Denial is a common feature of addictive disease. Patients with alcohol dependence often underestimate the amount of alcohol they consume, the duration of their drinking problem, or the impact alcohol has had on their personal life or health. They are likely to overestimate their ability to control their drinking or to quit without assistance. In some cases, their perceptions go against compelling evidence of the severity of their problem. For some, the denial is fragile and is easily penetrated when they are supportively confronted with the facts. (e.g., liver disease, drunk driving arrests, repeated detoxifications). For others, the denial is fixed and is unaffected by confrontation with the evidence.
Addiction denial is usually considered in psychodynamic terms, as an unconscious ego defense mechanism. It is held that to fully acknowledge addiction-related problems would be so threatening to the individual's ego that he or she must misconstrue, reinterpret, or even forget the facts of the case. The central feature of this interpretation is that the denial is based on emotional rejection of the truth, rather than a simple failure of insight.
We propose that alcoholic denial is sometimes more of a cognitive failure than an ego defense mechanism. This cognitive failure may consist of diminished capacity for insight, or it may be an inability to integrate readily available information so as to draw an obvious conclusion. It may involve an inability to develop an organized, systematic approach for searching memory and for searching the environment for evidence of alcoholism, as well as poor discrimination of relevant from nonrelevant evidence. It may be influenced by mental rigidity, concreteness of thought, and poor ability to deal with complexity. Such cognitive deficits are common in alcoholics (for reviews, see Tarter and Edwards,
1 Grant,
2 Oscar-Berman and Hutner,
3 and Charness.
4)
Undoubtedly, the denial displayed by individuals with alcohol and other drug dependencies sometimes has a defensive component. However, a pattern of severe denial in the face of overwhelming evidence of addiction and addiction-related problems is also consistent with a cognitive defect.
If alcoholic denial is predominantly an ego defense mechanism, one would not expect those with severe, fixed denial to do more poorly on neuropsychological measures than patients with no denial or patients whose denial is easily penetrated and resolved. On the other hand, if fixed denial is a product of cognitive dysfunction, one might expect it to be related to more general cognitive dysfunction. Compared with alcoholics displaying little or no denial, those with fixed denial would be expected to perform more poorly on tests of reasoning, memory, concentration, mental flexibility, and general neuropsychological function.
METHODS
Design
The denial data were calculated from treatment plan information in the medical records of alcohol-dependent inpatients in a substance abuse rehabilitation program. The cognitive functioning data were drawn from records of neuropsychological tests results. All specific hypotheses, measures, and criteria for inclusion and exclusion were specified prior to chart reviews. Because the study was restricted to analysis of medical records, the hospital Human Studies Committee waived the informed consent requirement.
Subjects
We studied the records of 32 male and 12 female alcohol-dependent hospitalized inpatients, who were referred for routine neuropsychological evaluation. Of the 44 patients, 10 reported concomitant, secondary use of other drugs, including cocaine (3 subjects), marijuana (3), marijuana and cocaine (1), benzodiazepines (1), and multiple drugs (2 subjects). Patients were omitted from the study if their primary drug was not alcohol, or if substantial treatment plan data or neuropsychological data were missing. Brain damage unrelated to alcohol was not an exclusion criterion because we hypothesized that cognitive dysfunction, regardless of its etiology, would be found in cases of severe denial more often than in cases with little or no denial. The first 44 cases with adequate data were selected from an alphabetized list by the neuropsychologist, who was blind to the denial status of the patients.
Assessment of Denial
During the patients' treatment, an interdisciplinary team of addiction specialists assessed each subject as to whether denial was present. If it was present, they instituted denial-related treatment goals that were selected from a standard list of denial treatment goals (e.g., patient to list her or her own signs and symptoms of alcoholism, list problems caused by the drinking, list differences between his or her drinking and normal drinking). The treatment team then performed a weekly tally of the number of denial-related treatment goals that had been achieved and the number that remained unachieved. The denial measure used for this investigation was the percentage of the patient's denial-related treatment goals that remained unachieved at the time of discharge. Patients with no denial-related treatment goals were coded as having 0% of their denial-related goals remaining unachieved at the time of discharge (i.e., their denial was apparently either absent or resolved prior to admission to the treatment program). Thus, the denial scores were based on countable, operationalized criteria, rather than being simple opinions or global generalizations about the patient. Additionally, the clinicians whose findings were used as data were unaware that the data would be used in a study and were naive to the hypotheses explored by this study.
