T he cerebellum has typically been associated with motor function, but case reports as far back as the mid-19th century suggest that the cerebellum has a role in nonmotor functions including personality, mood, and even psychosis.
1 The role of the cerebellum in both cognition and affect is not surprising. The cerebellum has connections with nonmotor cortical and subcortical areas associated with emotional processing, including the limbic system
2 and the prefrontal cortex.
3 The cerebellum also connects with brain stem nuclei, which supply the limbic system and cerebrum with serotonin, norepinephrine, and dopamine.
4 The nonmotor functions of the cerebellum include coordinating and monitoring errors in thought, similar to how it functions in motor control. The cognitive and affective symptoms following cerebellar dysfunction have been referred to as a “dysmetria of thought.”
5 The “dysmetria of thought” hypothesis has been postulated to explain symptoms in schizophrenia. Andreason and colleagues
6 offered that disruption of a cortical-thalamic-cerebellar circuit can lead to a “dysmetric cognitive state” that can account for cognitive, affective, and psychotic symptoms of schizophrenia. Evidence for disruption of cerebellar circuitry in schizophrenia comes from both structural and functional neuroimaging studies.
7,
8 Postmortem studies reveal smaller anterior portions of the vermis, as well as reduced size and density of Purkinje cells in the vermis, in patients with schizophrenia.
9,
10 Structural and functional abnormalities have also been described in depression
11,
12 and bipolar disorder.
13,
14Given the relationship between the cerebellum and cortical and subcortical areas and its potential role in psychiatric illness, it should follow that behavioral changes should be observable after cerebellar injury. Schmahmann and Sherman
15 examined the behavioral performance of 20 patients with cerebellar damage. Cerebellar pathology included cerebellar infarction (n=13), postinfectious cerebellitis (n=3), cerebellar cortical atrophy (n=3), and one patient with a resected cerebellar mass. Patients underwent neuropsychological testing and a bedside mental status examination. All patients displayed cognitive deficits. Difficulty modulating behavior and personality style was observed in 15 patients and characterized by flattened affect, disinhibition, and behavior described as “overfamiliarity, flamboyant and impulsive actions, and humorous but inappropriate and flippant comments.”
15 The behavioral symptoms were more pronounced in patients with lesions involving the vermis or paravermian regions. They named this constellation of symptoms the “cerebellar cognitive affective syndrome.” In this syndrome, cognitive impairments include deficits in executive functions, spatial cognition, and language. The affective component includes changes in personality, disinhibition, inappropriate behavior, altered regulation of mood, blunting of affect, obsessive compulsive tendencies, and psychotic thinking.
16 While influential in our understanding of the cognitive and affective functions of the cerebellum, the absence of a comparison group and the heterogeneity of the patient population in that pivotal study make it difficult to attribute the affective and cognitive observations to the cerebellum. The purpose of this review is to systematically and critically examine the controlled evidence for the presence of affective symptoms following cerebellar damage.
