The nation's academic health centers (AHCs) are currently faced with a developmental challenge of greater magnitude than in any period since the time of the Flexner Report in 1912.
1–4 The nature of this challenge is commonly framed in fiscal terms. The components of this crisis have been described as the result of reduced revenues for medical schools; the demise of fee-for-service practice reimbursements for physicians; the termination of cost-plus-reimbursement formulas for university hospitals; and the development of a variety of commercial competitive care delivery systems, collectively described as “managed care.”
5 In short, the AHCs of the 21st century are experiencing a rapidly changing, capital-based health care economy, for which they have employed 19
th century managerial and administrative structures.
6 Academic health centers face a marketplace in which adaptation to business fundamentals is vital. Elements of this adaptive change will vary from center to center, but almost certainly will include more open financial accountability, strengthened centralized governance, realistic business assessments of programs and projects, and the development of new organizational structures based more on mission than history.
In this paper, we describe one example of an actual management reorganization that can improve efficiency while enhancing core academic missions: the merging of traditional psychiatry and neurology departments into a single neuropsychiatry department.
There are good reasons to contemplate various merger forms between psychiatry and neurology within the nation's AHCs. Historically, psychiatrists and neurologists have studied and treated many similar disease syndromes, but they've done so from different perspectives of the mind and brain.
7–11 When the American Board of Psychiatry and Neurology was established in 1934, psychiatry and neurology decided to certify together, and they have remained together with considerable testing overlap to the present day.
12 More recently, integrated neuropsychiatric medical societies have formed (the American Neuropsychiatric Association and the British Neuropsychiatric Association), and neuropsychiatric journals have been founded (
The Journal of Neuropsychiatry and Clinical Neurosciences, and
Neuropsychiatry, Neuropsychology, and Behavioral Neurology). A number of neuropsychiatric books have appeared
13–15 as well as topical essays concerning the overlap of boundaries between neurology and psychiatry.
16–22 Philosophical arguments have been made for increased integration between the current separate medical specialties of neurology and psychiatry.
23,24 Arguments for such neuropsychiatric integration have been made from the realm of neuroscientific research.
25,26 Education for residents and medical students has been emphasized as a heuristic area for neuropsychiatric collaboration.
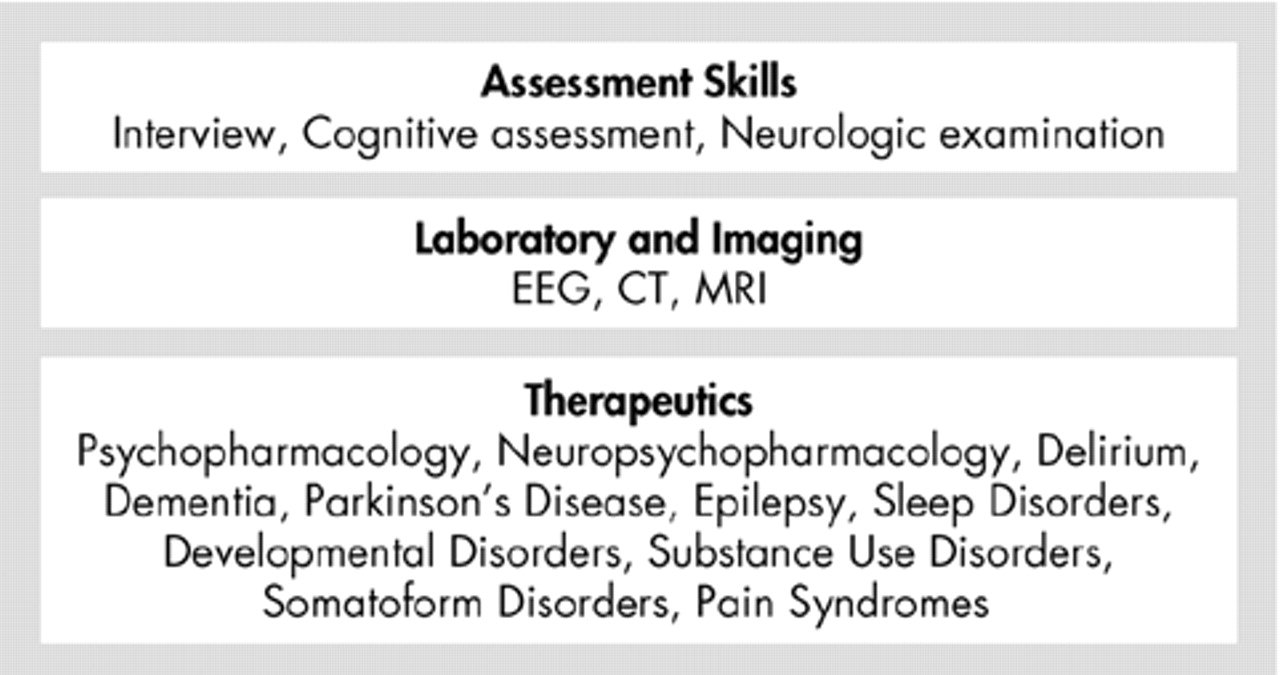
27–29 There are clinical domains of neuropsychiatric evaluation and treatment, which may be distinguishable from the practice patterns of general neurology and psychiatry.
