P rogress in the treatment of pediatric brain tumors has led to an increase in the number of children, adolescents, and young adults surviving free of neoplastic disease, but this increased survival has come at a price. Morbidity is high among survivors, both from consequences of the primary lesion and from the effects of the multimodal treatment on the developing brain. Surgery, radiation, and chemotherapeutic agents may produce both immediate and delayed injury to the CNS, and lead to profound clinical consequences in survivors.
Combined modality brain tumor treatment often results in chronic medical complications.
1 Survivors of pediatric brain tumors may suffer endocrinopathies, growth abnormalities, intellectual decline, neurocognitive and psychosocial dysfunction, and increased rates of anxiety, depression, dementia, and personality and behavioral disturbances.
2 Additionally, there is an increased actuarial risk for developing a second malignant neoplasm.
3Among all children successfully treated for cancer, survivors of CNS malignancies are more likely to have significant neurocognitive and neuropsychological sequelae, neurological impairment, and reduced quality of life.
1 The risk of psychiatric hospitalization is increased for survivors of brain tumors but not among survivors of other cancers in childhood or adolescence.
4 Children treated with only surgery and chemotherapy may not exhibit as significant a neuropsychiatric compromise as irradiated patients.
5 Tumor location, neurologic status at diagnosis, and surgical morbidity also affect long-term developmental and neurocognitive status. The greater severity of late neuropsychiatric effects in survivors of pediatric brain tumors has been primarily attributed to cranial radiation, with the magnitude of the impairment relative to radiation dose and age at treatment.
6Radiation may produce focal or diffuse white matter necrosis, myelin degeneration, glial cell change and proliferation, and microvascular changes leading to parenchymal hemorrhage and necrosis.
7 The degree of histopathological change may correlate with clinical findings and vary according to radiation dose, field, and time from treatment. The degree of direct CNS injury from radiotherapy appears to plateau 3 to 5 years from treatment. Late focal necrosis and progressive necrotizing leukoencephalopathy with necrosis, demyelination, and reactive gliosis can be seen years after initial treatment. Radionecrosis may present even later, with increased intracranial pressure and focal neurological signs, typically occurring more than 10 years after radiation therapy in the range of 5000 to 6000 cGy. Cerebral atrophy with increased ventricular size, widened sulci, areas of hypodensity or hyperintensity, and focal calcifications can be seen years later on neuroimaging.
8The purpose of this report is to alert psychiatrists and other physicians to the risk of psychosis following the treatment of brain tumors in children and adolescents.
METHOD
We reviewed psychiatric consultations on patients who were treated for intracranial malignancies at Childrens Hospital Los Angeles from April 16, 1991 through December 31, 2000, to identify patients with psychosis. From this group, we separated patients found to be persistently psychotic from those with delirium or brief psychotic symptoms. Their clinical presentation and course were summarized, noting type and original location and spread of the neoplasm, surgical procedures, radiation therapy, chemotherapy, complications including ventriculomegaly and seizures, endocrine function, neuroimaging studies, neuropsychologic assessment, mental status examination, psychotropic medication and response. Data were analyzed and reported descriptively.
RESULTS
Childrens Hospital Los Angeles treated approximately 600 new patients with primary intracranial neoplasms from 1991 through 2000. On reviewing the psychiatric consultations done during this period, psychosis was found in 17 patients who had been treated for a primary intracranial malignancy. Nine patients with brief psychosis or delirium were excluded, and the remaining eight patients with persistent psychotic symptoms became the subject of this descriptive study.
There were two boys and six girls in the study group. They were 9 to 20 (mean=13.8 [SD=3.8], median=14 years) years old when psychosis was first diagnosed. They ranged in age from 11 months to 13 (mean=7.5 [SD 3.6], median=8) years old at the time of diagnosis of their brain tumor, and the interval between initial diagnosis and later onset of psychosis ranged from 2 to 12 years (mean=7 [SD=3.7], median=7). The correlation between age at diagnosis and age when psychosis was found at psychiatric consultation was 0.45.