METHODS
We conducted a systematic literature review looking at the affective component of the cerebellar cognitive affective syndrome. We have included a wide array of emotion-related symptoms, going beyond the usual definition of affect, in keeping with Schmahmann’s
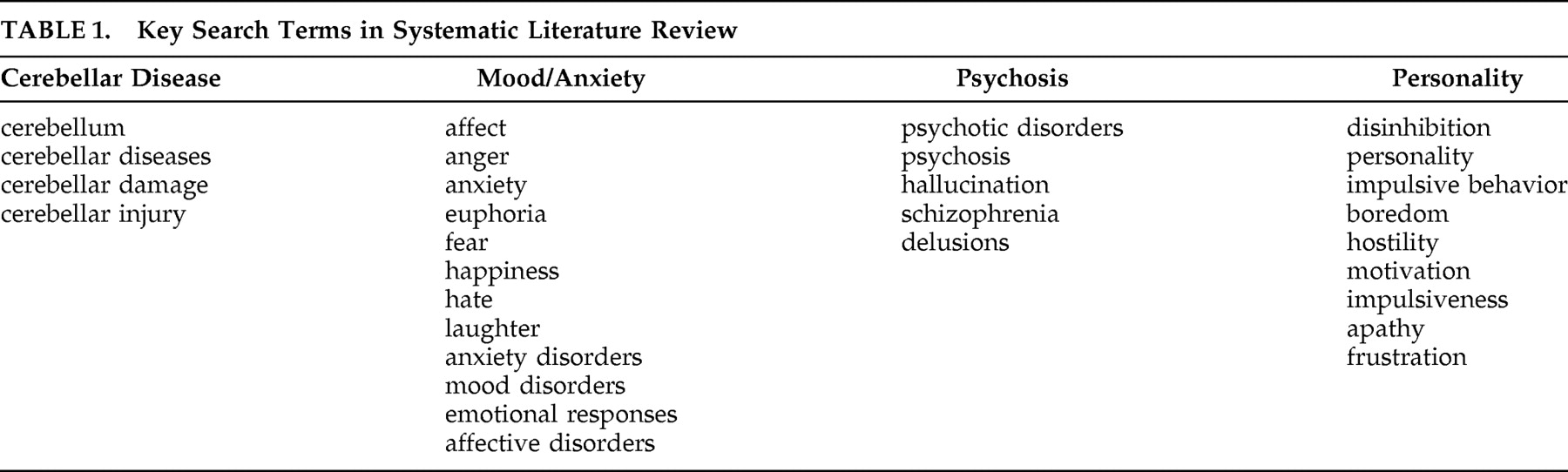
16 description of the affective component of the cerebellar cognitive affective syndrome. We included personality symptoms, psychosis, mood and anxiety symptoms, and disorders. In searching MEDLINE (1966–July 2006), Embase (1980–July 2006), and PsychINFO (1967–June 2006), we included terms relating to cerebellar pathology and the described affective component of the cerebellar cognitive affective syndrome (
Table 1 ).
Only articles relating to cerebellar pathology that included a comparison group were included in this review. Cerebellar pathology included any disease that primarily affects the cerebellum or patients with cerebellar lesions. Studies of patients with primary psychiatric diseases with no obvious cerebellar pathology and articles that did not relate to the described emotion-related symptoms were excluded. References in review articles, comments, and letters were reviewed for further relevant articles. Relevant articles from auto alerts up until May 2008 were also included.
The relevant studies were summarized in table form and critically reviewed. Furthermore, we selected studies that used comparable research measures of affective aspects of cerebellar cognitive affective syndrome. Where present, the raw data from each study were extracted and entered into RevMan 4.2 (Cochrane Collaboration, 2006) to calculate the standardized mean difference (SMD) of scores between patients with cerebellar pathology and the comparison group. Heterogeneity was estimated, and significance was assessed using χ
2 and I
2 . Outcomes were pooled with the random-effects meta-analytic model developed by Cochrane, which weights each study’s effect size by its sample size and by the between-study variance.
17RESULTS
We obtained 1,947 results. Of these, 1,678 were excluded because they did not discuss both cerebellar pathology and the described emotion-related symptoms. An additional 187 articles pertaining to primary psychiatric diseases with no obvious cerebellar pathology were also excluded. Twenty-four articles dealing with cerebellar lesions and 31 dealing with diseases that primarily affect the cerebellum were excluded for not having a non-cerebellar comparison group. References from 21 review articles, letters, and comments yielded three additional controlled studies. Updated autoalerts yielded two additional articles.
Eleven articles met inclusion criteria and are discussed in the following sections. They consisted of six studies of diseases primarily affecting the cerebellum and five studies of cerebellar lesions. All studies of diseases primarily affecting the cerebellum used populations with one or more forms of spinocerebellar ataxia.
Spinocerebellar Ataxias
The spinocerebellar ataxias are a heterogeneous group of disorders with clinical manifestations of predominantly, but not exclusively, cerebellar findings. They include a number of different disorders with varying inheritable patterns as well as sporadic forms.