Assessment of Cognitive Status
The neuropsychological tests were selected and administered by a neuropsychologist (W.R.) on an individualized clinical basis.
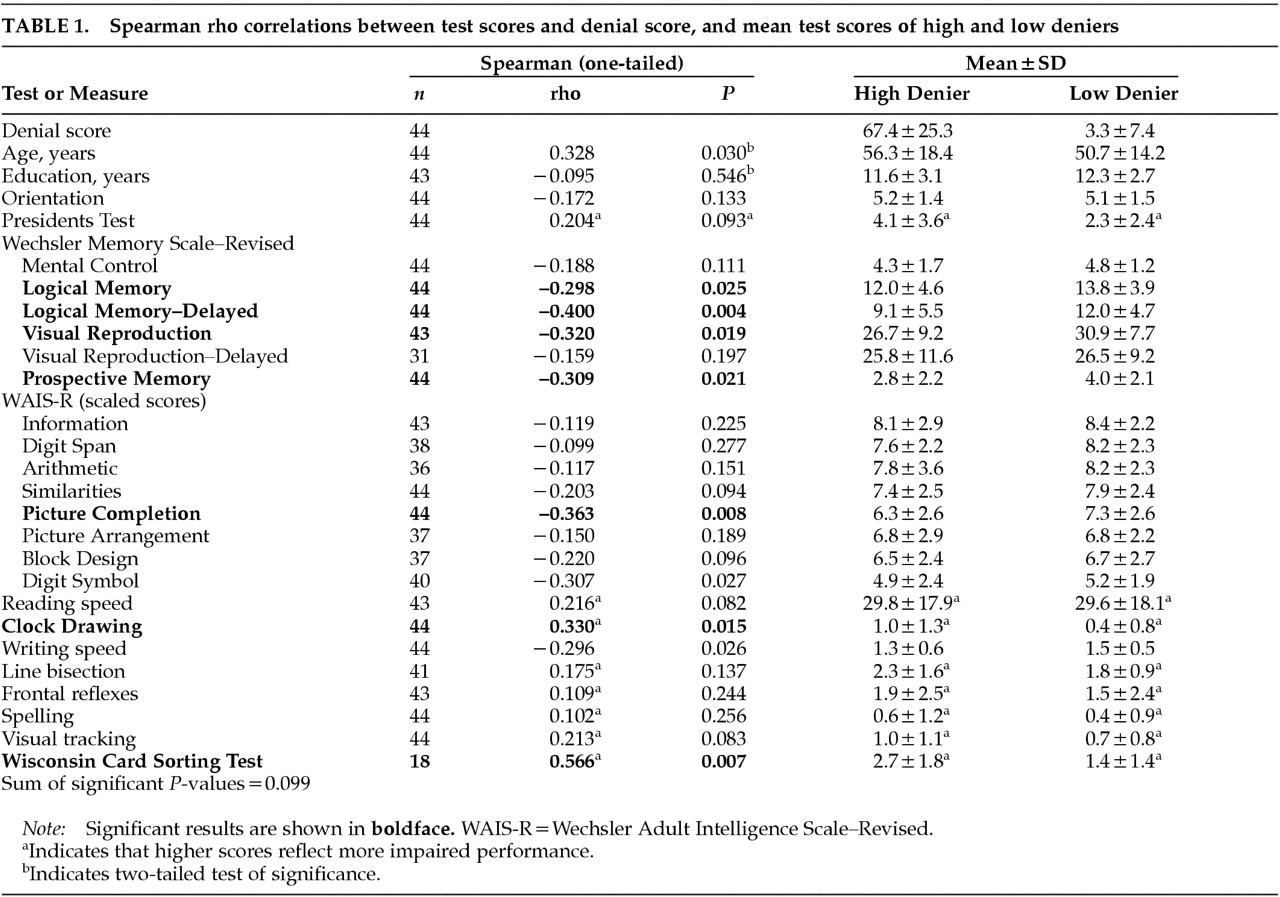
Table 1 lists the tests for which data were present for most of the subjects. All tests were administered in an identical fashion to each subject. The neuropsychologist was not included in the treatment team and did not participate in the assessment of denial. Orientation was scored 2 points for each correct age, place, and date, and 1 point for each near miss. The Presidents test
5 was limited to the Verbal Sequencing procedure. The score is the weighted number of sequence errors. The Prospective Memory test
6 consisted of remembering to do three things during the course of the exam, either on a cue or at a prespecified time. Each task could receive a score between 0 and 2. Reading speed was measured as the elapsed time to read a 56-word paragraph from the Alcoholics Anonymous Big Book.
