies.
Class II:
Evidence provided by one or more well-designed clinical studies, such as case control or cohort studies.
Class III:
Evidence provided by expert opinion, nonrandomized historical controls, or case reports of one or more.
Strength of Recommendation Ratings
Type A:
Strong positive recommendation, based on Class I evidence or overwhelming Class II evidence.
Type B:
Positive recommendation, based on Class II evidence.
Type C:
Positive recommendation, based on strong consensus of Class III evidence.
Type D:
Negative recommendation, based on inconclusive or conflicting Class II evidence.
Type E:
Negative recommendation, based on evidence of ineffectiveness or lack of efficacy.
Recommendations
The special article that presents the opinions of joint committees of the American Academy of Neurology and the American Clinical Neurophysiology Society
4 concluded that QEEG might be a useful adjunct in the evaluation of patients with symptoms of cerebrovascular disease or dementia, making Type B recommendations (positive, based on Class II evidence provided by one or more well-designed clinical studies) for such use of QEEG. The special article further concluded that QEEG remains investigational for clinical use in postconcussion syndrome or mild head injury, learning disability, attention disorders, schizophrenia, depression, alcoholism, and drug abuse, with a Type D recommendation (negative, based on inconclusive or conflicting Class II evidence).
Basing our judgment on the prescribed procedures and adopting the rating scales used in that special article, we believe that the studies summarized in this review adequately justify the assessments of the utility of QEEG in the major categories of illness that follow:
Cerebrovascular Disease:
On the basis of many concordant Class II studies, Type B recommendation.
Dementia:
On the basis of multiple Class I and many concordant Class II studies, Type A recommendation.
Learning and Attention Disorders:
On the basis of multiple Class II studies and abundant Class II evidence, Type B recommendation.
Mood Disorders:
On the basis of multiple Class II studies, Type B recommendation.
Postconcussion Syndrome:
On the basis of several Class II studies and multiple concordant Class III studies, Type C recommendation.
Schizophrenia:
On the basis of conflicting Class II and III evidence, Type D recommendation.
Substance Abuse:
On the basis of conflicting Class II and III evidence, Type D recommendation.
Clinical Implications
In view of the accumulation of positive findings surveyed in this article, more psychiatrists may wish to explore the utility of these methods for themselves and begin to apply them in their clinical practice. EEG, first clinically applied in 1929 by the neuropsychiatrist Hans Berger,
258 promises to have greatly expanded use as psychiatrists become more familiar with its many applications.