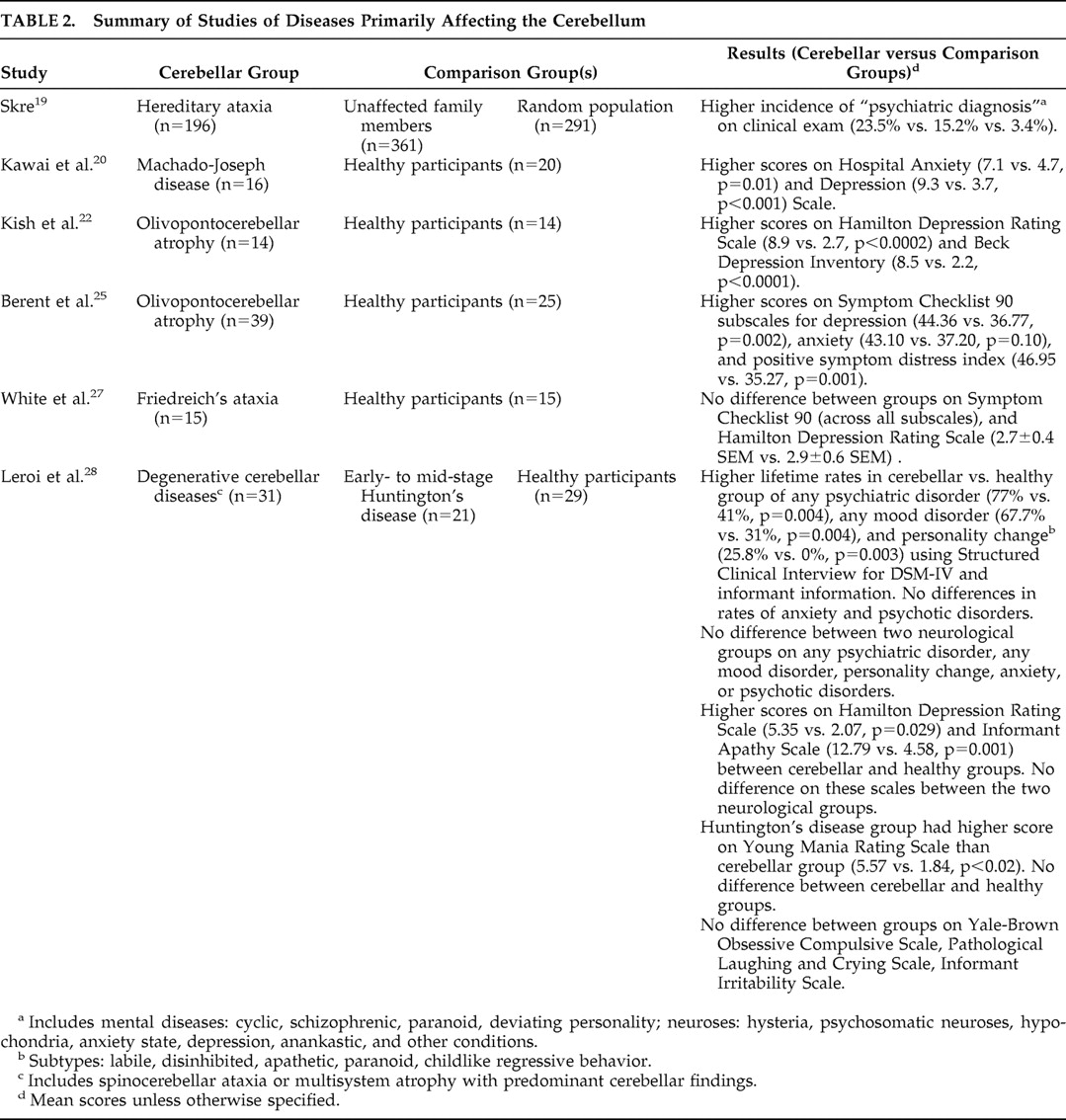
18 The subtypes of spinocerebellar ataxias that have been examined in the studies include hereditary ataxia, Machado-Joseph disease, olivopontocerebellar atrophy, Friedreich’s ataxia, and multisystem atrophy with predominant cerebellar findings. Details of the disease studies are summarized in
Table 2 .
Skre
19 found individuals with hereditary ataxia had a higher incidence of having a psychiatric diagnosis than unaffected family members and a healthy comparison group. Psychiatric diagnoses were based on clinical examination, specific diagnoses were not reported, and no standardized measures were used.
