Major depressive disorder (MDD) may occur before the development of neurological symptoms in multiple sclerosis (MS).
1–4 Studies have reported high rates of depression in MS, and rates of MDD are two times more prevalent in patients with MS when compared with other chronic illnesses, including other neurological disorders.
5,6 Comorbid MDD and MS has been associated with a lower quality of life and increased risk of suicidal ideation.
7 Psychiatric and medical comorbidity has also been associated with delays in MS diagnosis and greater disability at time of diagnosis.
8 Neuroimaging data reveal an association between low mood and structural and functional brain abnormalities, suggesting that depression in MS may arise directly from the demyelination process and be of a different etiology than in non-MS patients.
9,10 Despite the clinical significance,
7 previous studies have not examined whether MDD occurs before neurological symptoms in MS.
The purpose of this study is to explore whether subjects with MS report symptoms of depression that occur before the development of neurological MS. We examined the prevalence and severity of depression in subjects diagnosed with MS before and after onset of MS and whether depression severity is associated with more lesions on MRI. We addressed the following questions: 1) What is the prevalence of MDD in MS? 2) Does MDD occur before the onset of neurological symptoms in multiple sclerosis? 3) Is there a correlation between severity of depression and brain lesions on magnetic resonance imaging (MRI)?
METHOD
Standard Protocol Approvals, Registrations, and Patient Consents
The protocol received approval from the University of Massachusetts Medical Center Institutional Review Board, an ethical standards committee on human experimentation. Written informed consent was obtained from all patients participating in the study after the procedures had been explained. The inclusion criterion was a clinically definite diagnosis of MS. Subjects with active substance abuse, defined as 1 month prior to enrollment, or those having a psychotic disorder were excluded.
Data Collection
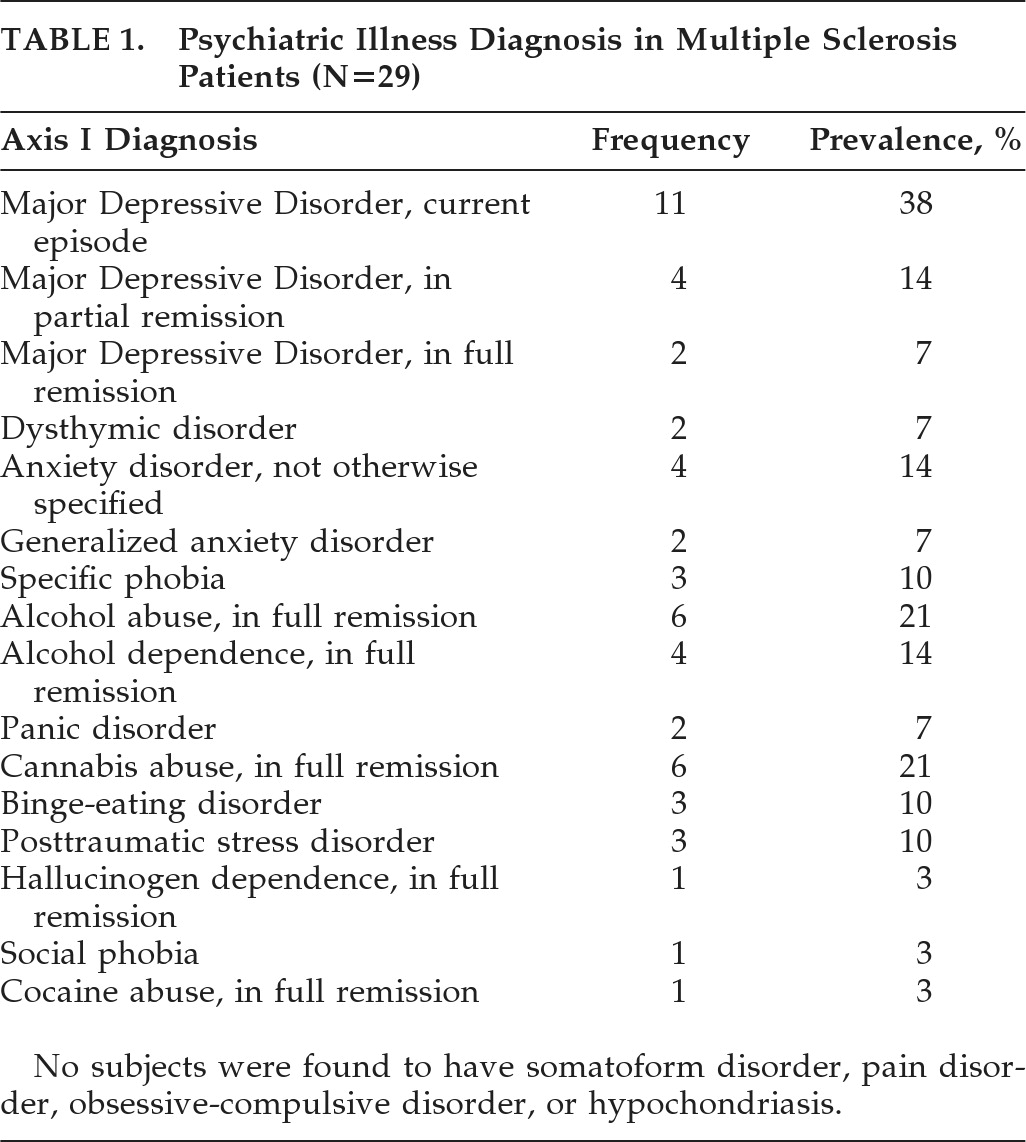
Thirty subjects between the ages of 19 and 65 with clinically definite MS with or without a past psychiatric history of depression were enrolled and provided written informed consent to participate in the study. Disease and demographic characteristics were noted (
