The children of mothers exposed to genital/reproductive infections in the months surrounding conception have an increased risk of developing schizophrenia, according to a new report from the Prenatal Determinants of Schizophrenia (PDS) study.
The study requires replication but adds to accumulating evidence that the origins of schizophrenia may lie in events occurring during gestation. It appears in the May American Journal of Psychiatry.
The PDS study has already explored associations between prenatal influenza, toxoplasmosis, and rubella and later incidence of schizophrenia.
“More important than any individual study is the gestalt that comes out of this line of research,” Mark Opler, Ph.D., a research scientist in the Department of Epidemiology at Columbia University, told Psychiatric News. Opler has conducted studies of prenatal lead exposure as a possible cause of schizophrenia and has collaborated with some of the co-authors of the current study.
“There is emerging a strong body of evidence showing that perturbation of some kind definitely affects the risk on the incidence of disorders in midlife,” he said.
Vicki Babulas, M.P.H., and colleagues examined data from the Child Health and Development Study, which enrolled 7,794 women from the Kaiser Permanente Medical Care Plan in Alameda, Calif., between 1959 and 1966. Researchers such as Jacob Yerushalmy, founder of the Child Health and Development Study, took a long view and set up the organizations and systems to do studies decades into the future.
Checking obstetric and medical records, Babulas and colleagues noted diagnoses of endometritis, cervicitis, pelvic inflammatory disease, vaginitis, syphilis, condylomata, or “venereal disease” in the women they studied. They diagnosed 71 cases of schizophrenia spectrum disorder, either using the Diagnostic Interview for Genetic Studies (44) and/or chart review (27).
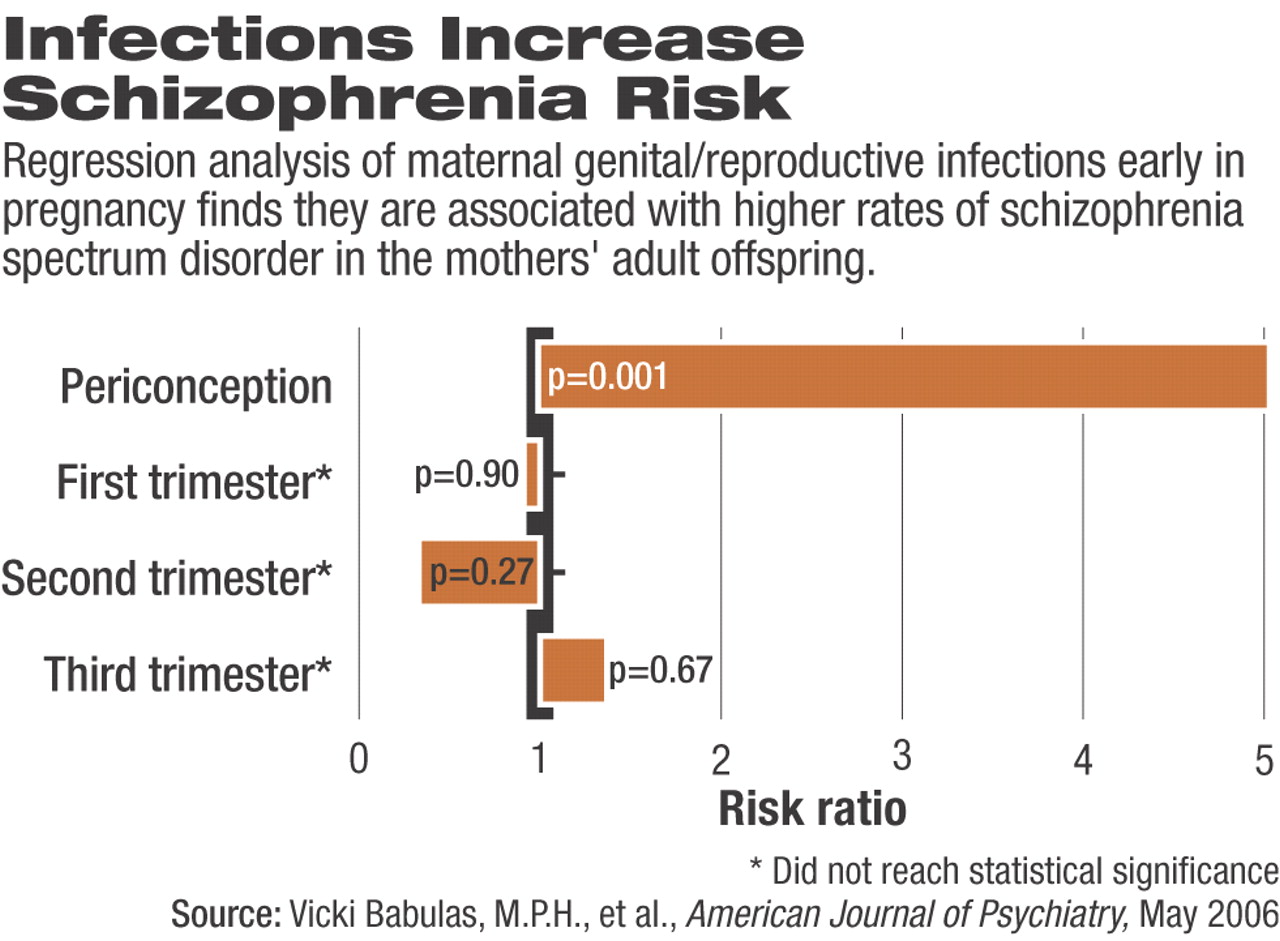
Children of women exposed to genital or reproductive infections during periconception (from 30 days before the last menstrual period to 30 days after the last period) had a five times greater chance of developing schizophrenia than unexposed control children. Results were adjusted for maternal race, education, age, and mental illness.
The timing of infection appeared significant. Exposure in the first trimester after the periconceptual period or in the second or third trimester produced no such association, wrote Babulas and colleagues.
“It's not just the exposure, but the timing of the exposure,” said Opler. Infections might have different effects if they occur at different times in the pregnancy, he said. If researchers knew the effects that biological agents had at specific stages of development, they could know what systems were likely to be affected at critical points and eventually link etiology with symptoms.
Babulas and colleagues suggested that the effects on the fetus of such infections are biologically plausible. Pathogens for genital or reproductive infections might ascend from the perineum, vagina, or cervix to infect the fetus directly, they wrote. “Alternatively, the pathogenic organism may be transmitted by traversing the placental tissues, gaining access to the fetal bloodstream, and crossing into the developing brain.”
The study is limited by the low numbers of cases exposed to genital/reproductive infections in the womb (five), a lack of serological confirmation of infection, and a definition of infection that includes a number of different microbes. Like previous PDS reports, this study used maternal serum immune markers, not data from inside the fetal compartment.
Nonetheless, the study is bolstered by use of prospective diagnosis and documentation of the mothers' infections and by face-to-face assessments of schizophrenia spectrum disorder.
“We're still in the early stages of studying these effects, but in 10 years [the research has] produced groundbreaking results,” said Opler.