In contrast to Skre, the other five studies used standardized measures and found higher depression and anxiety scores on a number of measures. Kawai et al.
20 found that patients with Machado-Joseph disease had significantly higher mean subscores of both depression and anxiety on the Hospital Anxiety and Depression Scale
21 than those in a healthy comparison group. Kish et al.
22 found that patients with olivopontocerebellar atrophy had higher scores on both the Hamilton Depression Rating Scale (HAM-D)
23 and the Beck Depression Inventory (BDI)
24 than those in a healthy comparison group. Berent et al.
25 found olivopontocerebellar atrophy patients rated themselves as being significantly more depressed, anxious, and in greater general distress on the Symptom Checklist 90 (SCL-90)
26 than those in a healthy comparison group. The clinical significance of these results is uncertain since the scores in these latter two studies were fairly low in both groups.
In contrast to the previous studies, White et al.
27 observed no between-group difference on the SCL-90 (across all subscales) or HAM-D in patients with Friedreich’s ataxia relative to a healthy comparison group. However, standard deviations, statistical comparison, and total HAM-D scores were not reported. Five patients were observed to be “inappropriately jocular” during and between testing; however, no standardized testing was used to quantify this observation.
The previous studies all used healthy comparison groups. In the Kish et al.
22 study, severity of depression was not associated with cognitive impairment. However, the other studies did not address the possible impact of cognitive or physical symptoms or having a neurological illness on emotional symptoms.
This limitation is partially addressed by Leroi et al.
28 by using more than one comparison group. In this study, patients with degenerative cerebellar diseases were compared to patients with early- to mid-stage Huntington’s disease in addition to a healthy comparison group. The authors reported significant differences between the group with cerebellar pathology and the healthy participants in lifetime rates of any psychiatric disorder, any mood disorder, and personality change based on a psychiatric interview using the Structured Clinical Interview for DSM-IV (SCID) and informant information. There were no statistically significant differences in rates of anxiety or psychotic disorders between the cerebellar and healthy comparison groups. Cross-sectional measures of current psychopathology showed significant differences between the cerebellar and healthy comparison subjects on the HAM-D and an informant rating scale for apathy.
29 The only differences between the two neurological groups was on the Young Mania Rating scale
30 in which the Huntington’s group scored higher than the cerebellar pathology group. It should be noted that bipolar disorder or mania was not seen in any of the patients in the cerebellar pathology or healthy groups, but was diagnosed in one patient in the Huntington’s group using the SCID. The similarity of the two neurological groups is interesting since Huntington’s disease is associated with severe psychopathology with relative sparing of the cerebellum.
31Cerebellar Lesions
While the cerebellum appears significantly affected in the spinocerebellar ataxias, this heterogeneous group of disorders may also affect other cortical and subcortical areas relevant to “affective” symptoms.
32 Studying patients with specific cerebellar lesions may more accurately implicate the cerebellum’s involvement with behavioral and affective symptoms. Indeed, some recent research in patients with focal cerebellar lesions has shed light on the role of the cerebellum in specific aspects of cognition.
