Hoffman et al.
1,2 recently reported beneficial effects of low-frequency TMS of left temporoparietal cortex in medication-resistant hallucinating patients. In the first study, patients were stimulated during 4 days with TMS. (The mean duration of stimulation was 10 minutes daily.) All three patients demonstrated considerable improvement in hallucination severity as rated on a visual analog scale after the 4-day period. In the second study,
2 12 medication-resistant hallucinating patients with schizophrenia were treated with TMS, and again active stimulation reduced ratings of hallucination severity relative to sham stimulation. Four patients could be classified as nonresponders because they did not improve or the improvement was negligible.
The rationale of Hoffman and co-workers
1,2 for stimulating left temporoparietal regions in their TMS studies originated from the hypothesis that brain regions underlying speech perception contribute to auditory hallucinations. However, although there is some evidence for the involvement of left temporoparietal cortex in hallucinations,
3 most brain imaging studies of hallucinating patients indicate the auditory cortex (middle and superior temporal gyri) to be mainly involved in the experience of auditory hallucinations.
3–5 Therefore, in this study we investigated whether TMS at the auditory cortex would improve severity of hallucinations. We stimulated for a longer period, 2 weeks, and included a standardized hallucination rating scale. We also evaluated the effect of low-frequency TMS treatment on a wide range of neurocognitive functions.
METHODS
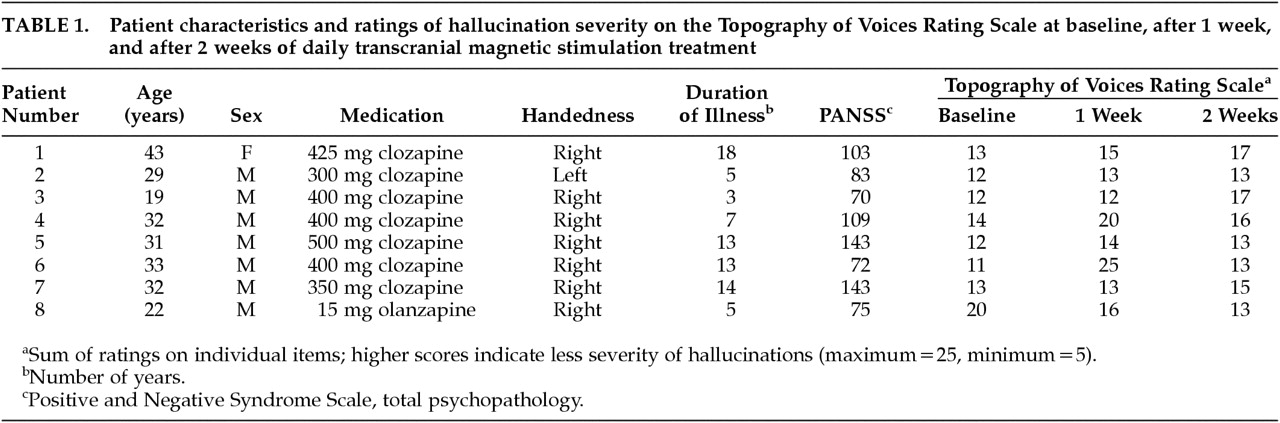
Nine medication-resistant patients with auditory hallucinations participated in the study after giving written informed consent. The study was approved by the medical committee of the University Medical Center–Utrecht. All patients had DSM-IV diagnoses of schizophrenia, as established with the Comprehensive Assessment of Symptoms and History (CASH). All patients had a stable medication status and used atypical antipsychotics. None of the patients received concomitant anticonvulsant drugs or benzodiazepines, which may reduce TMS effects. Further patient characteristics are given in
Table 1.
Patients were stimulated daily with TMS for 20 min during 2 weeks consecutively (only workdays; in total, 10 days) in an open trial. Stimulation was carried out with a Neopulse stimulator (Atlanta, GA, Neotonus, Inc.) at a frequency of 1 Hz and an intensity of 80% of the motor threshold. For one patient (Patient #1) the intensity was lower, approximately 50%, because of painful muscle contraction at higher intensities. The location of stimulation was approximately 2 cm above T
3 electrode position (International 10–20 System). The definition of this stimulation position was based on Talairach Atlas coordinates (coronal plane) in order to influence predominantly the superior temporal gyrus. At baseline, after 1 week, and at the end of the treatment, a standardized hallucination scale, the Topography of Voices Rating Scale,
6 was completed by each patient. This scale, which measures frequency, audibility, clarity, and affective response to auditory-verbal hallucinations, consists of 5 items that are rated on a 5-point scale by the patient. The author who carried out the stimulation (A.A.L.d'A.) was not involved in collecting the data.