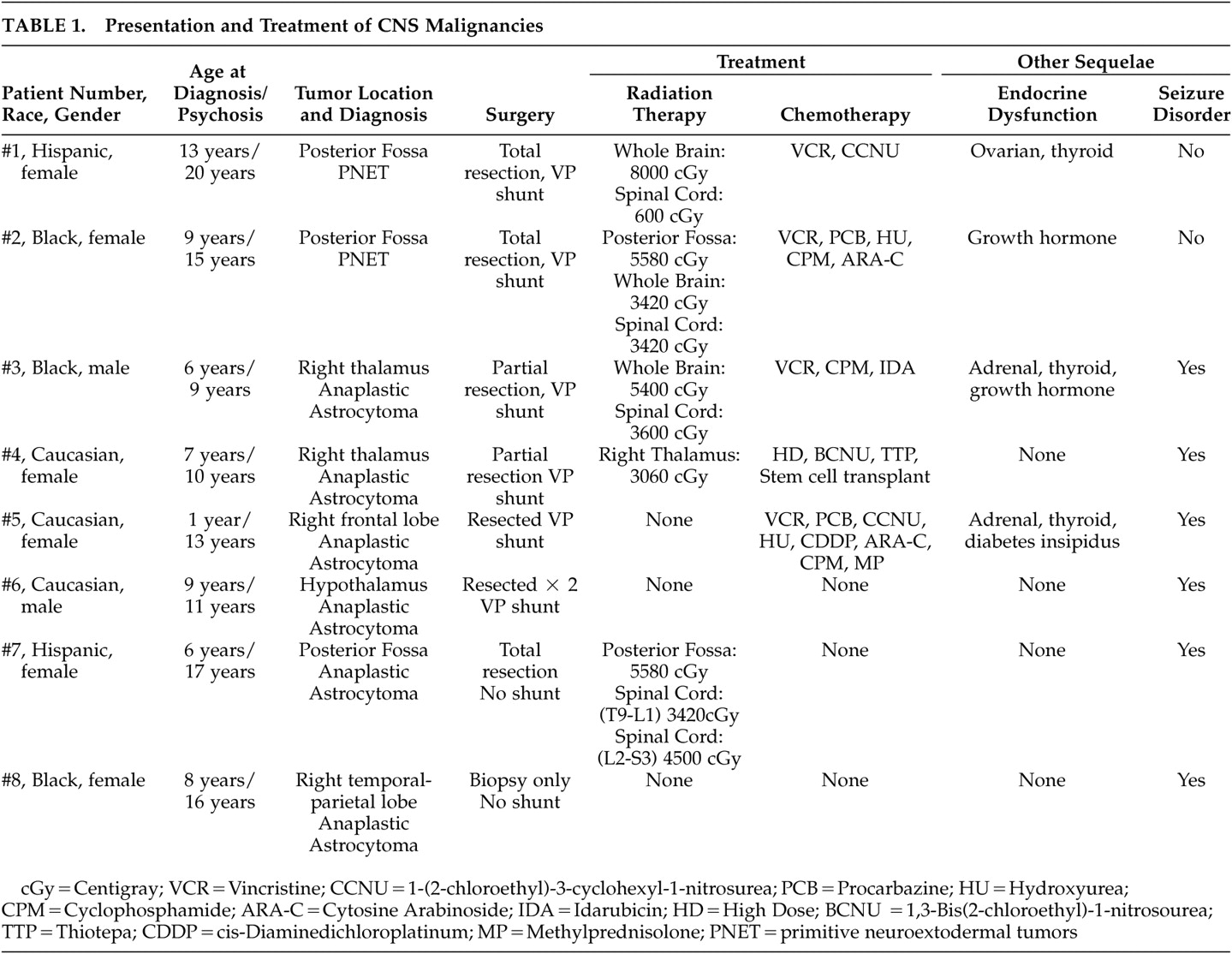
Six patients were diagnosed with an astrocytoma arising in the right thalamus, posterior fossa, optic chiasm, right frontal lobe, or right temporal-parietal lobe. The remaining two patients had primitive neuroectodermal tumors (medulloblastoma) arising in the posterior fossa (
Table 1 ).