7 Clock Drawing was administered and scored according to criteria adapted from Benjamin.
8 Scores could range from 0 (normal) to 3 (severe). Writing speed was scored as the number of letters per second writing the phrase “He shouted the warning,” from the Reitan Aphasia Screening Test.
9 Spelling evaluation was based on the above task, and scores could range from 0 (normal) to 3 (severely impaired). The Line Bisection score was the subject's average amount of error in bisecting each of 10 standard horizontal lines and was expressed as a percentage of the line's length. The Frontal Release Reflexes
10 score consisted of rating a snout reflex and a palmomental reflex on a scale between 0 (absent, normal) and 3 (sharp). The score reported is averaged across both the snout and the palmomental and across both sides of the body. The Wisconsin Card Sorting Test
11 was administered with a nontraditional protocol. Subjects were required to use trial and error logic to sort cards according to a concept (color, shape, or number) that was not revealed to them, except that they were advised of the correctness or incorrectness of their response after each trial. After each series of 10 trials in which a patient had not mastered the task, the level of structure was increased according to a standardized protocol, first by describing the three possible sorting criteria (color, shape, or number), then by correcting their incorrect responses, and finally by telling them what the correct sorting criterion is. The amount of structure can vary between 0 (no structure needed) and 5 (the subject makes errors even when explicitly told the correct sorting criterion).
Data Analysis
Because of a highly skewed distribution on the denial measure, we conservatively selected nonparametric statistical tests (Spearman rho correlations) to analyze the findings. Since there was a clear directional expectation to our working hypothesis (i.e., that persistent denial would be associated with worse test performance), most of the correlation coefficients were assessed with one-tailed tests of significance. However, since we had no
a priori hypothesis about the relationship between denial and the demographic variables of age and education, these correlations were evaluated with two-tailed tests of significance. To adjust for multiple correlation coefficients, we employed a conservative alpha level of 0.025, based on Dunn's test.
12 Seven correlations remain statistically significant at this level. The sum of the probabilities associated with these 7 correlations is 0.099, which is an acceptable experiment-wide error rate. For illustrative purposes,
Table 1 also shows the mean test scores for “high deniers” vs. “low deniers,” based on a median split of the subjects by their denial scores.
RESULTS
The number of denial-related treatment goals assigned to the subjects on intake varied from 0 to 20. The actual Denial scores (i.e., the percentage of these goals that remained unachieved at discharge) varied from 100 (i.e., 100% of the denial-related treatment goals still unachieved at discharge) to 0 (no denial present or no denial-related treatment goals remaining unachieved at discharge). The distribution of this variable was highly asymmetric. Fully 18 of the 44 subjects had Denial scores of zero, and 14 of these were by virtue of having no denial-related treatment goals to begin with.
Denial was not significantly associated with years of education. Denial scores were higher for females (mean=54.5) than for males (mean=28.2), but the difference was only marginally significant (Mann-Whitney U=120, P=0.049). A marginally significant correlation was also found between age and denial (rho=0.328, P=0.030), such that older subjects were higher in denial. However, using a median split on denial scores, high-denial subjects (mean age=56.3) were not significantly older than low denial subjects (mean age=50.7; t=−1.137, one-tailed P=0.131).
For all 24 tests studied, the correlation with denial was in the predicted direction (i.e., higher denial being associated with poorer test performance). The correlations achieved statistical significance for 7 of the 24 tests (presented in bold print in
Table 1). The memory measures Logical Memory, Logical Memory–Delayed, Visual Reproduction, and Prospective Memory were significantly correlated with denial, such that poorer performance was related to higher denial. Poorer performance on two measures of planning, problem solving, and general adaptive ability (Wisconsin Card Sorting Test and Clock Drawing) were significantly related to higher denial. Poorer performance on the Picture Completion subtest of the WAIS-R was significantly correlated with persistent denial. Marginally significant correlations with denial were obtained on two measures of mental speed, the Writing Speed measure and the Digit Symbol Substitution subtest of the WAIS-R (
P>0.025, <0.05). In both cases, slower performance was associated with higher denial.