30 A diagram of such a neuropsychiatric practice model is illustrated in
Figure 1.
In the midst of such discussion on the virtues of various parameters of neuropsychiatric integration, it may seem surprising that the business and management domains of neuropsychiatry have been omitted. During a period of reorganization at Texas Tech University Health Sciences Center (TTUHSC), we took the opportunity to develop and test a management model for neuropsychiatry.
NEUROPSYCHIATRY AS A MANAGEMENT MODEL
Basic science departments in the AHCs are presently undergoing far-reaching and widespread structural changes in the hopes of saving administrative expenses as well as achieving academic synergies.
31 These structural changes in administration are occurring in response to scientific advances and business pressures to create more efficient academic structures. We hypothesized that the historical, scientific, and clinical practice developments in neuropsychiatry described above should argue in favor of a similar reorganization between traditional clinical departments of neurology and psychiatry. Indeed, four medical schools in the United States presently have merged departments of psychiatry and neurology (Meharry University, the University of South Carolina, Tulane University, and the University of Missouri) (Association of Chairs of Academic Departments of Psychiatry; personal communications). The business performance characteristics of these merged departments have not, however, been reported. Inside AHCs, there are two types of managerial benefits that must accrue if a prospective merger is to be considered a successful business enterprise: administrative efficiencies from the merger, accruing from the combination of two departmental chair offices, and other administrative savings, depending upon the administrative structure of the integrated neuropsychiatry department.
We proposed to create a merged department model for neuropsychiatry and adapt the business structure of the new department to the business tasks of a 21st century academic department. We considered such a department to be a conglomerate business entity, with three product lines related to clinical care, education, and research. If the administrative structures of the department were recast according to these three product lines and personnel costs were reengineered in the administration of these product lines, we expected immediate merger related operational savings to accrue to the medical school. In addition, if the opinion papers regarding historical, scientific, educational, and practice links between neurology and psychiatry are correct, other positive benefits deriving from synergies should accrue to a neuropsychiatric departmental merger. Below, we describe the actual performance characteristics of this neuropsychiatric departmental merger at TTUHSC.
THE TEXAS TECH EXPERIMENT
The fiscal year at TTUHSC is from September 1 through August 31 of the subsequent year. The merger of the departments of psychiatry and neurology was ordered by the Office of the President at TTUHSC in early 1998, but operational planning did not begin until late in the 1999 fiscal year. The actual merger operational steps were implemented during the 2000 fiscal year.