Sensitive neuropsychological measures were included that were primarily aimed at auditory and verbal functions: an auditory imagery test
7 in which subjects were asked to mentally compare acoustic characteristics of everyday sounds; the Rey Auditory-Verbal Learning Test (verbal memory); the Token Test, short form (verbal comprehension); and tests of verbal fluency and phoneme detection. The following nonverbal measures were also included: Judgment of Line Orientation, Line Bisection Test, Benton Visual Retention Test, and the Test for Facial Recognition, short form. (For description of the neuropsychological tests, see Lezak.
8)
Nonparametric statistical analysis (Friedman's test) was performed in the analysis of hallucination ratings, because the measurement scale was ordinal.
RESULTS
One patient was excluded from the analysis because (he) discontinued medication, after which symptoms aggravated. Symptom ratings of the remaining 8 patients are listed in
Table 1. A significant effect of TMS treatment was observed on the Topography of Voices Rating Scale between baseline and the end of the treatment: χ
2=4.5, df=1,
P=0.034 (mean±SD: 13.4±2.8 at baseline, 14.6±1.8 at end of treatment). We also computed the corresponding effect size, which was
r=0.65. The difference between baseline and week 1 showed the same trend but failed to reach significance: χ
2=3.6, df=1,
P=0.070.
Of the neurocognitive measures, only the auditory imagery test revealed a significant performance difference: t=–2.6, df=5, P=0.046. For this test, baseline data were not available for two patients. Performance was significantly better at posttest (mean=17.7 correct out of 21) than at baseline (mean=15.3).
DISCUSSION
The present study was designed to investigate whether 2 weeks of daily 1-Hz transcranial magnetic stimulation of left auditory cortex would influence hallucination severity and neurocognition in medication-resistant hallucinating patients. A statistically significant effect was observed on hallucination severity ratings as measured with a standardized scale. Thus, our results are in accordance with the findings of Hoffman et al.,
1,2 who also reported beneficial effects of TMS on hallucinations in schizophrenia. However, in the present study, all patients still experienced hallucinations after the treatment. Indeed, considering that the location of stimulation was based on the weight of the neuroimaging evidence and that we stimulated for 20 minutes daily during 2 weeks, we had expected more promising results.
Examination of the individual data revealed that hallucination severity improved in 7 of 8 patients at week 2. In 5 patients this was an improvement of 2 points or more on the standardized scale. The fact that a few patients did not seem to respond substantially to TMS (and one actually deteriorated) is in accordance with the study by Hoffman and colleagues
2 in which 4 out of 12 patients were classified as nonresponders because they did not improve more than 1 point on a 10-point visual analog scale. We observed individual differences in the onset of the improvement, whereas a previous study
2 revealed large individual differences in the duration of the TMS effect. These data suggest that there may be a complex interaction between number of treatments, brain location of treatment, and improvement, differing from patient to patient, that deserves further exploration.
In the neurocognitive domain, only auditory imagery showed improvement after TMS treatment. Speculatively, the concurrent improvement of hallucination severity and auditory imagery may be seen as in accordance with theories that have implicated deficient imagery processes in hallucination. Alternatively, improvement on the imagery task may be attributable to a test-retest effect, although such effects would then also be expected on the other neurocognitive tests.
A limitation of this explorative study was the lack of a placebo-control group. Clearly, larger double-blind, placebo-controlled trials are needed before strong conclusions about TMS treatment of auditory hallucinations can be reached. To our knowledge, the present study is the first to use TMS in patients taking clozapine, demonstrating that TMS can safely be applied in conjunction with clozapine. Interestingly, all 7 patients on clozapine showed improvement on the voice rating scale, while the single patient on olanzapine showed worsening. This finding suggests that interactions may occur between type of medication and effectiveness of TMS, a possibility that should be studied in more detail. In addition, future research may evaluate the effect of TMS of the right hemisphere and compare TMS over medial-temporal sites with TMS over temporoparietal sites. Moreover, effects on hallucinations in other modalities may be explored.
An important finding of this study was that daily TMS stimulation during 2 weeks did not have adverse effects on cognitive functioning. This is especially important because TMS is known to be capable of transiently disrupting processing in brain areas. With regard to clinical safety, our results on cognitive function thus converge with recent MRI studies that indicate no structural brain changes in humans after high-dose repetitive TMS.
9ACKNOWLEDGMENTS
The authors thank Anke Jongen, Claudy Oomen, and Esther Caspers for their assistance in this study. The authors are grateful to Neotonus, Inc., for making the TMS equipment available. This work was presented at the third annual meeting of the International Society for Transcranial Magnetic Stimulation (ISTS), Chicago, IL, May 10, 2000.