DISCUSSION
Overall, the hypothesis of an association of denial with relative cognitive impairment was confirmed. Persistent denial was associated with poorer verbal memory, poorer executive functions, poorer visual inference, and mental slowness. This pattern of compromised functions could be expected to facilitate denial and to interfere with its resolution through treatment.
In particular, poor performance on the Wisconsin Card Sorting Test implies poor ability to modify one's way of approaching a problem in response to repeated experience and poor ability to identify and use a concept after being shown multiple examples of the concept. An individual with such deficits might have difficulty altering something as stable as his or her self-concept to come to the counterintuitive conclusion that he or she is alcoholic. Compromised verbal memory would make it difficult to gather and integrate all the evidence necessary to make a rational judgment about the severity of the drinking problem. Poor clock drawing and poor prospective memory suggest planning and organizing skills insufficient to organize a systematic investigation of the possibility that one's drinking is abnormal. Poor performance on the Picture Completion test also suggests compromised ability to draw logical inferences from readily available information. This is a central feature of fixed denial.
There are a number of interesting parallels between severe alcoholic denial and “anosognosic” denial,
13 such as denial of hemiplegia after stroke. Anosognosia has more recently been described in connection with unawareness of deficits such as hemiblindness, amnesia, dementia, and receptive aphasia.
14–19 It is now characterized more commonly as a failure of a brain mechanism that monitors the adequacy of one's behavior, for example comparing the actual consequences of one's actions with the intended or expected consequences.
20–22 More broadly, it has been characterized as a failure to discover a defect,
23,24 that is, failure to systematically gather, integrate, and retain the relevant information, or failure to make use of the information to draw an obvious conclusion (i.e., that one is paralyzed, blind, etc.). These characterizations are also descriptive of fixed denial of alcoholism. Both types of denial appear to be associated with impaired executive function. The cognitive deficits attendant to either type are predominantly nonverbal and somewhat difficult to detect without formal neuropsychological testing. Both types present severe obstacles to effective treatment.
The findings have significant implications for treatment. A common approach to treating denial is massive confrontation of the patient with convincing evidence from multiple sources (e.g., spouse, children, doctor). This approach will probably be ineffective in cases of anosognosic denial and may be counterproductive. The cognitively compromised client will not be able to integrate such a volume of information, may experience confusion, and may become increasingly rigid in his or her position. Effective treatment of anosognosic denial will require a much more structured and paced approach, in which information is presented in small, manageable chunks and reinforced before more information is presented.
This study has certain limitations that should be noted, especially for future research on this topic. Because the findings are based on study of participants in an inpatient addiction treatment program who had been referred for neuropsychological testing, the findings may not generalize to less severely afflicted alcoholics. However, the measured neuropsychological differences between high-denial and low-denial subjects cannot be explained as an artifact of selection bias. That is, if all subjects had presumptive brain damage, this would restrict the chances of finding more brain damage in those with persistent denial and would make the obtained differences more difficult to achieve.
Additionally, the obtained correlations between denial and cognitive status may have been lower because the two measures were taken at slightly different points in time. Denial and cognitive impairment both tend to change over the course of treatment. Thus, cognitive impairments measured six days after admission may not correlate highly with denial measured at discharge two weeks later. The fact that significant correlations were obtained despite these obstacles suggests a strong underlying effect of cognitive dysfunction on denial, but more or less simultaneous measurements would be better in future investigations.
Subjects' age may have had an influence on the current findings, such that older subjects tended to be more cognitively impaired and higher in denial. This does not appear to be a strong effect, but it should be monitored in future investigations.
It should also be noted that the denial measure employed in this study equates severity of denial with tenacity of denial. That is, the severity of denial is measured only by the degree to which it failed to resolve over the course of treatment. We did not assess whether the initial severity of the denial correlated with cognitive deficits. We do not know whether resolution of cognitive deficiencies correlates with resolution of denial. These questions invite further exploration.
Better identification of these organically compromised patients and use of a better informed treatment approach could have widespread positive consequences. Given the prevalence of neuropsychological impairment among chronic alcoholics, and given the implications of those impairments for denial, increased utilization of neuropsychological assessment is indicated, particularly in cases of severe denial. Further investigation of the neuropsychological determinants of denial is also clearly indicated.
ACKNOWLEDGMENTS
The authors thank Cary Savage, Ph.D., for his assistance in statistical analysis and manuscript preparation. This work was supported by National Institute on Drug Abuse Grants R01-DA08781 and K24-DA00427 to Dr. Gastfriend.