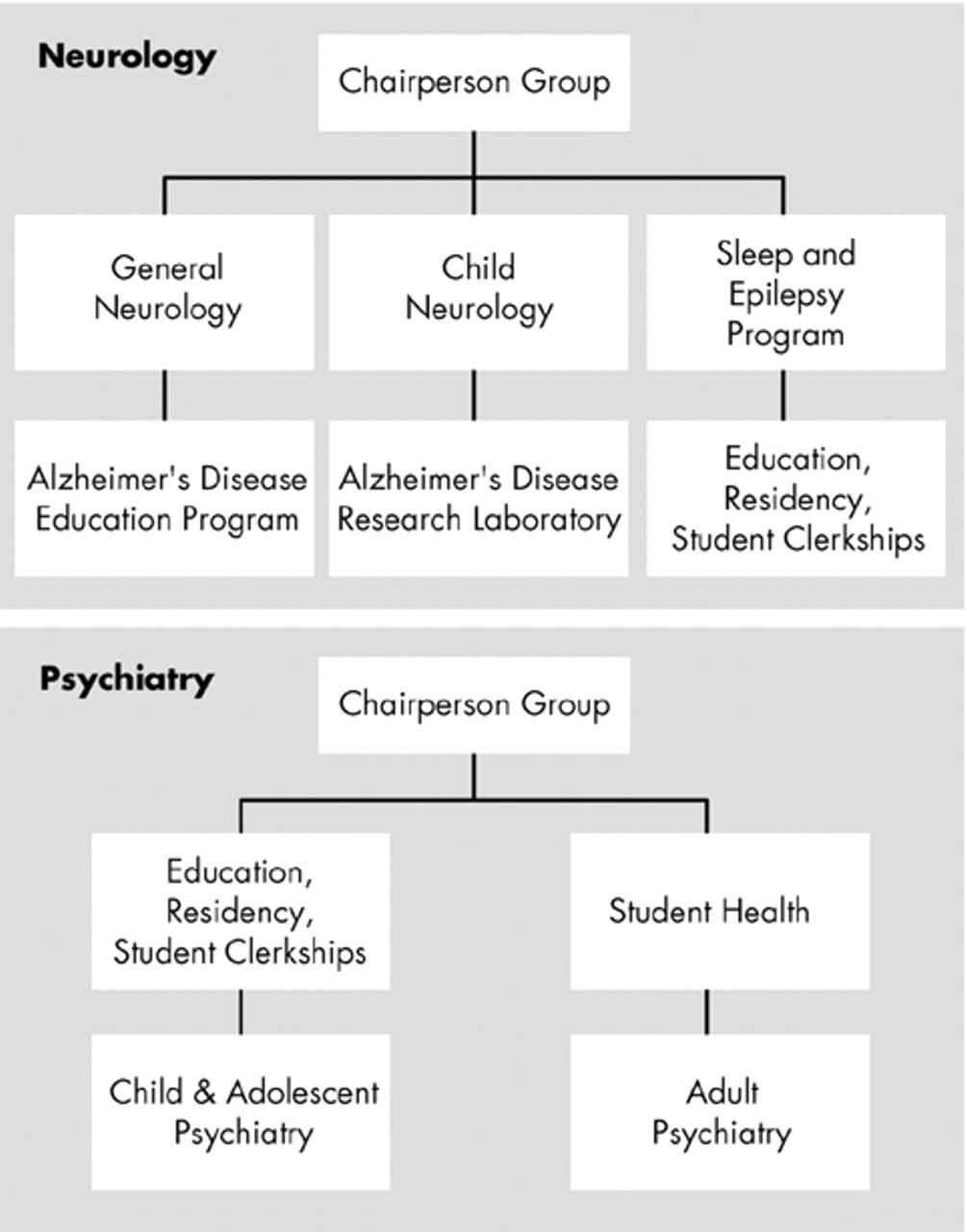
Prior to the 1998 merger of the neurology and psychiatry departments at TTUHSC, the neurology and psychiatry departments had the respective structures depicted in
Figure 2. Each box in the organizational diagrams represents a locus of financially supported physician-led management. This was a typical, early 20th century organizational structure, with administrative resources organized around academic territories, as opposed to product lines. Both departments had histories of recurring operational financial losses, which had become sources of friction between departmental and medical school leaderships.