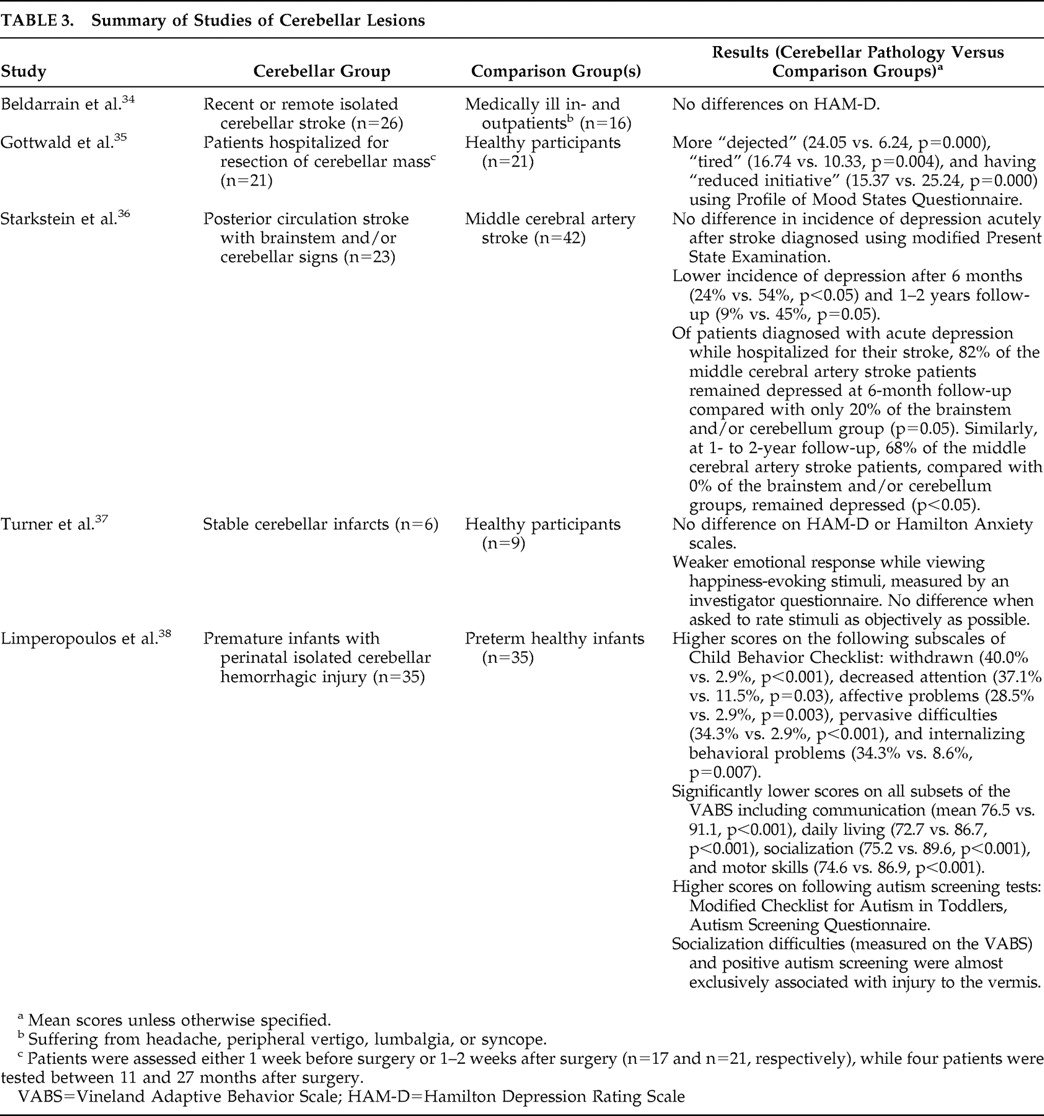
33 Details of lesion studies are summarized in
Table 3 .
Beldarrain et al.
34 assessed a group of patients who had either a recent (within 3 weeks) or remote (at least 6 months prior to assessment) history of cerebellar stroke. Patients with extracerebellar lesions on MRI were excluded. These were compared to hospital in- and outpatients suffering from headache, peripheral vertigo, lower back pain, or syncope, matched for age, gender, and education, and without cognitive impairment. The authors reported no differences between groups on the HAM-D, but scores and statistical analysis were not reported. The possible impact of a medically ill comparison group on the lack of between-group differences on the HAM-D was not assessed.
Gottwald et al.
35 compared a group of healthy participants to a group of patients hospitalized for resection of cerebellar lesions (tumors and hematomas). The affective state of participants was assessed using a German version of the Profile of Mood States questionnaire (POMS).
39 Most patients were assessed either soon before surgery or soon after surgery. Patients described themselves as significantly more “dejected,” “tired,” and having “reduced initiative” relative to the healthy comparison group. However, as the authors acknowledge, the effect of being hospitalized, being recently diagnosed, or having either imminent or recent neurosurgery on affect was not assessed.
Starkstein et al.
36 looked at 71 consecutive patients admitted for an acute thromboembolic infarct. Patients were divided into those with posterior circulation and middle cerebral artery infarcts. Sixty-two percent of the posterior circulation infarct patients (n=23) had brainstem and/or cerebellar signs. However, only 39% of these (n=9) had cerebellar lesions on CT scan or neurological exam. There was no significant difference between posterior circulation and middle cerebral artery infarct groups in the incidence of depression. Depression was diagnosed based on symptoms elicited by the modified Present State Examination (PSE).