Seven lesions were completely or partially surgically resected, and one patient had biopsy only. Four patients developed ventriculomegaly postoperatively and required ventriculo-peritoneal shunt, and one patient had a shunt placed for persistent headaches without ventriculomegaly. Four patients required hormone supplementation for hypopituitarism with thyroid hormone, adrenal corticoid, growth hormone, and antidiruetic hormone.
Four patients were treated postoperatively with both radiation and chemotherapy, two patients were treated with chemotherapy only, one patient received radiation only, and one was given neither radiation nor chemotherapy at parents’ request. The five patients treated with cranial radiation received between 3420 and 5400 cGy to the whole brain. The six patients who were treated with chemotherapeutic agents received different combinations of vincristine, BCNU (1,3-Bis(2-chloroethyl)-1-nitrosourea), cyclophosphamide, CCNU (1-(2-chloroethyl)-3-cyclohexyl-1-nitrosurea), procarbazine, hydroxyurea, cytosine arabinoside, idarubacin, and thiotepa. One patient underwent autologous bone marrow transplant.
Neuroimaging studies on six patients coincident with the onset of psychosis demonstrated diffuse, irregular, asymmetric focal calcifications, glial scars, and multiple small areas of necrosis and infarction.
Cognitive impairment was apparent in all eight patients, and mean IQ was in the borderline range. All patients were in special education, where their behavioral problems had become more disturbing and pronounced than their cognitive limitations. Two patients had a history of aggressive behavior.
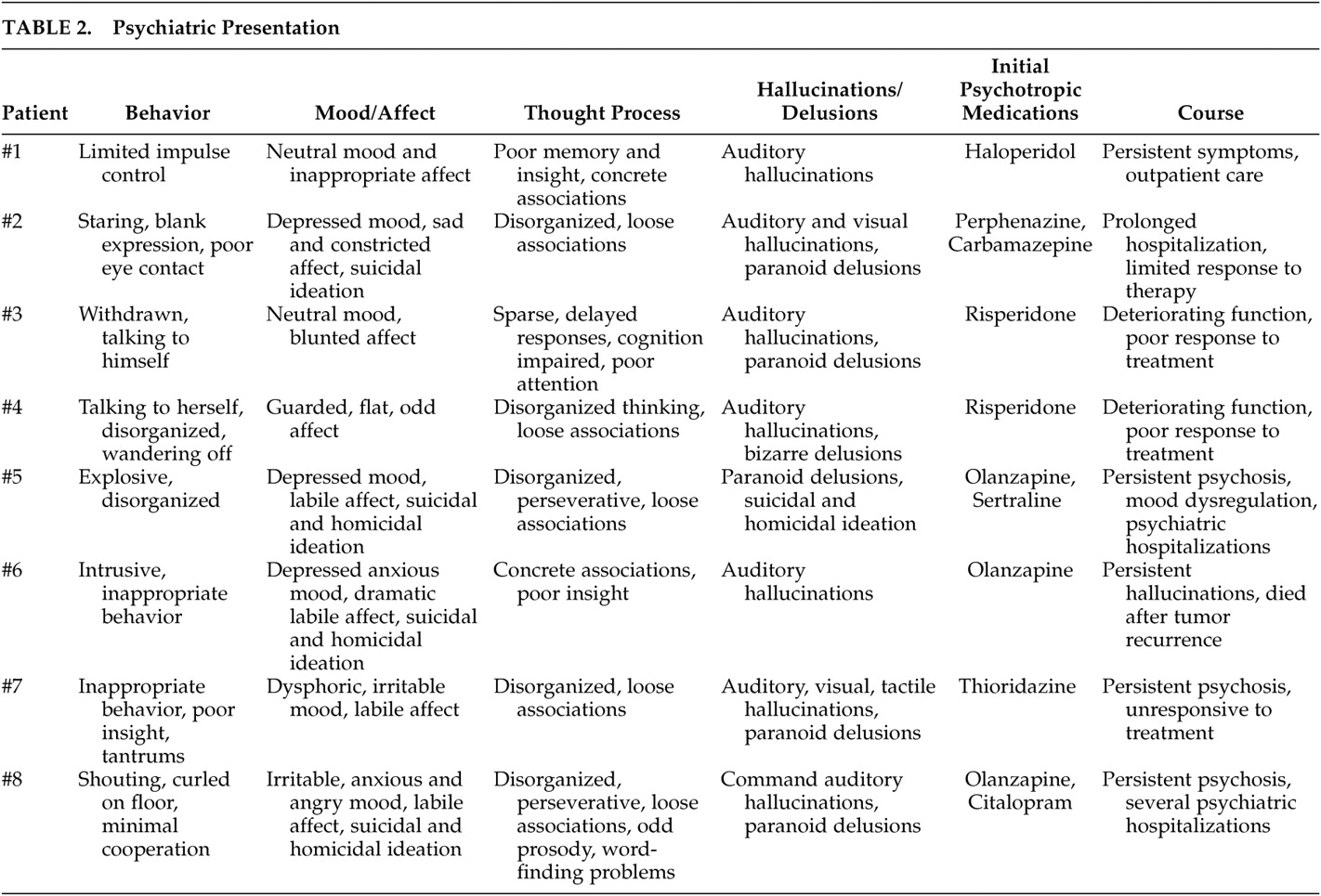
All patients behaved abnormally at the initial psychiatric evaluation, and only two were fully cooperative with the interview process. The patients were disorganized, impulsive, and bizarre, staring into space, talking to themselves, wandering off, or lying on the floor but were not hostile or aggressive at the time of initial interview (
Table 2 ).
The patients reported auditory, visual, and tactile hallucinations. Paranoid or bizarre delusions were noted in association with hallucinations, and one patient presented with paranoid delusional thinking without hallucinations. Memory and cognition were significantly impaired in all of the patients, and attention and concentration were limited. Disorganized thinking, confusion and loose associations were common. Suicidal and homicidal ideation were present in some, but none had attempted suicide.