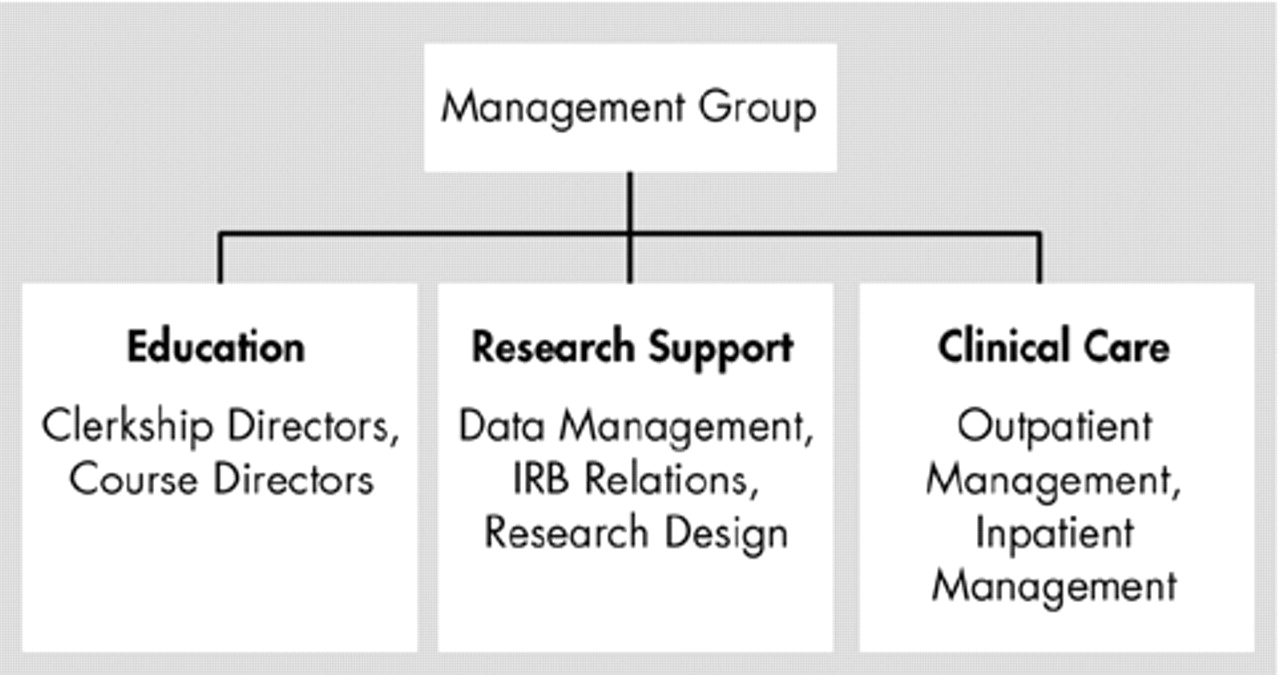
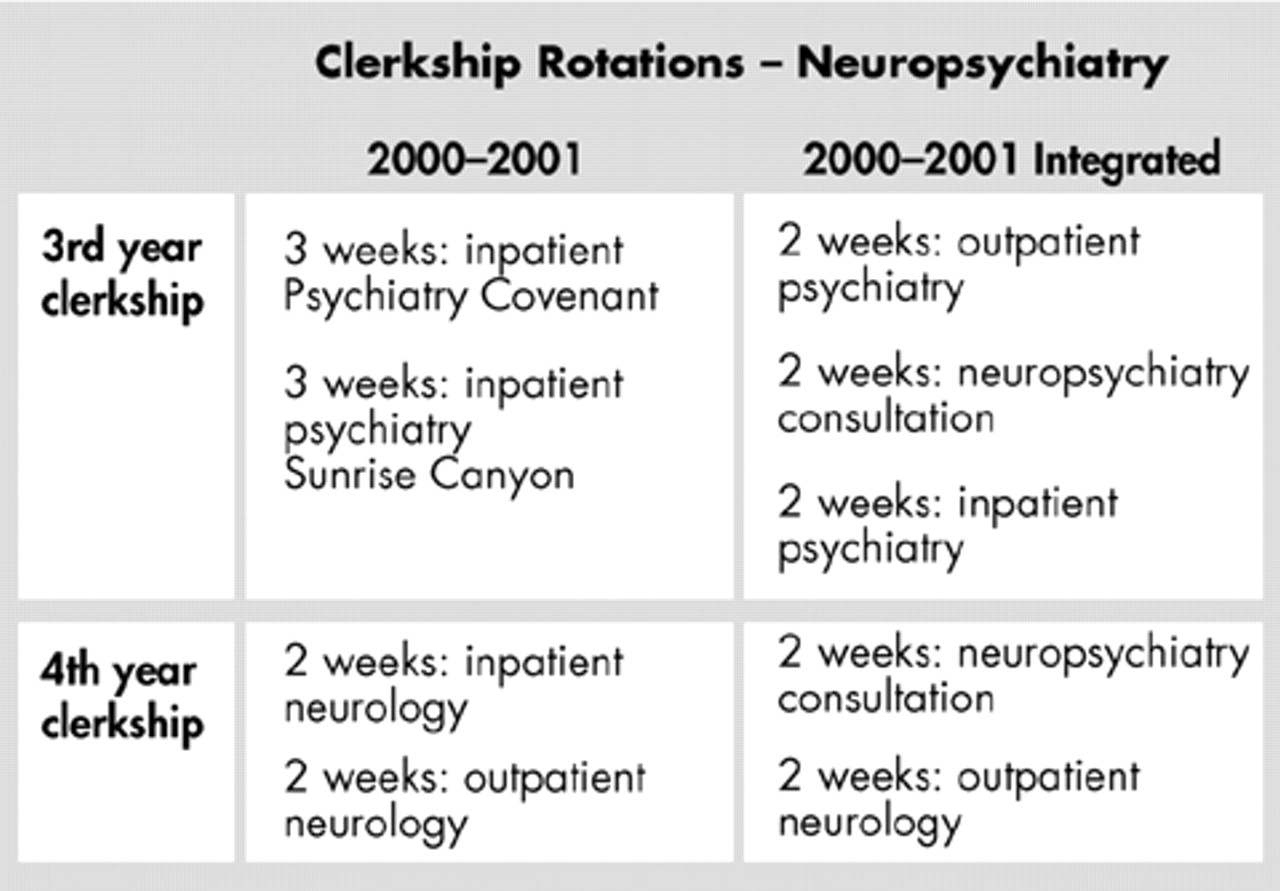
The merger and administrative reorganization which created a neuropsychiatry department were determined to commit administrative support services to the three major product lines only, and to conserve the use of physician faculty time for academic purposes (
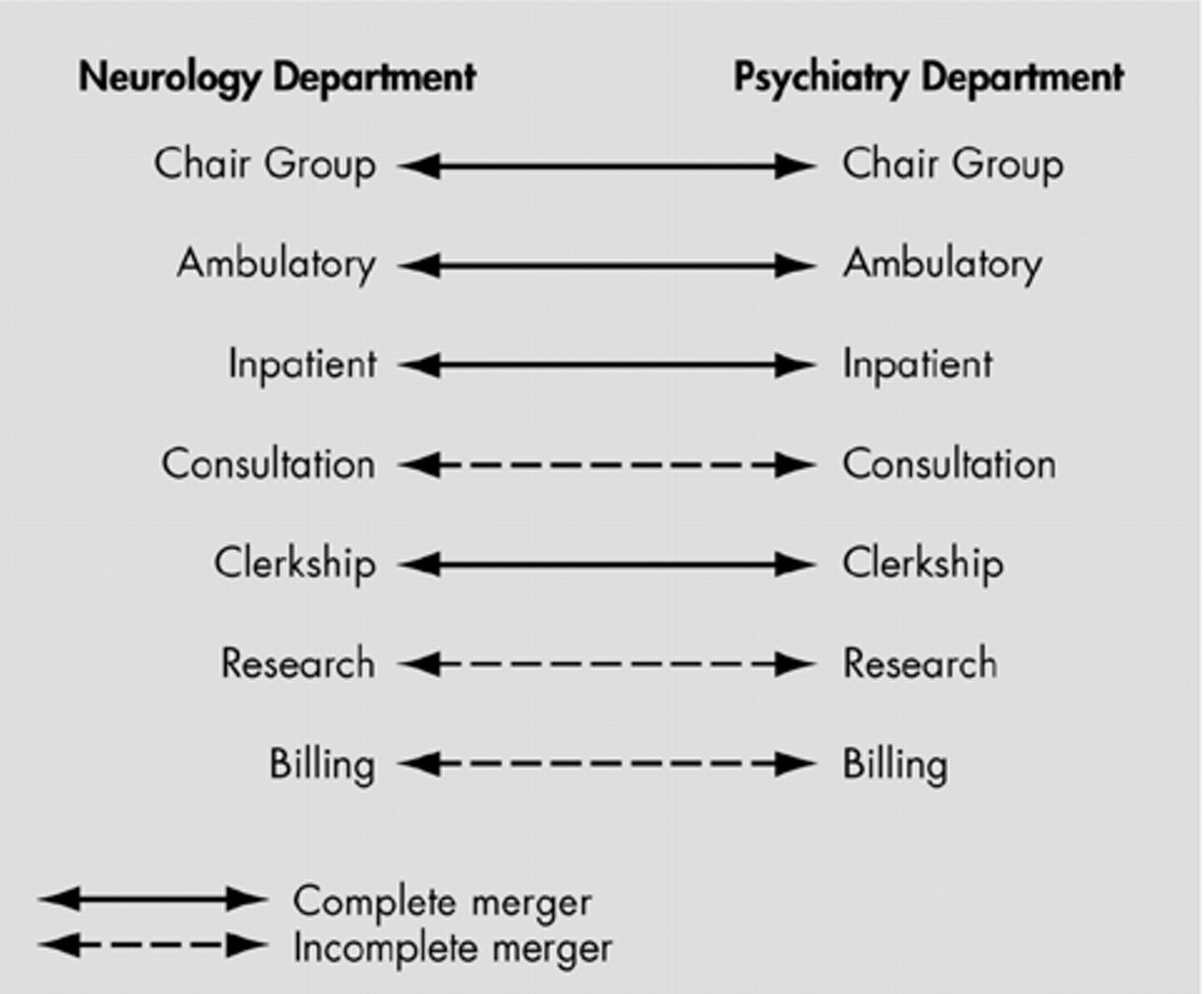
Figure 3). These structures were created in steps, using a merger formula (
Figure 4). First, we completely merged the chair administrative groups, the ambulatory management teams, and the medical student clerkship directorship. A “business week only” merger of the inpatient consultation services was accomplished next, leaving night and weekend coverage separated according to traditional mechanisms. Faculty administrative effort was explicitly relegated to residency and clerkship directorships only, in an attempt to allow faculty members time to perform research, clinical care, and actual educational endeavors. Ambulatory and research support administrative functions were packaged into new teams, composed of trained business administrative personnel and nurse clinicians. The separate neurology and psychiatry medical student clerkships were merged under the leadership of a single faculty member (
Figure 5). More than twenty full time faculty and staff departed or were separated from the departments during this process. Four of the faculty losses came from the former neurology department group, and four faculty departed from the psychiatry group.