Table 1), and subjects were assessed with the following psychiatric battery: 1) In order to establish a diagnosis of MDD, subjects were interviewed with the Structured Clinical Interview for DSM-IV-TR (SCID); 2) In subjects with a current or premorbid (before onset of MS) history of mental illness, details about the timeline were obtained, including the number of months before onset of physical symptoms of MS the depression symptoms occurred and whether the subject experienced a delay in MS diagnosis; 3) A subjective index of depression was obtained with the Beck Depression Inventory (BDI); fatigue, with the Fatigue Severity Scale (FSS); quality of life (Short-Form Health Survey [SF-36]); and physical and psychological impact of MS (Multiple Sclerosis Impact Scale [MSIS-29]); 4) Details of medical and psychiatric history, family history of mental illness, start date of current depressive episode, number of previous depressive episodes, and current and past treatments, were obtained from subjects. Approximately two to three subjects were enrolled each month from July 2006 until June 2007.
Patient Selection
Thirty subjects were recruited, all of whom were diagnosed with definite MS before entry by MRI and/or lab results and/or clinical exam. Of these subjects, one patient was withdrawn secondary to active substance abuse, and six subjects were not included in the imaging data because the MRI tests were unavailable. MRIs were independently reviewed by two MS experts experienced in MRI interpretation. T2WI lesion volume, T1WI hypointense lesion number, Gd+-enhancing lesion number, and cerebral atrophy were categorized by two MS experts as None, Mild, Moderate, or Severe for each outcome. Each atrophy scale category (None, Mild, Moderate, or Severe) was converted to a numerical value for statistical analyses. MDD occurring before neurological MS was defined as a major depressive episode (MDE) occurring 6 months to 1 year before onset of neurological symptoms of MS.
Statistical Analysis
Analysis of the data was performed with SAS Version 9.1 (SAS Institute, Cary, NC). Because of the limited sample size, the analyses focused on descriptive statistics and nonparametric methods. Although demographic data were collected, sample size was not sufficient for subgroup analyses.
RESULTS
Subjects enrolled had a mean age of 43 years; 21 of the 26 subjects enrolled were women, and 8 were men. Subjects had been diagnosed with MS at a mean age of 38. Fisher's exact test was performed, and no statistically significant relationship was found between prevalence of depression and family history of psychiatric illness.
