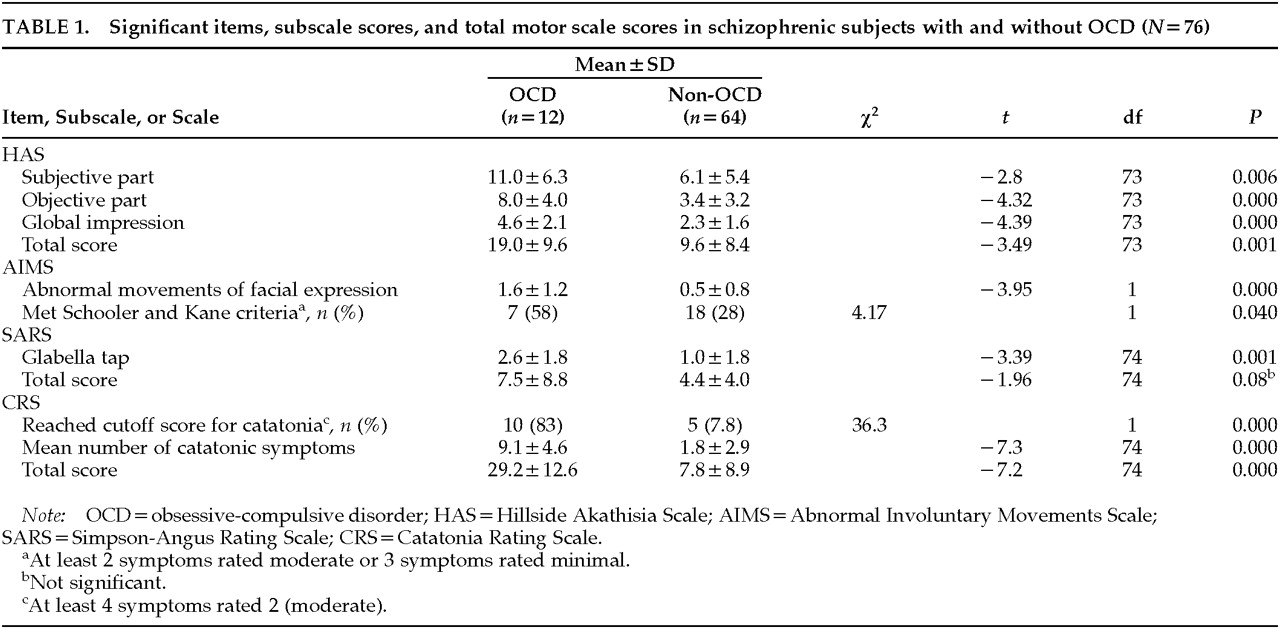
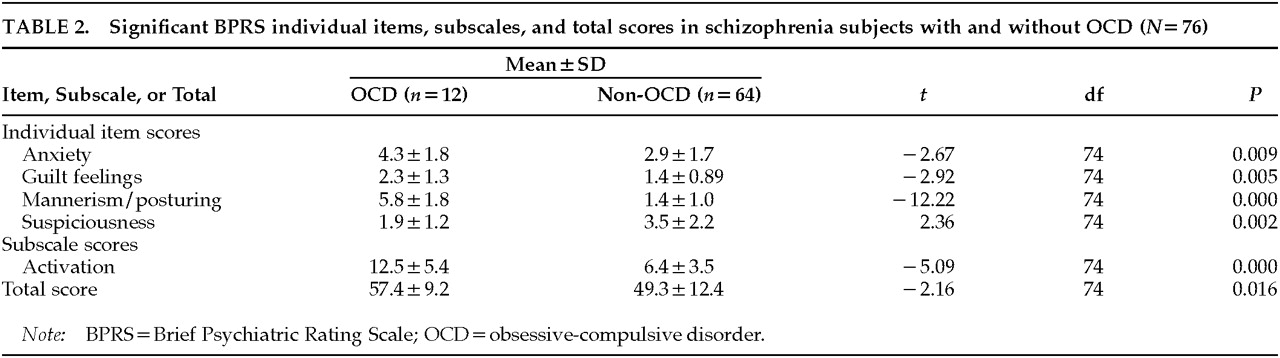
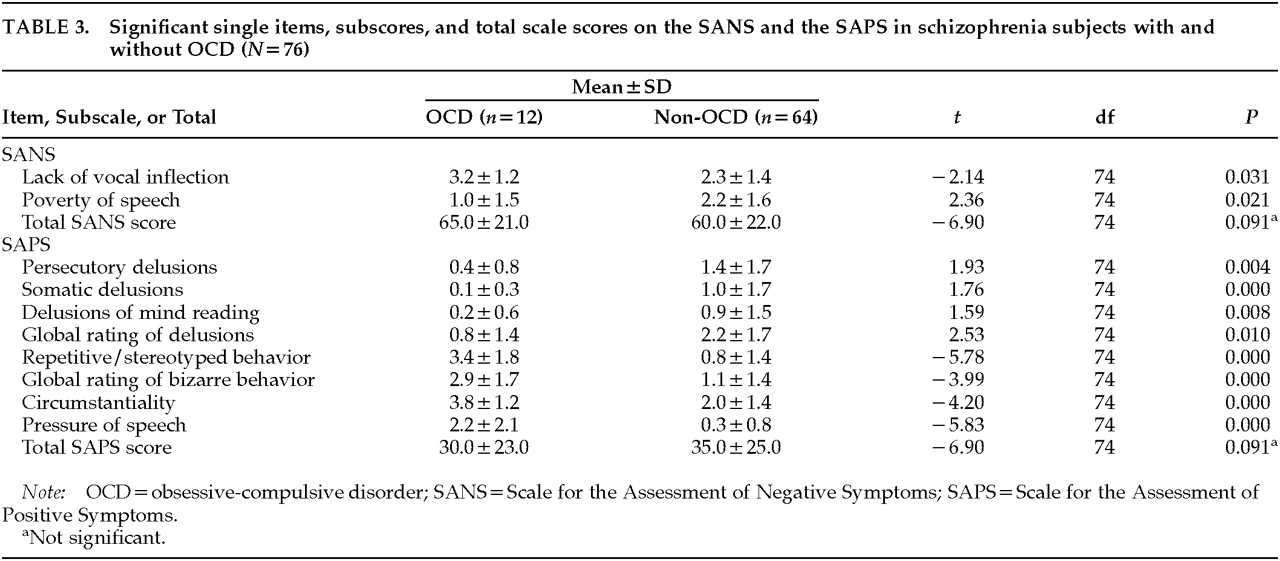
A major finding in the present study was the high frequency of motor symptoms in the schizophrenic subjects with OCD. This finding supports our central hypothesis. All subjects had been exposed to neuroleptics and other psychotropic medications, but our analysis was corrected for medication exposure and confirmed that the presence of OCD in schizophrenia was strongly associated with motor symptoms. Although the prevalence of extrapyramidal symptoms was not different in the two groups, schizophrenic subjects with OCD had significantly more severe akathisia and more abnormal involuntary movements than their non-OCD counterparts. The pathogenesis of akathisia and abnormal involuntary movements is not clear, and neuroleptic exposure seems to be only one of the factors contributing to their manifestation.
46–54 From our findings, it seems likely that schizophrenic patients with OCD are particularly vulnerable to developing both medication-induced neurological motor side effects and medication-unrelated motor symptoms. The high frequency of catatonia in the schizophrenic subjects with OCD confirms clinical observations by authors from the pre-neuroleptic era.
3,4The finding that motor symptoms are a defining feature of schizophrenia with OCD strengthens an emerging connection between OCD, schizophrenia, and motor disorders. There is much direct and indirect evidence pointing to involvement of the frontal lobe and the basal ganglia in the pathophysiology of both schizophrenia and OCD.
55–60OCD has significant associations with a variety of motor symptoms, including stereotypies, grimacing, twitching, catatonia, and tics.