RESULTS
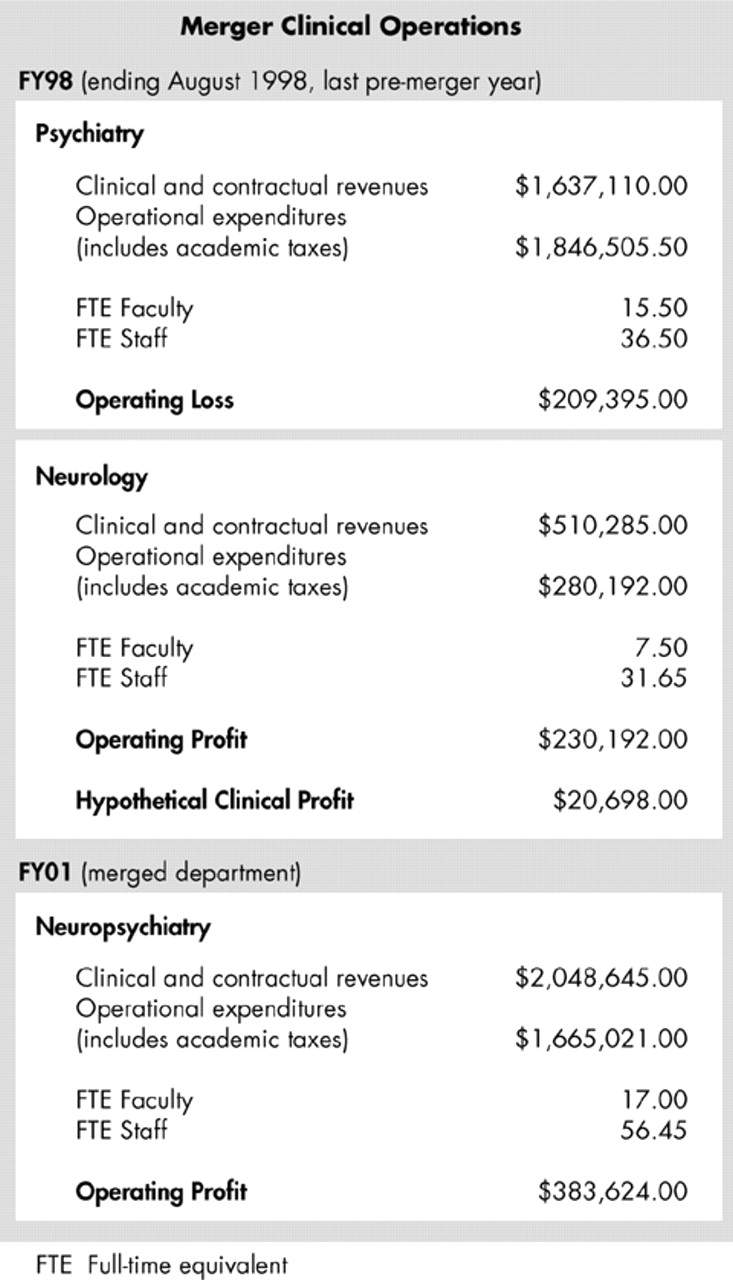
A before-and-after comparison of departmental clinical operational changes that can be attributed to the merger is illustrated in
Figure 6. The comparison data in
Figure 6 are for fiscal year 1998, the last full year before the merger began, and for fiscal year 2001, the first full year after substantial merger accomplishment. The data presented are for clinical operations only, not for research support, nor for state-based educational support.
Figure 6 illustrates that total clinical revenues remained essentially flat between the comparison fiscal years, at about 2.1 million dollars, but that significant operating efficiencies had accrued by fiscal year 2001. The merged department had changed two separate operations from a summed break-even performance to one generating operating profits of about $383,000.00 on an annual basis.
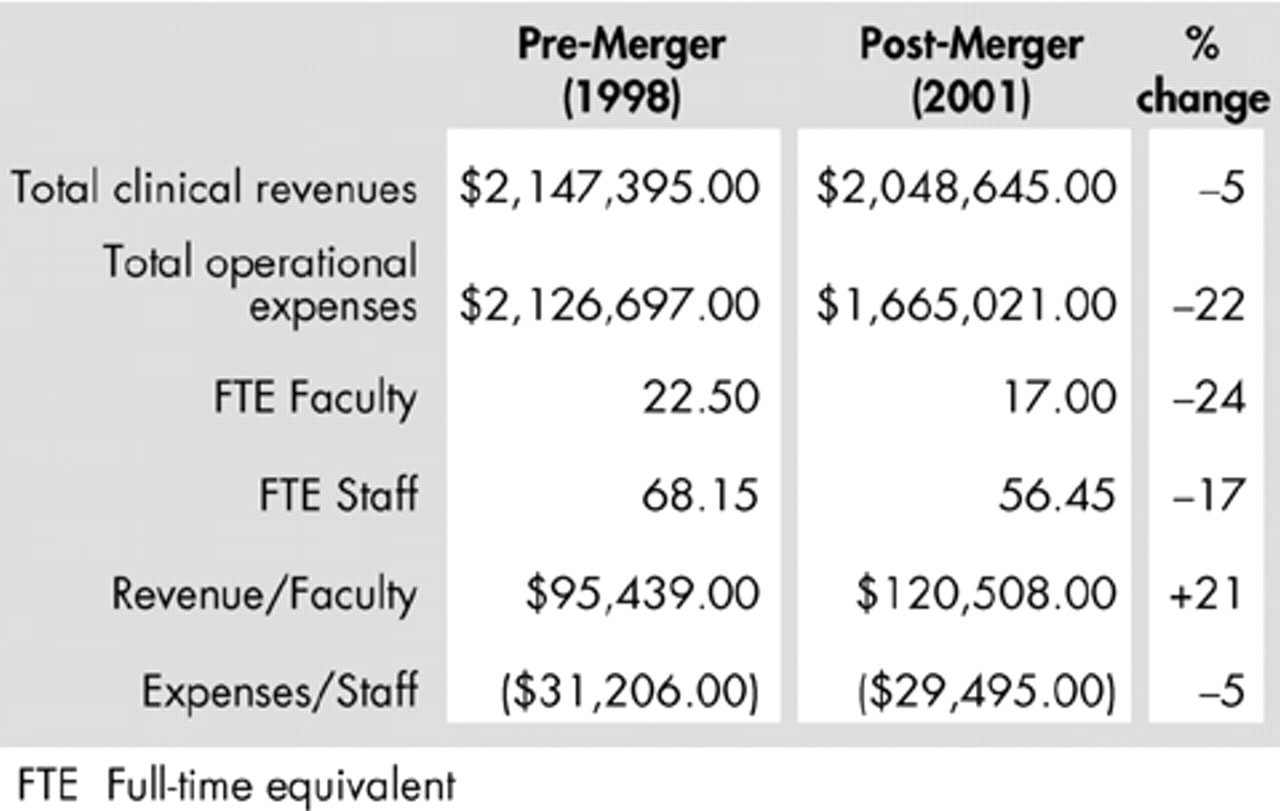
The operating efficiencies of the merger are depicted from the perspective of productivity ratios in
Figure 7. Fundamentally, the efficiencies of an academic restructuring are derived from savings in personnel costs from both the faculty and the staff. Personnel represent the primary operating costs of conducting business at the department level since many structural and overhead costs are performed at higher levels of administration such as the medical school. One can see from the numbers in
Figure 7 that essentially the same revenue and contract income were supported in the integrated neuropsychiatry department by significantly fewer faculty members and staff.
DISCUSSION