Subjects had a history of MS for a mean of 5 (SD: 5.22) years. Four subjects reported a Major Depressive Episode (MDE) occurring as a prodrome to MS, with a mean onset of 0.5 (SD: 0.35) years before onset of neurological symptoms. Three subjects in which MDE occurred as a prodrome reported a mean 1.2-year (SD: 0.29) delay in MS diagnosis as a result of physical symptoms' being attributed to depression.
As severity of depression increased, as determined by BDI scores, atrophy on MRI increased (Spearman correlation coefficient (ρ)=0.52, p=0.01). The number of gadolinium-enhancing lesions and T1WI hypointense foci (“black holes”) did not reveal a significant correlation with depression symptom severity.
Severity of depression (BDI) correlated significantly with the psychological impact of MS (MSIS-29; Spearman correlation coefficient: ρ=0.63, p=0.012). Severity of depression (BDI) correlated significantly with physical impact of MS (MSIS-29; Spearman correlation coefficient: ρ=0.75, p=0.0013). Severity of depression (BDI) was not significantly correlated with physical functioning (SF-36; Spearman correlation coefficient: ρ=0.41, p=0.13), but approached significance. Borderline significance was found in the correlations of severity of depression (BDI) with energy and fatigue (SF-36; Spearman ρ=0.43, p=0.11), and severity of depression (BDI) with fatigue severity (FSS; Spearman ρ=0.45, p=0.10). Other SF-36 and FSS measures were not correlated significantly with depression severity (BDI).
No statistically significant relationship was found (by Fisher's exact test) between prevalence of depression and family history of psychiatric illness. Presence of major depression and MS was not related to a family history of psychiatric illness.
DISCUSSION
These findings are consistent with other studies that report high rates of MDD in MS. In this study, we found that 15% of subjects reported an MDE that occurred before the onset of neurological MS symptoms. Also, we found that 75% of subjects reported a delay in MS diagnosis secondary to MDD. MDD may occur not only before neurological MS symptoms, but it may also delay the diagnosis of MS. Such a delay is clinically significant because it may result in delayed treatment, increased disease burden, and disability and lower quality of life. Importantly, the rates of other psychiatric diagnoses were similar to that of the general population, supporting a specific association between depression and MS. Our study also replicates the association between depression and cerebral atrophy in MS patients noted by previous authors.
10The study has several limitations beyond the limited sample size. The high prevalence of depression in subjects may be secondary to the increased likelihood of participation in the study in patients with a history of depression. Several subjects were excluded because of unavailable MRI data at the time of data collection, which may confound the data. The wide range of disease durations at the time of neuroimaging may have confounded the findings, given that disease duration may be an important influence on variables such as atrophy and lesion burden.
Often, MS presents a diagnosis and treatment dilemma when psychiatric symptoms precede the onset of neurologic symptoms or when comorbid psychiatric and neurologic symptoms are present. Patients presenting with unexplained neurological symptoms in the context of depression should be further investigated in order to capture MS at an earlier stage. Optimal care requires an increased awareness of psychiatric comorbidity in order to maintain objectivity and awareness during treatment. Future studies are needed to further characterize neuropsychiatric presentations of MS and develop criteria for selecting patients in which imaging and lab work are indicated.
Acknowledgments
This study is not industry-sponsored. Dr. Nancy Byatt reports no disclosures. Dr. Anthony Rothschild has received grants or funding from NIMH, Cyberonics, Takeda, and Wyeth, and has been a consultant for Pfizer, GlaxoSmithKline, Forest Laboratories, and Eli Lilly. He has received royalties from the Rothschild Scale for Antidepressant Tachyphylaxis (RSAT),TM and American Psychiatric Press, Inc. for Clinical Manual for Diagnosis and Treatment of Psychotic Depression, Evidence-Based Guide to Antipsychotic Medications. Dr. Peter Riskind has received honoraria and/or has consulted for Biogen Idec, and Teva Neurosciences. Dr. Carolina Ionete has consulted for Biogen Idec, TEVA, Serono, and Bayer. Dr. Anne Hunt reports no disclosures.