All eight patients were treated with antipsychotic medications. Their response to medication has been limited, and psychotic symptoms persisted and progressed. In addition, antidepressant and mood-stabilizing medications were tried for associated mood symptoms with minimal benefit. Three patients required inpatient psychiatric hospitalization, either at initial evaluation or later in their course. All seven surviving patients have poor control of symptoms despite ongoing antipsychotic treatment. They remain significantly impaired, dependent on their families for support and close supervision, and continue to need intensive, ongoing psychiatric care.
DISCUSSION
Psychotic symptoms may be seen in association with infarction, tumors, or traumatic brain injury, and often a delay of several years may occur between the time of injury and onset of psychotic symptoms.
9 Intracranial neoplasms may present with psychosis, which often remits when the tumor is resected.
10 This is distinct from the onset of psychosis long after the tumor has been treated. In a comprehensive review of all psychiatric hospitalizations in Denmark, where patients with a history of malignancies in childhood could be identified and tracked, psychosis occurred in survivors of childhood intracranial malignancies at approximately the same rate (2.4%) as in our series (2.8%).
4Learning and cognition, which require the complex interplay of cortical, subcortical, and cerebellar circuits, are known to be impaired in survivors of childhood intracranial malignancies. Psychosis in these patients similarly may result from disruption in the circuits underlying sensory integration, memory and associative processes
11,
12 and critical injury to the limbic system and its extensive connections within the cortico-cerebellar-thalamic-cortical circuit.
13This series of pediatric patients represents a heterogeneous group, and due to small sample size, any association of late onset psychosis with tumor location, impact of surgery, treatment with radiation or chemotherapy could not be examined, and the mechanism of psychotic symptoms, bizarre behavior, mood dysfunction, hallucinations, and delusional thinking could not be determined. Nonetheless, as more children survive brain tumors, it is likely we will see more, serious psychiatric problems in this population as they age.