The creation of structural change within a conservative institution such as an AHC is not a simple matter. A number of faculty and staff left or were separated during the merger process. There is a limit to how far such changes can proceed within a 2-year period. For example, we have not attempted to merge or even significantly alter our general psychiatry inpatient unit, although this would be a natural site for continued integration. The merged department, however, seems to have a positive culture of its own, with high ratings on clerkship evaluations, high rates of faculty retention, and solid cash flows to support faculty development and other discretionary items.
It is also unclear to what extent the neuropsychiatry business model outlined in this paper can be exported to other AHCs in the United States. Each AHC is culturally different from others, in terms of its historical identity and extant business operating structures. Organizational change must respect these cultural differences in order to be effective. Additionally, a neuropsychiatric integration requires a substrate of neuropsychiatric faculty who are positive about neuropsychiatry and willing to try new ways of conducting department business. Three faculty members in the TTUHSC department are dually certified in adult neurology and adult psychiatry. Such neuropsychiatric faculty members presently available in the United States are limited.
Another limitation to this study is that it does not address the question of whether academic synergies have accompanied the neuropsychiatric merger at TTUHSC. These synergies would include hypothesized enhancements in the quality of educational and research programs in a neuropsychiatry department beyond financial savings attributable to expense reduction. Such synergies are more difficult to identify within usual and customary operating statements of academic departments and might be delayed at onset, when compared with the efficiencies described here. We hope to report on these academic synergies in a future paper.
ACKNOWLEDGMENTS
This study was conducted at Texas Tech University Health Sciences Center, Lubbock, Texas.