21,22,30 There is also evidence in the literature that obsessional slowness, which is characterized by loss of motor fluency, hesitancy of limb movements, speech and gait abnormalities, cogwheel rigidity, complex repetitive movements, and tics and is seen in a subset of patients with OCD, may actually represent a different subtype of OCD.
61–63 The clinical description of the symptoms of obsessional slowness overlaps with symptoms of catatonia; however, their relationship has not been explored yet. Conversely, several extrapyramidal motor disorders, most frequently Huntington's disease, tic disorders, distortion dystonia, Tourette's syndrome, and Parkinson's disease,
22–30 are known to manifest symptoms of OCD.
29 It has been suggested that the links between these disorders and OCD include anatomical and biochemical lesions affecting primarily the basal ganglia and their connections with cerebral regions controlling the frontal lobe and other higher cortical centers.
24,64The involvement of the basal ganglia in catatonia is not fully explored;
65,66 however, the symptomatological spectrum of catatonia shows resemblance to the symptoms of extrapyramidal movement disorders.
65 There is also evidence from neuroimaging studies pointing to structural abnormalities in the basal ganglia
67 and of a basal ganglia regional glucose metabolism asymmetry during catatonic episodes.
68 Furthermore, it has been suggested that the efficacy of benzodiazepines in the treatment of catatonia is mediated by potentiation of GABAergic transmission in the basal ganglia.
69 Thus, it appears that at least some catatonic symptoms are linked to a dysfunction or abnormality in the basal ganglia. Further studies should identify those catatonic symptoms that are caused by basal ganglia dysfunction.