40 Symptoms were converted to DSM-III criteria for either major depression or dysthymic (minor) depression. A subgroup of patients in the posterior circulation infarct group with brainstem and/or cerebellar infarct showed significantly lower rates of depression compared to the middle cerebral artery infarct group after 6 months and at 1–2 years follow-up after stroke. No significant difference was found acutely after the stroke. Of the patients diagnosed with acute depression while hospitalized for their stroke, a greater percentage of middle cerebral artery infarct patients remained depressed at 6 months and 1–2 years later compared to the brainstem/cerebellar pathology group. It should be noted that the brainstem/cerebellar pathology group contained some patients with only brainstem lesions as well as patients with both brainstem and cerebellar lesions; therefore differences cannot be attributed specifically to the cerebellum.
Turner et al.
37 found that cerebellar stroke patients experienced a weaker emotional response while viewing happiness-evoking stimuli relative to a healthy comparison group. However, when asked to rate the stimuli as objectively as possible (as opposed to their personal emotional response), there were no differences between the groups. Differences in how the groups processed frightening stimuli on a functional neuroimaging level were also observed. While interesting theoretically, the clinical significance of this is questionable. In fact, there were no differences in both groups on the HAM-D or Hamilton Anxiety Scale.
41Limperopoulos et al.
38 found more frequent caregiver-reported behavioral problems, socialization difficulties, and higher scores on autism screening tests in children with cerebellar damage in the perinatal period compared to a group of healthy preterm infants. Longer term outcomes of this population and specific affective measures were not utilized in this study.
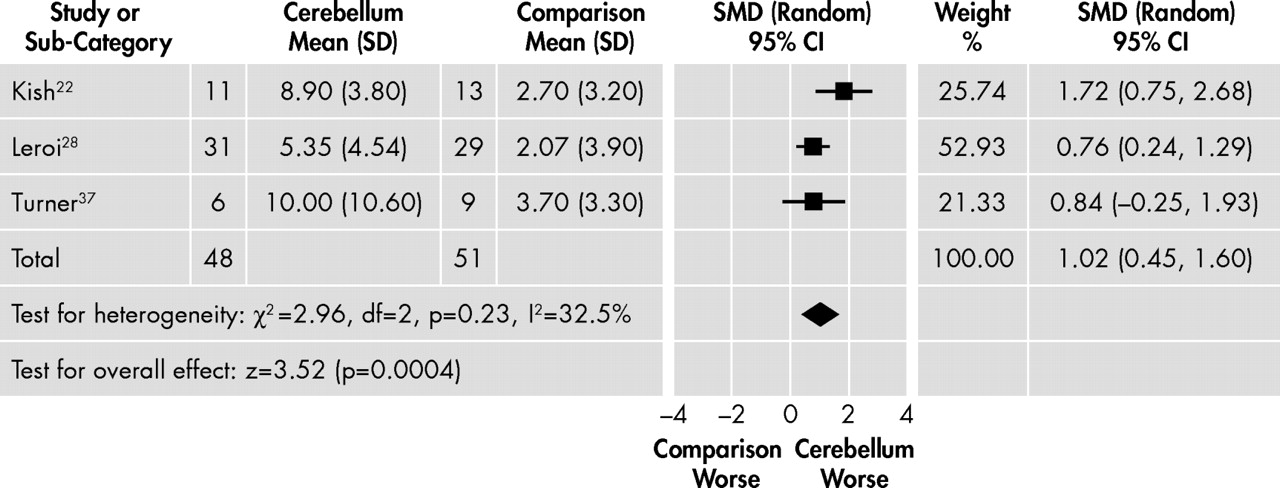
Meta-Analysis
Only one outcome variable, the HAM-D, was reported in more than one study. Means and standard deviation for the full-scale HAM-D were not available in two of the studies
27,
34 even after the authors were contacted directly. Another study utilized the HAM-D but did not incorporate a healthy comparison group.
36 We pooled the results of the three studies assessing depression with the HAM-D in cerebellar diseases that had data available.
22,
28,
37 These studies were homogeneous (χ
2 =2.96, df=2, p=0.23, I
2 =32.5%), and patients with cerebellar diseases had higher HAM-D scores (standardized mean difference=1.02, 95% CI=0.45–1.60, p=0.0004;
Figure 1 ). However, the clinical significance of this modest difference remains uncertain especially since the two studies excluded from the meta-analysis
27,
34 for lack of data availability reported negative findings. Additionally, the studies included heterogeneous populations.
DISCUSSION
In the current systematic review of the affective component of the cerebellar cognitive affective syndrome, we focused on studies of patients with cerebellar pathology relative to non-cerebellar comparison groups. We reviewed five studies of populations with spinocerebellar ataxia that used standardized measures. Cerebellar pathology patients had higher depressive and anxiety scores on a number of different self-report and observer report measures in some
22,
25,
28 but not all
27 of these studies. Apathy and personality changes were reported in one study.
28We also reviewed five studies of patients with cerebellar lesions. Two studies
34,
37 revealed no difference on depression or anxiety scores (using HAM-D and the Hamilton Anxiety Scale) in patients with cerebellar lesions relative to a healthy comparison group, but hospitalized patients in one study
35 indicated more depressive symptoms on the Profile of Mood States questionnaire relative to the healthy participants. The rate and course of depression was different in a group of patients that had either brainstem or cerebellar strokes compared to middle cerebral artery strokes.
36 Cerebellar stroke patients differed in their emotional response relative to a healthy comparison group.
37 Infants with cerebellar damage sustained perinatally had more behavioral problems, socialization difficulties, and higher scores on autism screening tests than healthy preterm infants.
38 Pooling of the three studies with available HAM-D scores revealed statistically significant but modestly higher depressive scores in patients with cerebellar diseases relative to healthy comparison groups in the present analysis.
We have highlighted the tentative evidence supporting the role of the cerebellum in the affective syndrome in patients with cerebellar damage. This is consistent with the many case reports that report affective symptoms in patients with cerebellar pathology. These case reports describe a wide range of mood and anxiety symptoms including depression,
42,
43 anxiety,
44,
45 lack of emotions,
46 and affect dysregulation.
5,
47 Psychotic symptoms and personality changes also described in the literature include delusions,
48 paranoid ideations,
49 hallucination,
50 apathy,
42 disinhibition,
5 irritability,
51 and “personality change.”
50We have also highlighted some limitations to the few available studies utilizing a comparison group with no cerebellar pathology. The limited evidence is particularly notable, especially those reports evaluating patients with isolated cerebellar lesions that provide the most direct correlation to the cerebellum. Future studies should address the lack of emotion-related symptoms generally observed in clinical practice in relation to cerebellar damage by focusing on specific anatomical locations of lesions within the cerebellum that may lead to affective symptoms. There is some evidence that the vermis is important in this regard.
5 This is not surprising given its extensive connectivity with the limbic system,
2 a network in the brain responsible for emotion formation and regulation. It is also necessary to use standardized and sensitive measures to detect possibly subtle changes in affect or behavior that may not reach threshold for a specific psychiatric diagnosis. Comparison groups must also be matched for severity of physical and cognitive impairment. This is a challenge if healthy comparison groups are used, given the comorbid functional and cognitive sequelae of neurological illness and specifically cerebellar disease. These limitations need to be addressed either by controlling for these aforementioned factors or using a more parallel comparison group such as patients with other diseases or other brain lesions.
Cerebellar damage is associated with dysmetric symptoms including difficulty coordinating movement, instability of gait, impairment of articulation, and difficulty with eye movement and swallowing.
16 While one may hypothesize an increased prevalence of emotional symptoms in these patients, consistent with a “dysmetria of emotion,”
5 the evidence for this is currently limited. This hypothesis needs to be addressed in the future with well-designed cohort studies with a comparison group with no cerebellar pathology to adequately evaluate the affective component of the cerebellar cognitive affective syndrome.
Acknowledgments
Preliminary results were presented at the annual meeting of the American Neuropsychiatric Association in Tucson, AZ, February 17–20, 2007.